The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’S Perspective
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pleiotropic Effects of Antithrombin Strand 1C Substitution Mutations
Pleiotropic effects of antithrombin strand 1C substitution mutations. D A Lane, … , E Thompson, G Sas J Clin Invest. 1992;90(6):2422-2433. https://doi.org/10.1172/JCI116133. Research Article Six different substitution mutations were identified in four different amino acid residues of antithrombin strand 1C and the polypeptide leading into strand 4B (F402S, F402C, F402L, A404T, N405K, and P407T), and are responsible for functional antithrombin deficiency in seven independently ascertained kindreds (Rosny, Torino, Maisons-Laffitte, Paris 3, La Rochelle, Budapest 5, and Oslo) affected by venous thromboembolic disease. In all seven families, variant antithrombins with heparin-binding abnormalities were detected by crossed immunoelectrophoresis, and in six of the kindreds there was a reduced antigen concentration of plasma antithrombin. Two of the variant antithrombins, Rosny and Torino, were purified by heparin-Sepharose and immunoaffinity chromatography, and shown to have greatly reduced heparin cofactor and progressive inhibitor activities in vitro. The defective interactions of these mutants with thrombin may result from proximity of s1C to the reactive site, while reduced circulating levels may be related to s1C proximity to highly conserved internal beta strands, which contain elements proposed to influence serpin turnover and intracellular degradation. In contrast, s1C is spatially distant to the positively charged surface which forms the heparin binding site of antithrombin; altered heparin binding properties of s1C variants may therefore reflect conformational linkage between the reactive site and heparin binding regions of the molecule. This work demonstrates that point mutations in and immediately adjacent to strand 1C have multiple, or pleiotropic, […] Find the latest version: https://jci.me/116133/pdf Pleiotropic Effects of Antithrombin Strand 1C Substitution Mutations David A. -

Human <X2-Macroblobulin and Plasmin. (459) Antithrombin III
924 Abstracts added before the incubation of CPA positive plasma at 0° C for 20 hours. Addition of CIINH after CPA generation did not affect the shortened Thrombotest Time (TT). Synthetic amidino compounds (diOHstilbamidine, dibromopropamidine}, which have b een cla imed as sp ecific inhibitors of CI est e rase, were al so effective inhib i tors of CPA in final concentrations of l0- 4 - lO- • M . Alike to CliNH t h ey h ad no effect on a TT shortened by previous gen eration of CPA. In 8 subjects with CIINH d eficiency the shortening of t.he TT of plasma incubated at 0° C for 20 hours exeeeded that in a control group of 48 men and women not us ing oestrogenic drugs (p 0.05). CIINH activity proved to be consumed during CPA probably by binding of kallikrein, since purified CPA-kallikrein blocked purified CIINH activity. The antigen level of CIINH was n ot affected by CPA. This finding h as diagnostic importa nce since fal se low levels of CfiNH activity may b e detected in serum samples exp osed to CPA favouring conditions. In fact t his proved to be the case in a l arge proport ion of subjects t h ou ght to be suffering from so-called acquir ed angioneurotic oed em a (Quincke's oedema urticaria) on ground of low CfiNH activity determined in a frozen and thawed serum sample. C1INH activity proved to b e completely normal in fresh samples. P . Lambin, J. ll!J.. Fine, R. Audran and M. -

Urokinase, a Promising Candidate for Fibrinolytic Therapy for Intracerebral Hemorrhage
LABORATORY INVESTIGATION J Neurosurg 126:548–557, 2017 Urokinase, a promising candidate for fibrinolytic therapy for intracerebral hemorrhage *Qiang Tan, MD,1 Qianwei Chen, MD1 Yin Niu, MD,1 Zhou Feng, MD,1 Lin Li, MD,1 Yihao Tao, MD,1 Jun Tang, MD,1 Liming Yang, MD,1 Jing Guo, MD,2 Hua Feng, MD, PhD,1 Gang Zhu, MD, PhD,1 and Zhi Chen, MD, PhD1 1Department of Neurosurgery, Southwest Hospital, Third Military Medical University, Chongqing; and 2Department of Neurosurgery, 211st Hospital of PLA, Harbin, People’s Republic of China OBJECTIVE Intracerebral hemorrhage (ICH) is associated with a high rate of mortality and severe disability, while fi- brinolysis for ICH evacuation is a possible treatment. However, reported adverse effects can counteract the benefits of fibrinolysis and limit the use of tissue-type plasminogen activator (tPA). Identifying appropriate fibrinolytics is still needed. Therefore, the authors here compared the use of urokinase-type plasminogen activator (uPA), an alternate thrombolytic, with that of tPA in a preclinical study. METHODS Intracerebral hemorrhage was induced in adult male Sprague-Dawley rats by injecting autologous blood into the caudate, followed by intraclot fibrinolysis without drainage. Rats were randomized to receive uPA, tPA, or saline within the clot. Hematoma and perihematomal edema, brain water content, Evans blue fluorescence and neurological scores, matrix metalloproteinases (MMPs), MMP mRNA, blood-brain barrier (BBB) tight junction proteins, and nuclear factor–κB (NF-κB) activation were measured to evaluate the effects of these 2 drugs in ICH. RESULTS In comparison with tPA, uPA better ameliorated brain edema and promoted an improved outcome after ICH. -

Fibrinolysis and Anticoagulant Potential of a Metallo Protease Produced by Bacillus Subtilis K42
Fibrinolysis and anticoagulant potential of a metallo protease produced by Bacillus subtilis K42 WESAM AHASSANEIN, ESSAM KOTB*, NADIA MAWNY and YEHIA AEL-ZAWAHRY Department of Microbiology, Faculty of Science, Zagazig University, Zagazig, Egypt 44519 *Corresponding author (Email, [email protected]) In this study, a potent fibrinolytic enzyme-producing bacterium was isolated from soybean flour and identified as Bacillus subtilis K42 and assayed in vitro for its thrombolytic potential. The molecular weight of the purified enzyme was 20.5 kDa and purification increased its specific activity 390-fold with a recovery of 14%. Maximal activity was attained at a temperature of 40°C (stable up to 65°C) and pH of 9.4 (range: 6.5–10.5). The enzyme retained up to 80% of its original activity after pre-incubation for a month at 4°C with organic solvents such as diethyl ether (DE), toluene (TO), acetonitrile (AN), butanol (BU), ethyl acetate (EA), ethanol (ET), acetone (AC), methanol (ME), isopropanol (IP), diisopropyl fluorophosphate (DFP), tosyl-lysyl-chloromethylketose (TLCK), tosyl-phenylalanyl chloromethylketose (TPCK), phenylmethylsulfonylfluoride (PMSF) and soybean trypsin inhibitor (SBTI). Aprotinin had little effect on this activity. The presence of ethylene diaminetetraacetic acid (EDTA), a metal-chelating agent and two metallo protease inhibitors, 2,2′-bipyridine and o-phenanthroline, repressed the enzymatic activity significantly. This, however, could be restored by adding Co2+ to the medium. The clotting time of human blood serum in the presence of this enzyme reached a relative PTT of 241.7% with a 3.4-fold increase, suggesting that this enzyme could be an effective antithrombotic agent. -
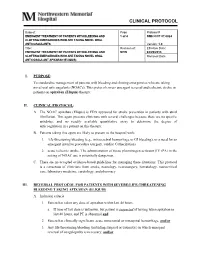
Clinical Protocol
CLINICAL PROTOCOL Subject: Page Protocol # EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND 1 of 4 NMH CCP 07.0024 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL ANTICOAGULANTS Version: 1.0 Title: Revision of: Effective Date: EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND NEW 04/29/2013 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL Removal Date: ANTICOAGULANT APIXABAN (ELIQUIS) I. PURPOSE: To standardize management of patients with bleeding and clotting emergencies who are taking novel oral anticoagulants (NOACs). This protocol covers emergent reversal and ischemic stroke in patients on apixaban (Eliquis) therapy. II. CLINICAL PROTOCOL: A. The NOAC apixaban (Eliquis) is FDA approved for stroke prevention in patients with atrial fibrillation. This agent presents clinicians with several challenges because there are no specific antidotes, and no readily available quantitative assay to determine the degree of anticoagulation in a patient on this therapy. B. Patients taking this agent are likely to present to the hospital with; 1. life-threatening bleeding (e.g., intracerebral hemorrhage or GI bleeding), or a need for an emergent invasive procedure (surgery, cardiac Catherization) 2. acute ischemic stroke. The administration of tissue plasminogen activator (IV tPA) in the setting of NOAC use is potentially dangerous. C. There are no accepted evidence-based guidelines for managing these situations. This protocol is a consensus of clinicians from stroke, neurology, neurosurgery, hematology, neurocritical care, laboratory medicine, cardiology, and pharmacy. III. REVERSAL PROTOCOL FOR PATIENTS WITH SEVERE/LIFE-THREATENING BLEEDING TAKING APIXABAN (ELIQUIS) A. Inclusion criteria: 1. Patient has taken any dose of apixaban within last 48 hours. a. If time of last dose is unknown, but patient is suspected of having taken apixaban in last 48 hours, and PT is abnormal and 2. -

2: Genetic Aspects of a Antitrypsin Deficiency
259 REVIEW SERIES Thorax: first published as 10.1136/thx.2003.006502 on 25 February 2004. Downloaded from a1-Antitrypsin deficiency ? 2: Genetic aspects of a1- antitrypsin deficiency: phenotypes and genetic modifiers of emphysema risk D L DeMeo, E K Silverman ............................................................................................................................... Thorax 2004;59:259–264. doi: 10.1136/thx.2003.006502 The genetic aspects of AAT deficiency and the variable globin locus which results in haemoglobin S. This mutant haemoglobin assumes a sickle shape manifestations of lung disease in PI Z individuals are when deoxygenated, causing an array of clinical reviewed. The role of modifying genetic factors which may consequences. However, affected individuals interact with environmental factors (such as cigarette vary widely in disease severity. One known genetic modifier of sickle cell disease is heredi- smoking) is discussed, and directions for future research tary persistence of fetal haemoglobin in which are presented. continued production of Hb F impairs sickling ........................................................................... and limits disease severity. In pulmonary medicine, cystic fibrosis and AAT deficiency—classic monogenic disorders he susceptibility to develop chronic obstruc- that display marked variability in disease sus- tive pulmonary disease (COPD) results from ceptibility—demonstrate elements of genetic Ta combination of genetic and environmental complexity. In severe AAT deficiency the Z factors. The most important environmental risk mutation leads to low serum protein levels, but factor for COPD is cigarette smoking, but PI Z individuals vary markedly in lung and liver individuals vary in their susceptibility to the disease development and severity. The altered effects of cigarette smoke and only a minority of AAT protein is the product of a single gene, but smokers will develop COPD. -

Assembly of an Integrated Human Lung Cell Atlas Reveals That
medRxiv preprint doi: https://doi.org/10.1101/2020.06.02.20120634; this version posted June 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Assembly of an integrated human lung cell atlas reveals that SARS-CoV-2 receptor is co-expressed with key elements of the kinin-kallikrein, renin-angiotensin and coagulation systems in alveolar cells Davi Sidarta-Oliveira1,2, Carlos Poblete Jara1,3, Adriano J. Ferruzzi4, Munir S. Skaf4, William H. Velander5, Eliana P. Araujo1,3, Licio A. Velloso1 1Laboratory of Cell Signaling, Obesity and Comorbidities Research Center, University of Campinas, Brazil 2 Physician-Scientist Graduate Program, School of Medical Sciences, University of Campinas, Brazil 3Nursing School, University of Campinas, Brazil 4Institute of Chemistry and Center for Computing in Engineering and Sciences University of Campinas, Brazil 5Department of Chemical and Biomolecular Engineering, University of Nebraska, Lincoln, USA Correspondence: Licio A. Velloso Laboratory of Cell Signaling, Obesity and Comorbidities Research Center, University of Campinas, Campinas, Brazil Address: Rua Carl Von Lineaus s/n, Instituto de Biologia - Bloco Z. Campus Universitário Zeferino Vaz - Barão Geraldo, Campinas - SP, 13083-864 Phone: +55 19 3521-0025 E-mail: [email protected] Abstract SARS-CoV-2, the pathogenic agent of COVID-19, employs angiotensin converting enzyme-2 (ACE2) as its cell entry receptor. Clinical data reveal that in severe COVID- 19, SARS-CoV-2 infects the lung, leading to a frequently lethal triad of respiratory insufficiency, acute cardiovascular failure, and coagulopathy. -

Alpha -Antitrypsin Deficiency
The new england journal of medicine Review Article Dan L. Longo, M.D., Editor Alpha1-Antitrypsin Deficiency Pavel Strnad, M.D., Noel G. McElvaney, D.Sc., and David A. Lomas, Sc.D. lpha1-antitrypsin (AAT) deficiency is one of the most common From the Department of Internal Med genetic diseases. Most persons carry two copies of the wild-type M allele icine III, University Hospital RWTH of SERPINA1, which encodes AAT, and have normal circulating levels of the (Rheinisch–Westfälisch Technische Hoch A schule) Aachen, Aachen, Germany (P.S.); protein. Ninety-five percent of severe cases of AAT deficiency result from the homo- the Irish Centre for Genetic Lung Dis zygous substitution of a single amino acid, Glu342Lys (the Z allele), which is present ease, Royal College of Surgeons in Ire in 1 in 25 persons of European descent (1 in 2000 persons of European descent land, Beaumont Hospital, Dublin (N.G.M.); and UCL Respiratory, Division of Medi are homozygotes). Mild AAT deficiency typically results from a different amino cine, Rayne Institute, University College acid replacement, Glu264Val (the S allele), which is found in 1 in 4 persons in the London, London (D.A.L.). Address re Iberian peninsula. However, many other alleles have been described that have vari- print requests to Dr. Lomas at UCL Re spiratory, Rayne Institute, University Col able effects, such as a lack of protein production (null alleles), production of mis- lege London, London WC1E 6JF, United folded protein, or no effect on the level or function of circulating AAT (Table 1). Kingdom, or at d . -

The Plasmin–Antiplasmin System: Structural and Functional Aspects
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Bern Open Repository and Information System (BORIS) Cell. Mol. Life Sci. (2011) 68:785–801 DOI 10.1007/s00018-010-0566-5 Cellular and Molecular Life Sciences REVIEW The plasmin–antiplasmin system: structural and functional aspects Johann Schaller • Simon S. Gerber Received: 13 April 2010 / Revised: 3 September 2010 / Accepted: 12 October 2010 / Published online: 7 December 2010 Ó Springer Basel AG 2010 Abstract The plasmin–antiplasmin system plays a key Plasminogen activator inhibitors Á a2-Macroglobulin Á role in blood coagulation and fibrinolysis. Plasmin and Multidomain serine proteases a2-antiplasmin are primarily responsible for a controlled and regulated dissolution of the fibrin polymers into solu- Abbreviations ble fragments. However, besides plasmin(ogen) and A2PI a2-Antiplasmin, a2-Plasmin inhibitor a2-antiplasmin the system contains a series of specific CHO Carbohydrate activators and inhibitors. The main physiological activators EGF-like Epidermal growth factor-like of plasminogen are tissue-type plasminogen activator, FN1 Fibronectin type I which is mainly involved in the dissolution of the fibrin K Kringle polymers by plasmin, and urokinase-type plasminogen LBS Lysine binding site activator, which is primarily responsible for the generation LMW Low molecular weight of plasmin activity in the intercellular space. Both activa- a2M a2-Macroglobulin tors are multidomain serine proteases. Besides the main NTP N-terminal peptide of Pgn physiological inhibitor a2-antiplasmin, the plasmin–anti- PAI-1, -2 Plasminogen activator inhibitor 1, 2 plasmin system is also regulated by the general protease Pgn Plasminogen inhibitor a2-macroglobulin, a member of the protease Plm Plasmin inhibitor I39 family. -

ACTIVASE (Alteplase) for Injection, for Intravenous Use Initial U.S
Application 103172 This document contains: Label for ACTIVASE [Supplement 5203, Action Date 02/13/2015] Also available: Label for CATHFLO ACTIVASE [Supplement 5071, Action Date 01/04/2005] HIGHLIGHTS OF PRESCRIBING INFORMATION Acute Ischemic Stroke These highlights do not include all the information needed to use • Current intracranial hemorrhage. (4.1) ACTIVASE safely and effectively. See full prescribing information for • Subarachnoid hemorrhage. (4.1) ACTIVASE. Acute Myocardial Infarction or Pulmonary Embolism • History of recent stroke. (4.2) ACTIVASE (alteplase) for injection, for intravenous use Initial U.S. Approval: 1987 -----------------------WARNINGS AND PRECAUTIONS----------------------- • Increases the risk of bleeding. Avoid intramuscular injections. Monitor for ---------------------------INDICATIONS AND USAGE-------------------------- bleeding. If serious bleeding occurs, discontinue Activase. (5.1) Activase is a tissue plasminogen activator (tPA) indicated for the treatment of • Monitor patients during and for several hours after infusion for orolingual • Acute Ischemic Stroke (AIS). (1.1) angioedema. If angioedema develops, discontinue Activase. (5.2) • Acute Myocardial Infarction (AMI) to reduce mortality and incidence of • Cholesterol embolism has been reported rarely in patients treated with heart failure. (1.2) thrombolytic agents. (5.3) Limitation of Use in AMI: the risk of stroke may be greater than the benefit • Consider the risk of reembolization from the lysis of underlying deep in patients at low risk of death -

Plasmin (Human) 1.00 Mg
Plasmin (Human) 1.00 mg Ref#: HPLAS Lot#: xxxxxx Exp. Date: xxxx-xx Store at -10°C to -20°C For Research Use Only Not for Use in Diagnostic Procedures For in vitro use only Description: Plasmin Format: Frozen in 50mM Hepes/ 50 mM sodium acetate/ 50% glycerol/ pH 8.5 Host: Human Storage: Store between -10°C and -20°C Volume: 1 vial containing 0.962 mL Total Protein: 1.00 mg 1% Concentration: 1.04 mg/mL by Absorbance; Extinction Coefficient E 280 = 17.0 Activity: 228.00 nkat/mg Molecular weight: 83000 daltons Plasminogen is synthesized in the liver and circulates in plasma at a concentration of ~200 μg/mL (~2.3 μM). Plasminogen is a single-chain glycoprotein of ~88 kDa that consists of a catalytic domain followed by five kringle structures. Within these kringle structures are four low-affinity lysine binding sites and one high-affinity lysine binding site. It is through these lysine binding sites that plasminogen binds to fibrin and to α2-Antiplasmin. Native Plasminogen (Glu-Plasminogen) exists in two variants that differ in their extent of glycosylation, and each variant has up to six isoelectric forms with respect to sialic acid content, for a total of 12 molecular forms. Activation of Glu-Plasminogen by the Plasminogen activators Urokinase (UPA), or tissue Plasminogen Activator (tPA) occurs by cleavage after residue Arg560 to produce the two-chain active serine protease Plasmin. In a positive feedback reaction, the Plasmin generated cleaves an ~8 kDa peptide from Glu-Plasminogen, producing lys77- Plasminogen which has a higher affinity for Fibrin and when bound is a preferred substrate for Plasminogen activators such as Urokinase. -

A First in Class Treatment for Thrombosis Prevention. a Phase I
Journal of Cardiology and Vascular Medicine Research Open Access A First in Class Treatment for Thrombosis Prevention. A Phase I study with CS1, a New Controlled Release Formulation of Sodium Valproate 1,2* 2 3 2 1,2 Niklas Bergh , Jan-Peter Idström , Henri Hansson , Jonas Faijerson-Säljö , Björn Dahlöf 1Department of Molecular and Clinical Medicine, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden 2 Cereno Scientific AB, Gothenburg, Sweden 3 Galenica AB, Malmö, Sweden *Corresponding author: Niklas Bergh, The Wallenberg Laboratory for Cardiovascular Research Sahlgrenska University Hospi- tal Bruna Stråket 16, 413 45 Göteborg, Tel: +46 31 3421000; E-Mail: [email protected] Received Date: June 11, 2019 Accepted Date: July 25, 2019 Published Date: July 27, 2019 Citation: Niklas Bergh (2019) A First in Class Treatment for Thrombosis Prevention? A Phase I Study With Cs1, a New Con- trolled Release Formulation of Sodium Valproate. J Cardio Vasc Med 5: 1-12. Abstract Several lines of evidence indicate that improving fibrinolysis by valproic acid may be a fruitful strategy for throm- bosis prevention. This study investigated the safety, pharmacokinetics, and effect on biomarkers for thrombosis of CS1, a new advanced controlled release formulation of sodium valproate designed to produce optimum valproic acid concen- trations during the early morning hours, when concentrations of plasminogen activator inhibitor (PAI)-1 and the risk of thrombotic events is highest. Healthy volunteers (n=17) aged 40-65 years were randomized to receive single doses of one of three formulations of CS1 (FI, FII, and FIII). The CS1 FII formulation showed the most favorable pharmacokinetics and was chosen for multiple dosing.