A First in Class Treatment for Thrombosis Prevention. a Phase I
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Aspirin for the Primary Prevention of Cardiovascular Events: a Summary of the Evidence
Aspirin for the Primary Prevention of Cardiovascular Events: A Summary of the Evidence Michael Hayden, MD; Michael Pignone, MD, MPH; Christopher Phillips, MD; Cynthia Mulrow, MD, MSc Epidemiolgy power to precisely estimate major harms such as gastrointestinal bleeding and hemorrhagic stroke.4,5 Cardiovascular disease (CVD), including ischemic coronary heart disease (CHD), stroke, and The results of these first 2 randomized, controlled peripheral vascular disease, is the leading cause of trials were available to the members of the U.S. morbidity and mortality in the United States.1 In Preventive Services Task Force at the time of their 1997, the age-adjusted mortality rate due to 1996 recommendation.4,5 At that time, the Task coronary heart disease, cerebrovascular disease, and Force found insufficient evidence to recommend for atherosclerotic disease was 194 per 100,000 people, or against routine aspirin prophylaxis for the equating to more than 500,000 deaths per year.1 The primary prevention of myocardial infarction in estimated direct and indirect costs of CHD and asymptomatic people.6 stroke were $145 billion for 1999.2 Two additional large primary prevention trials Although the benefit of aspirin for patients with were published in 1998, and another was reported in known CVD is well established,3 the question of January 2001.7, 8, 9 In light of the new evidence, the whether aspirin reduces the risk of CVD in people U.S. Preventive Services Task Force sought to without known CVD is controversial. Two early reassess the value of aspirin for the primary randomized trials of aspirin in healthy men, the U.S. -

Urokinase, a Promising Candidate for Fibrinolytic Therapy for Intracerebral Hemorrhage
LABORATORY INVESTIGATION J Neurosurg 126:548–557, 2017 Urokinase, a promising candidate for fibrinolytic therapy for intracerebral hemorrhage *Qiang Tan, MD,1 Qianwei Chen, MD1 Yin Niu, MD,1 Zhou Feng, MD,1 Lin Li, MD,1 Yihao Tao, MD,1 Jun Tang, MD,1 Liming Yang, MD,1 Jing Guo, MD,2 Hua Feng, MD, PhD,1 Gang Zhu, MD, PhD,1 and Zhi Chen, MD, PhD1 1Department of Neurosurgery, Southwest Hospital, Third Military Medical University, Chongqing; and 2Department of Neurosurgery, 211st Hospital of PLA, Harbin, People’s Republic of China OBJECTIVE Intracerebral hemorrhage (ICH) is associated with a high rate of mortality and severe disability, while fi- brinolysis for ICH evacuation is a possible treatment. However, reported adverse effects can counteract the benefits of fibrinolysis and limit the use of tissue-type plasminogen activator (tPA). Identifying appropriate fibrinolytics is still needed. Therefore, the authors here compared the use of urokinase-type plasminogen activator (uPA), an alternate thrombolytic, with that of tPA in a preclinical study. METHODS Intracerebral hemorrhage was induced in adult male Sprague-Dawley rats by injecting autologous blood into the caudate, followed by intraclot fibrinolysis without drainage. Rats were randomized to receive uPA, tPA, or saline within the clot. Hematoma and perihematomal edema, brain water content, Evans blue fluorescence and neurological scores, matrix metalloproteinases (MMPs), MMP mRNA, blood-brain barrier (BBB) tight junction proteins, and nuclear factor–κB (NF-κB) activation were measured to evaluate the effects of these 2 drugs in ICH. RESULTS In comparison with tPA, uPA better ameliorated brain edema and promoted an improved outcome after ICH. -

Fibrinolysis and Anticoagulant Potential of a Metallo Protease Produced by Bacillus Subtilis K42
Fibrinolysis and anticoagulant potential of a metallo protease produced by Bacillus subtilis K42 WESAM AHASSANEIN, ESSAM KOTB*, NADIA MAWNY and YEHIA AEL-ZAWAHRY Department of Microbiology, Faculty of Science, Zagazig University, Zagazig, Egypt 44519 *Corresponding author (Email, [email protected]) In this study, a potent fibrinolytic enzyme-producing bacterium was isolated from soybean flour and identified as Bacillus subtilis K42 and assayed in vitro for its thrombolytic potential. The molecular weight of the purified enzyme was 20.5 kDa and purification increased its specific activity 390-fold with a recovery of 14%. Maximal activity was attained at a temperature of 40°C (stable up to 65°C) and pH of 9.4 (range: 6.5–10.5). The enzyme retained up to 80% of its original activity after pre-incubation for a month at 4°C with organic solvents such as diethyl ether (DE), toluene (TO), acetonitrile (AN), butanol (BU), ethyl acetate (EA), ethanol (ET), acetone (AC), methanol (ME), isopropanol (IP), diisopropyl fluorophosphate (DFP), tosyl-lysyl-chloromethylketose (TLCK), tosyl-phenylalanyl chloromethylketose (TPCK), phenylmethylsulfonylfluoride (PMSF) and soybean trypsin inhibitor (SBTI). Aprotinin had little effect on this activity. The presence of ethylene diaminetetraacetic acid (EDTA), a metal-chelating agent and two metallo protease inhibitors, 2,2′-bipyridine and o-phenanthroline, repressed the enzymatic activity significantly. This, however, could be restored by adding Co2+ to the medium. The clotting time of human blood serum in the presence of this enzyme reached a relative PTT of 241.7% with a 3.4-fold increase, suggesting that this enzyme could be an effective antithrombotic agent. -
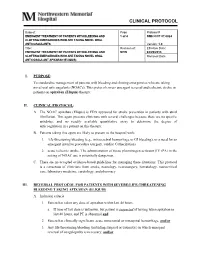
Clinical Protocol
CLINICAL PROTOCOL Subject: Page Protocol # EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND 1 of 4 NMH CCP 07.0024 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL ANTICOAGULANTS Version: 1.0 Title: Revision of: Effective Date: EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND NEW 04/29/2013 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL Removal Date: ANTICOAGULANT APIXABAN (ELIQUIS) I. PURPOSE: To standardize management of patients with bleeding and clotting emergencies who are taking novel oral anticoagulants (NOACs). This protocol covers emergent reversal and ischemic stroke in patients on apixaban (Eliquis) therapy. II. CLINICAL PROTOCOL: A. The NOAC apixaban (Eliquis) is FDA approved for stroke prevention in patients with atrial fibrillation. This agent presents clinicians with several challenges because there are no specific antidotes, and no readily available quantitative assay to determine the degree of anticoagulation in a patient on this therapy. B. Patients taking this agent are likely to present to the hospital with; 1. life-threatening bleeding (e.g., intracerebral hemorrhage or GI bleeding), or a need for an emergent invasive procedure (surgery, cardiac Catherization) 2. acute ischemic stroke. The administration of tissue plasminogen activator (IV tPA) in the setting of NOAC use is potentially dangerous. C. There are no accepted evidence-based guidelines for managing these situations. This protocol is a consensus of clinicians from stroke, neurology, neurosurgery, hematology, neurocritical care, laboratory medicine, cardiology, and pharmacy. III. REVERSAL PROTOCOL FOR PATIENTS WITH SEVERE/LIFE-THREATENING BLEEDING TAKING APIXABAN (ELIQUIS) A. Inclusion criteria: 1. Patient has taken any dose of apixaban within last 48 hours. a. If time of last dose is unknown, but patient is suspected of having taken apixaban in last 48 hours, and PT is abnormal and 2. -

The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’S Perspective
International Journal of Molecular Sciences Review The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’s Perspective Hau C. Kwaan 1,* and Paul F. Lindholm 2 1 Division of Hematology/Oncology, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA 2 Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; [email protected] * Correspondence: [email protected] Abstract: The novel coronavirus disease (COVID-19) has many characteristics common to those in two other coronavirus acute respiratory diseases, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). They are all highly contagious and have severe pulmonary complications. Clinically, patients with COVID-19 run a rapidly progressive course of an acute respiratory tract infection with fever, sore throat, cough, headache and fatigue, complicated by severe pneumonia often leading to acute respiratory distress syndrome (ARDS). The infection also involves other organs throughout the body. In all three viral illnesses, the fibrinolytic system plays an active role in each phase of the pathogenesis. During transmission, the renin-aldosterone- angiotensin-system (RAAS) is involved with the spike protein of SARS-CoV-2, attaching to its natural receptor angiotensin-converting enzyme 2 (ACE 2) in host cells. Both tissue plasminogen activator (tPA) and plasminogen activator inhibitor 1 (PAI-1) are closely linked to the RAAS. In lesions in the lung, kidney and other organs, the two plasminogen activators urokinase-type plasminogen activator (uPA) and tissue plasminogen activator (tPA), along with their inhibitor, plasminogen activator 1 (PAI-1), are involved. The altered fibrinolytic balance enables the development of a hypercoagulable Citation: Kwaan, H.C.; Lindholm, state. -

Venous Thromboembolism
CLINICAL PRACTICE GUIDELINES MOH/P/PAK/264.13(GU) Prevention and Treatment of Venous Thromboembolism VTE Ministry of Health Malaysian Society of National Heart Association Academy of Medicine Malaysia Haematology of Malaysia Malaysia STATEMENT OF INTENT These guidelines are meant to be a guide for clinical practice, based on the best available evidence at the time of development. Adherence to these guidelines may not necessarily ensure the best outcome in every case. Every health care provider is responsible for the management options available locally. REVIEW OF THE GUIDELINES These guidelines were issued in 2013 and will be reviewed in 2017 or sooner if new evidence becomes available. Electronic version available on the following website: http://www.haematology.org.my DISCLOSURE STATEMENT The panel members had completed disclosure forms. None held shares in pharmaceutical firms or acted as consultants to such firms (details are available upon request from the CPG Secretariat). SOURCES OF FUNDING The development of the CPG on Prevention and Treatment of Venous Thromboembolism was supported via unrestricted educational grant from Bayer Healthcare Pharmaceuticals. The funding body has not influenced the development of the guidelines. ISBN 978-967-12100-0-0 9 789671 210000 August 2013 © Ministry of Health Malaysia 01 GUIDELINES DEVELOPMENT The development group for these guidelines consists of Haematologist, Cardiologist, Neurologist, Obstetrician & Gynaecologist, Vascular Surgeon, Orthopaedic Surgeon, Anaesthesiologist, Pharmacologist and Pharmacist from the Ministry of Health Malaysia, Ministry of Higher Education Malaysia and the Private sector. Literature search was carried out at the following electronic databases: International Health Technology Assessment website, PUBMED, MEDLINE, Cochrane Database of Systemic Reviews (CDSR), Journal full teXt via OVID search engine and Science Direct. -

Proefschrift-Banne-Nemeth.Pdf
Stellingen behorende bij het proefschrift Venous thrombosis following lower-leg cast immobilization and knee arthroscopy From a population-based approach to individualized therapy 1. A prophylactic regimen of low-molecular-weight-heparin for eight days after knee arthroscopy or during the complete immobilization period in patients with casting of the lower leg is not efective for the prevention of symptomatic venous thromboembolism. -this thesis- 2. For patients with a history of venous thromboembolism who are undergoing surgery or are treated with a lower leg cast, the risk of recurrent venous thromboembolism is high. -this thesis- 3. Estimating the risk of venous thromboembolism risk following lower leg cast immobilization or following knee arthroscopy is feasible by using a risk prediction model. -this thesis- 4. A targeted approach, by identifying high-risk patients who may beneft from a higher dose or longer duration of thromboprophylactic therapy, is a promising next step to prevent symptomatic VTE following lower leg cast immobilization or knee arthroscopy. -this thesis- 5. The best treatment strategy to prevent symptomatic venous thromboembolism following lower leg cast immobilization or following knee arthroscopy is yet to be determined. 6. Prognostic models are meant to assist and not to replace clinicians’ decisions. Accurate estimation of risks of outcomes can enhance informed decision making with the patient. -Adapted from PLoS Med 10(2): e1001381- 7. The frst developed prediction model is not the last. 8. Voor de dagelijkse klinische praktijk is het essentieel dat onderzoeksresultaten op de juiste manier worden geïnterpreteerd en toegepast. Om dit te waarborgen is een intensievere samenwerking tussen epidemiologen en dokters aan te raden. -

Thrombosis and Aspirin: Clinical Aspect, Aspirin in Cardiology, Aspirin in Neurology, and Pharmacology of Aspirin
Thrombosis Thrombosis and Aspirin: Clinical Aspect, Aspirin in Cardiology, Aspirin in Neurology, and Pharmacology of Aspirin Guest Editors: Christian Doutremepuich, Jawad fareed, Jeanine M. Walenga, Jean-Marc Orgogozo, and Marie Lordkipanidzé Thrombosis and Aspirin: Clinical Aspect, Aspirin in Cardiology, Aspirin in Neurology, and Pharmacology of Aspirin Thrombosis Thrombosis and Aspirin: Clinical Aspect, Aspirin in Cardiology, Aspirin in Neurology, and Pharmacology of Aspirin Guest Editors: Christian Doutremepuich, Jawad fareed, Jeanine M. Walenga, Jean-Marc Orgogozo, and Marie Lordkipanidze´ Copyright © 2012 Hindawi Publishing Corporation. All rights reserved. This is a special issue published in “Thrombosis.” All articles are open access articles distributed under the Creative Commons Attribu- tion License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Editorial Board Louis M. Aledort, USA Thomas Kickler, USA Johannes Oldenburg, Germany David Bergqvist, Sweden S. P. Kunapuli, USA Graham F. Pineo, Canada Francis J. Castellino, USA Jose A. Lopez, USA Domenico Prisco, Italy M. Cattaneo, Italy C. A. Ludlam, Uk Karin Przyklenk, USA Beng Hock Chong, Australia Nageswara Madamanchi, USA Ashwini Koneti Rao, USA Frank C. Church, USA Martyn Mahaut-Smith, UK F. R. Rickles, USA Giovanni de Gaetano, Italy P. M . Ma nnu cc i, Ita ly Evqueni Saenko, USA David H. Farrell, USA Osamu Matsuo, Japan Paolo Simioni, Italy Alessandro Gringeri, Italy Keith R. McCrae, USA C. Arnold -

The Approach to Thrombosis Prevention Across the Spectrum of Philadelphia-Negative Classic Myeloproliferative Neoplasms
Review The Approach to Thrombosis Prevention across the Spectrum of Philadelphia-Negative Classic Myeloproliferative Neoplasms Steffen Koschmieder Department of Medicine (Hematology, Oncology, Hemostaseology, and Stem Cell Transplantation), Faculty of Medicine, RWTH Aachen University, Pauwelsstr. 30, D-52074 Aachen, Germany; [email protected]; Tel.: +49-241-8080981; Fax: +49-241-8082449 Abstract: Patients with myeloproliferative neoplasm (MPN) are potentially facing diminished life expectancy and decreased quality of life, due to thromboembolic and hemorrhagic complications, progression to myelofibrosis or acute leukemia with ensuing signs of hematopoietic insufficiency, and disturbing symptoms such as pruritus, night sweats, and bone pain. In patients with essential thrombocythemia (ET) or polycythemia vera (PV), current guidelines recommend both primary and secondary measures to prevent thrombosis. These include acetylsalicylic acid (ASA) for patients with intermediate- or high-risk ET and all patients with PV, unless they have contraindications for ASA use, and phlebotomy for all PV patients. A target hematocrit level below 45% is demonstrated to be associated with decreased cardiovascular events in PV. In addition, cytoreductive therapy is shown to reduce the rate of thrombotic complications in high-risk ET and high-risk PV patients. In patients with prefibrotic primary myelofibrosis (pre-PMF), similar measures are recommended as in those with ET. Patients with overt PMF may be at increased risk of bleeding and thus require a more individualized approach to thrombosis prevention. This review summarizes the thrombotic Citation: Koschmieder, S. The risk factors and primary and secondary preventive measures against thrombosis in MPN. Approach to Thrombosis Prevention across the Spectrum of Keywords: myeloproliferative neoplasms (MPN); polycythemia vera (PV); essential thrombocythemia Philadelphia-Negative Classic (ET); primary myelofibrosis (PMF); thrombosis; prevention; antiplatelet agents; anticoagulation; cy- Myeloproliferative Neoplasms. -

ACTIVASE (Alteplase) for Injection, for Intravenous Use Initial U.S
Application 103172 This document contains: Label for ACTIVASE [Supplement 5203, Action Date 02/13/2015] Also available: Label for CATHFLO ACTIVASE [Supplement 5071, Action Date 01/04/2005] HIGHLIGHTS OF PRESCRIBING INFORMATION Acute Ischemic Stroke These highlights do not include all the information needed to use • Current intracranial hemorrhage. (4.1) ACTIVASE safely and effectively. See full prescribing information for • Subarachnoid hemorrhage. (4.1) ACTIVASE. Acute Myocardial Infarction or Pulmonary Embolism • History of recent stroke. (4.2) ACTIVASE (alteplase) for injection, for intravenous use Initial U.S. Approval: 1987 -----------------------WARNINGS AND PRECAUTIONS----------------------- • Increases the risk of bleeding. Avoid intramuscular injections. Monitor for ---------------------------INDICATIONS AND USAGE-------------------------- bleeding. If serious bleeding occurs, discontinue Activase. (5.1) Activase is a tissue plasminogen activator (tPA) indicated for the treatment of • Monitor patients during and for several hours after infusion for orolingual • Acute Ischemic Stroke (AIS). (1.1) angioedema. If angioedema develops, discontinue Activase. (5.2) • Acute Myocardial Infarction (AMI) to reduce mortality and incidence of • Cholesterol embolism has been reported rarely in patients treated with heart failure. (1.2) thrombolytic agents. (5.3) Limitation of Use in AMI: the risk of stroke may be greater than the benefit • Consider the risk of reembolization from the lysis of underlying deep in patients at low risk of death -
Final Program
In Memoriam: Final Program XXV Congress of the International Society on Thrombosis and Haemostasis and 61st Annual SSC Meeting June 20 – 25, 2015 Toronto, Canada www.isth2015.org 1 Final Program Table of Contents 3 Venue and Contacts 5 Invitation and Welcome Message 12 ISTH 2015 Committees 24 Congress Support 25 Sponsors and Exhibitors 27 ISTH Awards 32 ISTH Society Information 37 Program Overview 41 Program Day by Day 55 SSC and Educational Program 83 Master Classes and Career Mentorship Sessions 87 Nurses Forum 93 Scientific Program, Monday, June 22 94 Oral Communications 1 102 Plenary Lecture 103 State of the Art Lectures 105 Oral Communications 2 112 Abstract Symposia 120 Poster Session 189 Scientific Program, Tuesday, June 23 190 Oral Communications 3 198 Plenary Lecture 198 State of the Art Lectures 200 Oral Communications 4 208 Plenary Lecture 209 Abstract Symposia 216 Poster Session 285 Scientific Program, Wednesday, June 24 286 Oral Communications 5 294 Plenary Lecture 294 State of the Art Lectures 296 Oral Communications 6 304 Abstract Symposia 311 Poster Session 381 Scientific Program, Thursday, June 25 382 Oral Communications 7 390 Plenary Lecture 390 Abstract Symposia 397 Highlights of ISTH 399 Exhibition Floor Plan 402 Exhibitor List 405 Congress Information 406 Venue Plan 407 Congress Information 417 Social Program 418 Toronto & Canada Information 421 Transportation in Toronto 423 Future ISTH Meetings and Congresses 2 427 Authors Index 1 Thank You to Everyone Who Supported the Venue and Contacts 2014 World Thrombosis Day -

State-Of-The-Art Thrombosis Prevention and Treatment
FOREWORD State-of-the-art thrombosis prevention and treatment antagonists are used for longer periods of primary ‘Pulmonary embolism is a and secondary prophylaxis of thrombosis. leading cause of death in Heparins, especially unfractionated, have draw- cancer patients and the risk for backs, including the need for subcutaneous venous thromboembolism is injections and the risk for heparin-induced thrombocytopenia and osteoporosis on long- significantly increased in patients term use. The heparin derivatives requires bind- with solid tumors and ing to antithrombin in order to exert their anti- hematological malignancies.’ coagulant properties. Vitamin K antagonists have a narrow thera- Benjamin Brenner Thrombosis is the leading cause of death in peutic range that necessitates frequent monitoring Rambam Health Care developed countries, with arterial thrombosis of the prothrombin time. The pharmacogenetics Campus, Department of presenting as myocardial infarction, stroke or of the vitamin K epoxide reductase and CYP219 Hematology and Bone Marrow Transplantation, peripheral arterial occlusion. Venous thrombo- genes may be helpful to better define the dose and Haifa, Israel embolism (VTE) is a major cause of mortality the risk for bleeding on vitamin K antagonists [5]. Tel.: +972 4854 3520 worldwide, despite some variations in prevalence These limitations led to the development of Fax: +972 4854 3886 of the disease [1]. While the incidence of VTE numerous new antithrombotic agents during the E-mail: b_brenner@ rambam.health.gov.il increases with aging, it is the leading cause of past decade, and to an ongoing effort by the vascular morbidity in young adults. industry to develop novel anticoagulants with A multitude of risk factors can contribute to improved efficacy and safety profile and better presentation of VTE [2].