Protocols for Anticoagulant and Thrombolytic Therapy Mar 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Enoxaparin Sodium Solution for Injection, Manufacturer's Standard
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION PrLOVENOX® Enoxaparin sodium solution for injection 30 mg in 0.3 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 40 mg in 0.4 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 60 mg in 0.6 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 80 mg in 0.8 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 100 mg in 1 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 300 mg in 3 mL solution (100 mg/mL), multidose vials for subcutaneous or intravenous injection PrLOVENOX® HP Enoxaparin sodium (High Potency) solution for injection 120 mg in 0.8 mL solution (150 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 150 mg in 1 mL solution (150 mg/mL), pre-filled syringes for subcutaneous or intravenous injection Manufacturer’s standard Anticoagulant/Antithrombotic Agent ATC Code: B01AB05 Product Monograph – LOVENOX (enoxaparin) Page 1 of 113 sanofi-aventis Canada Inc. Date of Initial Approval: 2905 Place Louis-R.-Renaud February 9, 1993 Laval, Quebec H7V 0A3 Date of Revision September 7, 2021 Submission Control Number: 252514 s-a version 15.0 dated September 7, 2021 Product Monograph – LOVENOX (enoxaparin) Page 2 of 113 TABLE OF CONTENTS Sections or subsections that are not applicable at the time of authorization are not listed. TABLE OF CONTENTS .............................................................................................................. -
Clinical Protocol
CLINICAL PROTOCOL Subject: Page Protocol # EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND 1 of 4 NMH CCP 07.0024 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL ANTICOAGULANTS Version: 1.0 Title: Revision of: Effective Date: EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND NEW 04/29/2013 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL Removal Date: ANTICOAGULANT APIXABAN (ELIQUIS) I. PURPOSE: To standardize management of patients with bleeding and clotting emergencies who are taking novel oral anticoagulants (NOACs). This protocol covers emergent reversal and ischemic stroke in patients on apixaban (Eliquis) therapy. II. CLINICAL PROTOCOL: A. The NOAC apixaban (Eliquis) is FDA approved for stroke prevention in patients with atrial fibrillation. This agent presents clinicians with several challenges because there are no specific antidotes, and no readily available quantitative assay to determine the degree of anticoagulation in a patient on this therapy. B. Patients taking this agent are likely to present to the hospital with; 1. life-threatening bleeding (e.g., intracerebral hemorrhage or GI bleeding), or a need for an emergent invasive procedure (surgery, cardiac Catherization) 2. acute ischemic stroke. The administration of tissue plasminogen activator (IV tPA) in the setting of NOAC use is potentially dangerous. C. There are no accepted evidence-based guidelines for managing these situations. This protocol is a consensus of clinicians from stroke, neurology, neurosurgery, hematology, neurocritical care, laboratory medicine, cardiology, and pharmacy. III. REVERSAL PROTOCOL FOR PATIENTS WITH SEVERE/LIFE-THREATENING BLEEDING TAKING APIXABAN (ELIQUIS) A. Inclusion criteria: 1. Patient has taken any dose of apixaban within last 48 hours. a. If time of last dose is unknown, but patient is suspected of having taken apixaban in last 48 hours, and PT is abnormal and 2. -

The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’S Perspective
International Journal of Molecular Sciences Review The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’s Perspective Hau C. Kwaan 1,* and Paul F. Lindholm 2 1 Division of Hematology/Oncology, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA 2 Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; [email protected] * Correspondence: [email protected] Abstract: The novel coronavirus disease (COVID-19) has many characteristics common to those in two other coronavirus acute respiratory diseases, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). They are all highly contagious and have severe pulmonary complications. Clinically, patients with COVID-19 run a rapidly progressive course of an acute respiratory tract infection with fever, sore throat, cough, headache and fatigue, complicated by severe pneumonia often leading to acute respiratory distress syndrome (ARDS). The infection also involves other organs throughout the body. In all three viral illnesses, the fibrinolytic system plays an active role in each phase of the pathogenesis. During transmission, the renin-aldosterone- angiotensin-system (RAAS) is involved with the spike protein of SARS-CoV-2, attaching to its natural receptor angiotensin-converting enzyme 2 (ACE 2) in host cells. Both tissue plasminogen activator (tPA) and plasminogen activator inhibitor 1 (PAI-1) are closely linked to the RAAS. In lesions in the lung, kidney and other organs, the two plasminogen activators urokinase-type plasminogen activator (uPA) and tissue plasminogen activator (tPA), along with their inhibitor, plasminogen activator 1 (PAI-1), are involved. The altered fibrinolytic balance enables the development of a hypercoagulable Citation: Kwaan, H.C.; Lindholm, state. -

Rtpa) for the Treatment of Hepatic Veno-Occlusive Disease (VOD
Bone Marrow Transplantation, (1999) 23, 803–807 1999 Stockton Press All rights reserved 0268–3369/99 $12.00 http://www.stockton-press.co.uk/bmt Recombinant tissue plasminogen activator (rtPA) for the treatment of hepatic veno-occlusive disease (VOD) S Kulkarni1, M Rodriguez2, A Lafuente2, P Mateos2, J Mehta1, S Singhal1, R Saso3, D Tait4, JG Treleaven3 and RL Powles1 Departments of 1Medical Oncology, 3Haematology and 4Radiotherapy, Royal Marsden NHS Trust, Sutton, Surrey, UK; and 2Haematology Department, Hospital La Paz, Madrid, Spain Summary: clinical syndrome characterized by hyperbilirubinemia, hepatomegaly and fluid retention,2,3 and results from dam- Seventeen patients who developed hepatic veno-occlus- age to structures in zone 3 of the liver acinus.4 In patients ive disease (VOD) following hematopoietic stem cell who have undergone hematopoietic stem cell transplan- transplantation were treated with recombinant tissue tation, chemoradiotherapy-induced endothelial cell damage plasminogen activator (rtPA) with or without heparin. is likely to be responsible for the pathogenesis of vessel rtPA was started a median of 13 days post transplant obstruction.5 (range 4–35). All patients received rtPA at a dose of 10 Treatment of established VOD has primarily been sup- mg/day as a starting dose, and 12 patients also received portive and any specific measures have resulted in little heparin (1500 U bolus; then 100 U/kg/day as a continu- impact on outcome. Based on the available evidence for ous i.v. infusion). The median number of days of rtPA involvement of hemostatic mechanisms and cytokines in therapy was 2.5 (1–12). The median total serum biliru- the pathogenesis of VOD,6–8 anti-thrombotic and anti-cyto- bin level was 116 mmol/l (range 63–194) at the begin- kine agents have been assessed for their role in treatment. -
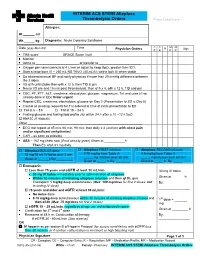
EXAMPLE Alteplase Thrombolytic Central Changes Noted
INTERIM ACS STEMI Alteplase Thrombolysis Orders Place Label Here Allergies: Ht. cm Wt. kg Diagnosis: Acute Coronary Syndrome C C M M Date (yyyy-Mon-dd) Time R Sign Physician Orders P E P R TIMI score ____________ GRACE Score (risk) ____________________ Monitor Admit to or transfer to _______________________ Oxygen per nasal cannula at 4 L/min or adjust to keep SpO2 greater than 92% Start a large bore IV – 250 mL NS TKVO (40 mL/h); saline lock IV when stable Do bilateral manual BP and notify physician if more than 20 mmHg difference between the 2 sides VS q1h until stable then q4h x 12 h, then TID & prn Neuro VS pre and 15 min post thrombolysis, then q1h x 4, q4h x 12 h, TID and prn CBC, PT, PTT, ALT, creatinine, electrolytes, glucose, magnesium, TnI and urea (if not already done in ED) Order urgent Repeat CBC, creatinine, electrolytes, glucose on Day 2 (Presentation to ED is Day 0) Cancel all pending requests for TnI ordered at time of initial presentation to ED TnI at 6 – 8 h TnI at 18 – 24 h Fasting glucose and fasting lipid profile (do within 24 h after a 10 –12 h fast) HbA1C (if diabetic) Other _______________________________________________________________ ECG stat repeat at 45 min, 60 min, 90 min: then daily x 3 (and prn with chest pain and/or significant arrhythmias) CXR – as soon as possible ASA – 162 mg chew now (if not already given) Given at h Then EC ASA 81 mg daily. Alteplase BOLUS dose Alteplase FIRST infusion Alteplase SECOND infusion 15 mg/15 mL IV bolus over 2 min 0.75 mg/kg from Table A 0.5 mg/kg from Table A _____ mg infusion over 30 min _____ mg infusion over 60 min Given at ______h By:_________ Given at _____ h By: ________ Given at _____ h By: _____ Enoxaparin Less than 75 years and eGFR at least 30 mL/min 30 mg IV bolus 30 mg IV bolus immediately prior to administration of alteplase Within 30 minutes of initiating alteplase infusion and then q12h, give Given at _______h Enoxaparin 1 mg/kg deep subcutaneous (Max. -

ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent
ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent ). Indications: - Management of acute myocardial infarction for the lysis of thrombi in coronary arteries; management of acute ischemic stroke -Acute myocardial infarction (AMI): Chest pain ≥20 minutes, ≤12-24 hours; S-T elevation ≥0.1 mV in at least two ECG leads -Acute pulmonary embolism (APE): Age ≤75 years: Documented massive pulmonary embolism by pulmonary angiography or echocardiography or high probability lung scan with clinical shock . -Restoration of central venous catheter function *Unlabeled/Investigational :Acute peripheral arterial occlusive disease. Dosage: -Coronary artery thrombi: Front loading dose (weight-based): -Patients >67 kg: Total dose: 100 mg over 1.5 hours; infuse 15 mg over 1-2 minutes. Infuse 50 mg over 30 minutes. Infuse remaining 35 mg of alteplase over the next hour. Maximum total dose: 100 mg -Patients ≤67 kg: Infuse 15 mg I.V. bolus over 1-2 minutes, then infuse 0.75 mg/kg (not to exceed 50 mg) over next 30 minutes, followed by 0.5 mg/kg over next 60 minutes (not to exceed 35 mg) Maximum total dose: 100 mg. See “Notes.” Note: Concurrently, begin heparin 60 units/kg bolus (maximum: 4000 units) followed by continuous infusion of 12 units/kg/hour (maximum: 1000 units/hour) and adjust to aPTT target of 1.5-2 times the upper limit of control. Note: Thrombolytic should be administered within 30 minutes of hospital arrival. Administer concurrent aspirin, clopidogrel, and anticoagulant therapy (ie, unfractionated heparin, enoxaparin, or fondaparinux) with alteplase (O’Gara, 2013). -Acute massive or submassive pulmonary embolism: I.V. (Activase®): 100 mg over 2 hours; may be administered as a 10 mg bolus followed by 90 mg over 2 hours as was done in patients with submassive PE (Konstantinides, 2002). -

ACTIVASE (Alteplase) for Injection, for Intravenous Use Initial U.S
Application 103172 This document contains: Label for ACTIVASE [Supplement 5203, Action Date 02/13/2015] Also available: Label for CATHFLO ACTIVASE [Supplement 5071, Action Date 01/04/2005] HIGHLIGHTS OF PRESCRIBING INFORMATION Acute Ischemic Stroke These highlights do not include all the information needed to use • Current intracranial hemorrhage. (4.1) ACTIVASE safely and effectively. See full prescribing information for • Subarachnoid hemorrhage. (4.1) ACTIVASE. Acute Myocardial Infarction or Pulmonary Embolism • History of recent stroke. (4.2) ACTIVASE (alteplase) for injection, for intravenous use Initial U.S. Approval: 1987 -----------------------WARNINGS AND PRECAUTIONS----------------------- • Increases the risk of bleeding. Avoid intramuscular injections. Monitor for ---------------------------INDICATIONS AND USAGE-------------------------- bleeding. If serious bleeding occurs, discontinue Activase. (5.1) Activase is a tissue plasminogen activator (tPA) indicated for the treatment of • Monitor patients during and for several hours after infusion for orolingual • Acute Ischemic Stroke (AIS). (1.1) angioedema. If angioedema develops, discontinue Activase. (5.2) • Acute Myocardial Infarction (AMI) to reduce mortality and incidence of • Cholesterol embolism has been reported rarely in patients treated with heart failure. (1.2) thrombolytic agents. (5.3) Limitation of Use in AMI: the risk of stroke may be greater than the benefit • Consider the risk of reembolization from the lysis of underlying deep in patients at low risk of death -
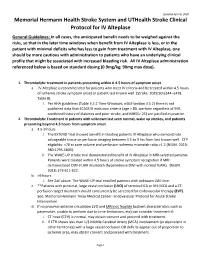
Protocol-IV-Alteplase.Pdf
Updated April 6, 2020 Memorial Hermann Health Stroke System and UTHealth Stroke Clinical Protocol for IV Alteplase General Guidelines: In all cases, the anticipated benefit needs to be weighed against the risks, so that in the later time windows when benefit from IV Alteplase is less, or in the patient with minimal deficits who has less to gain from treatment with IV Alteplase, one should be more cautious with administration to patients who have an underlying clinical profile that might be associated with increased bleeding risk. All IV Alteplase administration referenced below is based on standard dosing (0.9mg/kg; 90mg max dose). 1. Thrombolytic treatment in patients presenting within 0-4.5 hours of symptom onset. a. IV Alteplase is recommended for patients who meet IV criteria and be treated within 4.5 hours of ischemic stroke symptom onset or patient last known well. (Stroke. 2019;50:e344–e418. Table 8). i. Per AHA guidelines (Table 3.5.2 Time Windows; e363-Section 3.5.2) there is not published data that ECASS III exclusion criteria (age > 80, warfarin regardless of INR, combined history of diabetes and prior stroke, and NIHSS> 25) are justified in practice. 2. Thrombolytic Treatment in patients with unknown last seen normal, wake up strokes, and patients presenting beyond 4.5 hours from symptom onset. a. 4.5-9 hours i. The EXTEND Trial showed benefit in treating patients IV Alteplase who demonstrate salvageable tissue on perfusion imaging between 4.5 to 9 hrs from last known well. CTP eligibility: <70 cc core volume and perfusion-ischemia mismatch ratio >1.2 (NEJM. -

A First in Class Treatment for Thrombosis Prevention. a Phase I
Journal of Cardiology and Vascular Medicine Research Open Access A First in Class Treatment for Thrombosis Prevention. A Phase I study with CS1, a New Controlled Release Formulation of Sodium Valproate 1,2* 2 3 2 1,2 Niklas Bergh , Jan-Peter Idström , Henri Hansson , Jonas Faijerson-Säljö , Björn Dahlöf 1Department of Molecular and Clinical Medicine, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden 2 Cereno Scientific AB, Gothenburg, Sweden 3 Galenica AB, Malmö, Sweden *Corresponding author: Niklas Bergh, The Wallenberg Laboratory for Cardiovascular Research Sahlgrenska University Hospi- tal Bruna Stråket 16, 413 45 Göteborg, Tel: +46 31 3421000; E-Mail: [email protected] Received Date: June 11, 2019 Accepted Date: July 25, 2019 Published Date: July 27, 2019 Citation: Niklas Bergh (2019) A First in Class Treatment for Thrombosis Prevention? A Phase I Study With Cs1, a New Con- trolled Release Formulation of Sodium Valproate. J Cardio Vasc Med 5: 1-12. Abstract Several lines of evidence indicate that improving fibrinolysis by valproic acid may be a fruitful strategy for throm- bosis prevention. This study investigated the safety, pharmacokinetics, and effect on biomarkers for thrombosis of CS1, a new advanced controlled release formulation of sodium valproate designed to produce optimum valproic acid concen- trations during the early morning hours, when concentrations of plasminogen activator inhibitor (PAI)-1 and the risk of thrombotic events is highest. Healthy volunteers (n=17) aged 40-65 years were randomized to receive single doses of one of three formulations of CS1 (FI, FII, and FIII). The CS1 FII formulation showed the most favorable pharmacokinetics and was chosen for multiple dosing. -

Transition of Anticoagulants 2019
Transition of Anticoagulants 2019 Van Hellerslia, PharmD, BCPS, CACP, Brand Generic Clinical Assistant Professor of Pharmacy Practice, Angiomax bivalirudin Temple University School of Pharmacy, Philadelphia, PA Arixtra fondaparinux Bevyxxa betrixaban Pallav Mehta, MD, Assistant Professor of Medicine, Coumadin warfarin Division of Hematology/Oncology, Eliquis apixaban MD Anderson Cancer Center at Cooper, Camden, NJ Fragmin dalteparin Lovenox enoxaparin Reviewer: Kelly Rudd, PharmD, BCPS, CACP, Pradaxa dabigatran Clinical Specialist, Anticoagulation, Bassett Medical Center, Savaysa edoxaban Cooperstown, NY Xarelto rivaroxaban From To Action Apixaban Argatroban/ Wait 12 hours after last dose of apixaban to initiate parenteral anticoagulant. In cases of Bivalirudin/ high bleeding risk, consider omitting initial bolus when transitioning to heparin infusion. Enoxaparin/ Dalteparin/ Fondaparinux/ Heparin Apixaban Warfarin When going from apixaban to warfarin, consider the use of parenteral anticoagulation as a bridge (eg, start heparin infusion or therapeutic enoxaparin AND warfarin 12 hours after last dose of apixaban and discontinue parenteral anticoagulant when INR is therapeutic). Apixaban affects INR so that initial INR measurements during the transition may not be useful for determining the appropriate dose of warfarin. Apixaban Betrixaban, Wait 12 hours from last dose of apixaban to initiate betrixaban, dabigatran, edoxaban, or Dabigatran, rivaroxaban. Edoxaban, or Rivaroxaban Argatroban Apixaban, Start apixaban, betrixaban, dabigatran, -

The Treatment and Prevention Ofacute Ischemic Stroke
EDITORIAL Alvaro Nagib Atallah* The treatment and prevention of acute ischemic stroke rotecting the brain from the consequences .of alternated with placebo (lower dose) and placebo injections vascular obstruction is obviously very important. every 12 hours, for 10 days. The evaluation at 6 months PHowever, how to manage this is a very complex showed that the treated group had a lower incidence rate task. Three recent studies have provided evidence that of poor outcomes, death or dependency in daily activities, I 3 should not be ignored or misinterpreted by physicians. - 45 vs. 65%. In other words, it was necessary to treat 5 The National Institute of Neurological Disorders and patients to benefit one. Evaluations at 10 days did not show Stroke rt-PA Stroke Study Groupl shows the results of a differences in death rates or haemorrhage transformation randomized, collaborative placebo-controlled trial. Six of the cerebral infarction. hundred and twenty-four patients were studied. The The Multicentre Acute Stroke Trial-Italy (MAST-I) treatment was started before 90' of the start of the stroke Group compared the effectiveness of streptokinase, aspirin or before 180'. Patients received recombinant rt-PA and a combination of both for the treatment of ischemic (alteplase) 0.9 mg/kg or placebo. A careful neurological stroke. Six hundred and twenty-two patients were evaluation was done at 24 hours and 3 months after the randomized to receive I hour infusions of 1.5 mD of stroke. streptokinase alone, the same dose of streptokinase plus There were no significant differences between the 300 mg of buffered aspirin, or 300 mg of aspirin alone for groups at 24 hours after the stroke. -

(Dipotassium Salt) and Heparin on the Estimation of Packed Cell Volume
J Clin Pathol: first published as 10.1136/jcp.19.2.196 on 1 March 1966. Downloaded from J. clin. Path. (1966), 19, 196 Effect of ethylene-diamine-tetra-acetic acid (dipotassium salt) and heparin on the estimation of packed cell volume C. A. PENNOCK AND K. W. JONES From the Department of Haematology, Gibson Laboratories, Radcliffe Infirmary, Oxford SYNOPSIS The effect of varying concentrations of ethylene-diamine-tetra-acetic acid (E.D.T.A.) (dipotassium salt) and heparin on the estimation of packed cell volume has been studied using a microhaematocrit method. Varying concentrations of E.D.T.A. can produce serious errors in estimation of packed cell volume (P.C.V.) and reliable results are only obtained within the range of 1 to 2 mg./ml. Heparin is a more suitable anticoagulant for this investigation as varying the con- centration has little effect. Storage with either anticoagulant at suitable concentrations for 24 hours at room temperature has little influence on the results. The estimation ofthe packed cell volume (P.C.V.) is bottles are often returned to this laboratory contain- regarded as a reliable investigation in the diagnosis ing less than the recommended amount of blood.copyright. of anaemia, and errors in the estimation of mean Ethylene-diamine-tetra-acetic acid is known to corpuscular haemoglobin concentration (M.C.H.C.) cause distortion and shrinkage of red cells and are thought to be due more often to errors in the to affect the estimation of P.C.V. by conventional estimation of haemoglobin than of the P.C.V.