ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Safety of Venous Thromboembolism Prophylaxis with Fondaparinux in Ischemic Stroke☆
Thrombosis Research 135 (2015) 249–254 Contents lists available at ScienceDirect Thrombosis Research journal homepage: www.elsevier.com/locate/thromres Regular Article Safety of venous thromboembolism prophylaxis with fondaparinux in ischemic stroke☆ C.T. Hackett a,d,1, R.S. Ramanathan a,1, K. Malhotra a,M.R.Quigleyb,c,K.M.Kellya,c,M.Tiana,J.Protetcha, C. Wong a,c,D.G.Wrighta,c,A.H.Tayala,c,⁎ a Department of Neurology and Allegheny General Hospital Comprehensive Stroke Center, University of South Carolina b Department of Neurosurgery and Allegheny General Hospital, University of South Carolina c Drexel University College of Medicine, University of South Carolina d Department of Psychology, University of South Carolina article info abstract Article history: Introduction: Unfractionated heparin (UFH), low molecular weight heparin or fondaparinux are recommended Received 19 June 2014 for venous thromboembolism (VTE) prophylaxis in acutely ill medical patients. There are limited data on the Received in revised form 11 September 2014 safety of fondaparinux for VTE prophylaxis in ischemic stroke. We examined adverse event frequency in Accepted 4 November 2014 hospitalized patients with ischemic stroke who received VTE prophylaxis with fondaparinux versus UFH. Available online 13 December 2014 Materials and Methods: We performed a propensity score matched analysis on a retrospective cohort of 644 consecutive patients with acute ischemic stroke receiving fondaparinux (n = 322) or UFH (n = 322) for VTE prophylaxis. Patients who received intravenous tPA and continuous intravenous infusions of UFH were excluded. The primary outcome was major hemorrhage (intracranial or extracranial) and the secondary outcome was total hemorrhage (major and minor hemorrhage) during hospitalization. -

Product Monograph
PRODUCT MONOGRAPH PrFONDAPARINUX SODIUM INJECTION 2.5 mg/0.5 mL , 5.0 mg/0.4 mL, 7.5 mg/0.6 mL, and 10.0 mg/0.8 mL Sterile 2.5 mg/0.5 mL (5 mg/mL) 5.0 mg/0.4 mL (12.5 mg/mL) 7.5 mg/0.6 mL (12.5 mg/mL) 10.0 mg/0.8 mL (12.5 mg/mL) Synthetic Antithrombotic DIN Owner: Date of Preparation: Dr. Reddy’s Laboratories Limited July 20, 2012 Bachupally – 500 090 INDIA Date of Revision: November 3, 2014 Canadian Importer/Distributor: Innomar Strategies Inc. 3470 Superior Court- Oakville, Ontario L6L 0C4 CANADA Submission Control Number: 174569 1 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .........................................................3 SUMMARY PRODUCT INFORMATION........................................................................3 INDICATIONS AND CLINICAL USE..............................................................................3 CONTRAINDICATIONS...................................................................................................4 WARNINGS AND PRECAUTIONS..................................................................................4 ADVERSE REACTIONS....................................................................................................9 DRUG INTERACTIONS..................................................................................................22 DOSAGE AND ADMINISTRATION..............................................................................23 OVERDOSAGE................................................................................................................27 -
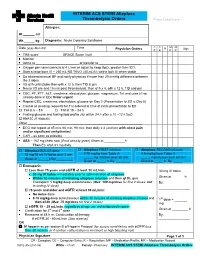
EXAMPLE Alteplase Thrombolytic Central Changes Noted
INTERIM ACS STEMI Alteplase Thrombolysis Orders Place Label Here Allergies: Ht. cm Wt. kg Diagnosis: Acute Coronary Syndrome C C M M Date (yyyy-Mon-dd) Time R Sign Physician Orders P E P R TIMI score ____________ GRACE Score (risk) ____________________ Monitor Admit to or transfer to _______________________ Oxygen per nasal cannula at 4 L/min or adjust to keep SpO2 greater than 92% Start a large bore IV – 250 mL NS TKVO (40 mL/h); saline lock IV when stable Do bilateral manual BP and notify physician if more than 20 mmHg difference between the 2 sides VS q1h until stable then q4h x 12 h, then TID & prn Neuro VS pre and 15 min post thrombolysis, then q1h x 4, q4h x 12 h, TID and prn CBC, PT, PTT, ALT, creatinine, electrolytes, glucose, magnesium, TnI and urea (if not already done in ED) Order urgent Repeat CBC, creatinine, electrolytes, glucose on Day 2 (Presentation to ED is Day 0) Cancel all pending requests for TnI ordered at time of initial presentation to ED TnI at 6 – 8 h TnI at 18 – 24 h Fasting glucose and fasting lipid profile (do within 24 h after a 10 –12 h fast) HbA1C (if diabetic) Other _______________________________________________________________ ECG stat repeat at 45 min, 60 min, 90 min: then daily x 3 (and prn with chest pain and/or significant arrhythmias) CXR – as soon as possible ASA – 162 mg chew now (if not already given) Given at h Then EC ASA 81 mg daily. Alteplase BOLUS dose Alteplase FIRST infusion Alteplase SECOND infusion 15 mg/15 mL IV bolus over 2 min 0.75 mg/kg from Table A 0.5 mg/kg from Table A _____ mg infusion over 30 min _____ mg infusion over 60 min Given at ______h By:_________ Given at _____ h By: ________ Given at _____ h By: _____ Enoxaparin Less than 75 years and eGFR at least 30 mL/min 30 mg IV bolus 30 mg IV bolus immediately prior to administration of alteplase Within 30 minutes of initiating alteplase infusion and then q12h, give Given at _______h Enoxaparin 1 mg/kg deep subcutaneous (Max. -

ACTIVASE (Alteplase) for Injection, for Intravenous Use Initial U.S
Application 103172 This document contains: Label for ACTIVASE [Supplement 5203, Action Date 02/13/2015] Also available: Label for CATHFLO ACTIVASE [Supplement 5071, Action Date 01/04/2005] HIGHLIGHTS OF PRESCRIBING INFORMATION Acute Ischemic Stroke These highlights do not include all the information needed to use • Current intracranial hemorrhage. (4.1) ACTIVASE safely and effectively. See full prescribing information for • Subarachnoid hemorrhage. (4.1) ACTIVASE. Acute Myocardial Infarction or Pulmonary Embolism • History of recent stroke. (4.2) ACTIVASE (alteplase) for injection, for intravenous use Initial U.S. Approval: 1987 -----------------------WARNINGS AND PRECAUTIONS----------------------- • Increases the risk of bleeding. Avoid intramuscular injections. Monitor for ---------------------------INDICATIONS AND USAGE-------------------------- bleeding. If serious bleeding occurs, discontinue Activase. (5.1) Activase is a tissue plasminogen activator (tPA) indicated for the treatment of • Monitor patients during and for several hours after infusion for orolingual • Acute Ischemic Stroke (AIS). (1.1) angioedema. If angioedema develops, discontinue Activase. (5.2) • Acute Myocardial Infarction (AMI) to reduce mortality and incidence of • Cholesterol embolism has been reported rarely in patients treated with heart failure. (1.2) thrombolytic agents. (5.3) Limitation of Use in AMI: the risk of stroke may be greater than the benefit • Consider the risk of reembolization from the lysis of underlying deep in patients at low risk of death -
Protocol-IV-Alteplase.Pdf
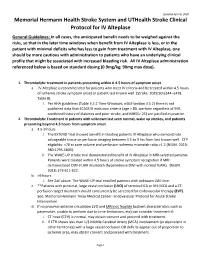
Updated April 6, 2020 Memorial Hermann Health Stroke System and UTHealth Stroke Clinical Protocol for IV Alteplase General Guidelines: In all cases, the anticipated benefit needs to be weighed against the risks, so that in the later time windows when benefit from IV Alteplase is less, or in the patient with minimal deficits who has less to gain from treatment with IV Alteplase, one should be more cautious with administration to patients who have an underlying clinical profile that might be associated with increased bleeding risk. All IV Alteplase administration referenced below is based on standard dosing (0.9mg/kg; 90mg max dose). 1. Thrombolytic treatment in patients presenting within 0-4.5 hours of symptom onset. a. IV Alteplase is recommended for patients who meet IV criteria and be treated within 4.5 hours of ischemic stroke symptom onset or patient last known well. (Stroke. 2019;50:e344–e418. Table 8). i. Per AHA guidelines (Table 3.5.2 Time Windows; e363-Section 3.5.2) there is not published data that ECASS III exclusion criteria (age > 80, warfarin regardless of INR, combined history of diabetes and prior stroke, and NIHSS> 25) are justified in practice. 2. Thrombolytic Treatment in patients with unknown last seen normal, wake up strokes, and patients presenting beyond 4.5 hours from symptom onset. a. 4.5-9 hours i. The EXTEND Trial showed benefit in treating patients IV Alteplase who demonstrate salvageable tissue on perfusion imaging between 4.5 to 9 hrs from last known well. CTP eligibility: <70 cc core volume and perfusion-ischemia mismatch ratio >1.2 (NEJM. -

LOW MOLECULAR WEIGHT HEPARIN and FONDAPARINUX Zachary Stacy and Sara K
4 Chapter LOW MOLECULAR WEIGHT HEPARIN AND FONDAPARINUX Zachary Stacy and Sara K. Richter INTRODUCTION The low molecular weight heparins (LMWHs) and the synthetic pentasaccharide, fondaparinux, offer several advantages over unfractionated heparin (UFH). Enoxa- parin and dalteparin were approved in the United States in 1993 and 1994, respec- tively, followed by fondaparinux in 2001. Tinzaparin was approved and available in 2000, but was subsequently withdrawn from the market in 2011. These injectables have been traditionally used as prophylaxis for venous thromboembolism or as a bridge therapy to therapeutic oral anticoagulation. Based on their relative ease of dosing and monitoring, these agents frequently replace UFH in many clinical situations. This chapter will focus on those agents currently available in the United States, including enoxaparin, dalteparin, and fondaparinux. PHARMACOLOGY AND PHARMACOKINETICS1-9 Traditionally, unfractionated heparin was the parenteral anticoagulant used in the inpatient setting. Active unfractionated heparin compounds are composed of an inconsistent number of sugars, each ending in a specific pentasaccharide sequence. Using a consistent and shorter sequence of sugars improved the variability in the anticoagulant effect, giving rise to fractioned LMWH products. Mechanism of Action • LMWHs and fondaparinux are indirect inhibitors of clotting factors requiring antithrom- bin to exert an anticoagulant effect (Figure 4-1). • A specific pentasaccharide sequence binds to antithrombin to potentiate its activity. • LMWHs inhibit both Factor Xa and IIa (thrombin) activity. • Fondaparinux selectively inhibits only Factor Xa. • Refer to Tables 4-1 and 4-2 for comparison of the specific clotting factors inhibited. 65 66 Anticoagulation Therapy AT AT AT X a AT Thro mbin UFH AT AT X a AT Thro mbin LMWH Xa AT AT AT Throm bin Fondaparinux FIGURE 4-1. -

Transition of Anticoagulants 2019
Transition of Anticoagulants 2019 Van Hellerslia, PharmD, BCPS, CACP, Brand Generic Clinical Assistant Professor of Pharmacy Practice, Angiomax bivalirudin Temple University School of Pharmacy, Philadelphia, PA Arixtra fondaparinux Bevyxxa betrixaban Pallav Mehta, MD, Assistant Professor of Medicine, Coumadin warfarin Division of Hematology/Oncology, Eliquis apixaban MD Anderson Cancer Center at Cooper, Camden, NJ Fragmin dalteparin Lovenox enoxaparin Reviewer: Kelly Rudd, PharmD, BCPS, CACP, Pradaxa dabigatran Clinical Specialist, Anticoagulation, Bassett Medical Center, Savaysa edoxaban Cooperstown, NY Xarelto rivaroxaban From To Action Apixaban Argatroban/ Wait 12 hours after last dose of apixaban to initiate parenteral anticoagulant. In cases of Bivalirudin/ high bleeding risk, consider omitting initial bolus when transitioning to heparin infusion. Enoxaparin/ Dalteparin/ Fondaparinux/ Heparin Apixaban Warfarin When going from apixaban to warfarin, consider the use of parenteral anticoagulation as a bridge (eg, start heparin infusion or therapeutic enoxaparin AND warfarin 12 hours after last dose of apixaban and discontinue parenteral anticoagulant when INR is therapeutic). Apixaban affects INR so that initial INR measurements during the transition may not be useful for determining the appropriate dose of warfarin. Apixaban Betrixaban, Wait 12 hours from last dose of apixaban to initiate betrixaban, dabigatran, edoxaban, or Dabigatran, rivaroxaban. Edoxaban, or Rivaroxaban Argatroban Apixaban, Start apixaban, betrixaban, dabigatran, -

The Treatment and Prevention Ofacute Ischemic Stroke
EDITORIAL Alvaro Nagib Atallah* The treatment and prevention of acute ischemic stroke rotecting the brain from the consequences .of alternated with placebo (lower dose) and placebo injections vascular obstruction is obviously very important. every 12 hours, for 10 days. The evaluation at 6 months PHowever, how to manage this is a very complex showed that the treated group had a lower incidence rate task. Three recent studies have provided evidence that of poor outcomes, death or dependency in daily activities, I 3 should not be ignored or misinterpreted by physicians. - 45 vs. 65%. In other words, it was necessary to treat 5 The National Institute of Neurological Disorders and patients to benefit one. Evaluations at 10 days did not show Stroke rt-PA Stroke Study Groupl shows the results of a differences in death rates or haemorrhage transformation randomized, collaborative placebo-controlled trial. Six of the cerebral infarction. hundred and twenty-four patients were studied. The The Multicentre Acute Stroke Trial-Italy (MAST-I) treatment was started before 90' of the start of the stroke Group compared the effectiveness of streptokinase, aspirin or before 180'. Patients received recombinant rt-PA and a combination of both for the treatment of ischemic (alteplase) 0.9 mg/kg or placebo. A careful neurological stroke. Six hundred and twenty-two patients were evaluation was done at 24 hours and 3 months after the randomized to receive I hour infusions of 1.5 mD of stroke. streptokinase alone, the same dose of streptokinase plus There were no significant differences between the 300 mg of buffered aspirin, or 300 mg of aspirin alone for groups at 24 hours after the stroke. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Fondaparinux
Development of a Synthetic Heparin Pentasaccharide: Fondaparinux Jeanine M. WALENGA*, Jawed FAREED*, Walter P. JESKE*, F. Xavier FRAPAISE*, Rodger L. BICK**, M. Michel SAMAMA*** * Department of Pathology, Loyola University Medical Center, 2160 S. First Avenue, Maywood, Illinois 60153, ** Medical School, University of Texas Southwestern, 8210 Walnut Hill Lane, Suite 604, Dallas, Texas 7523, USA *** Laboratoire Central D’Hematologie, Hôtel-Dieu, 1, Place du Parvis Notre-Dame, 75181 Paris, FRANCE ABSTRACT Fondaparinux (Arixtra®; Sanofi-Synthélabo/Organon) is the first of a new class of antithrombotic agents dis- tinct from low molecular weight (LMW) heparins and heparin. It is a synthetic pentasaccharide mimicking the si- te of heparin that binds to antithrombin III (AT). It is homogeneous with a molecular weight of 1728 Da. It exhi- bits only factor (F) Xa inhibitor activity via binding to AT, which in turn inhibits thrombin generation. It does not inhibit thrombin, release TFPI, or possess other actions of heparin. Low AT levels can limit the efficacy of fonda- parinux. There is nearly complete bioavailability subcutaneously, rapid onset of action, a prolonged half-life (15- 20 h) and no metabolism preceding renal excretion. Elderly and renal impaired patients have reduced clearance. The PT, aPTT and ACT are not affected by fondaparinux; anti-FXa assays are used if needed. Phase IIb clinical studies have identified a fixed dose of 2.5 mg once daily for prophylaxis of venous thrombosis without monitoring. Four phase III studies (n > 7000) demonstrated a combined 55% relative risk reduction of venous thromboembo- lic events in orthopedic surgery patients in comparison to the LMW heparin enoxaparin. -

Arixtra, INN-Fondaparinux
London, 29 August 2007 Product Name: Arixtra EMEA/H/C/403/II/24 SCIENTIFIC DISCUSSION ©EMEA 2007 I. SCIENTIFIC DISCUSSION 1.1. Introduction The company is requesting the following new indication in the treatment of Acute Coronary Syndromes (ACS) for Arixtra 2.5 mg: Treatment of unstable angina or non-ST segment elevation myocardial infarction (UA/NSTEMI) ACS for the prevention of death, myocardial infarction and refractory ischaemia. Fondaparinux has been shown to reduce all cause mortality in patients with UA/NSTEMI. Treatment of ST segment elevation myocardial infarction (STEMI) ACS for the prevention of death and myocardial re-infarction in patients who are managed with thrombolytics or who initially are to receive no other form of reperfusion therapy. Fondaparinux has been shown to reduce all cause mortality in patients with STEMI. As a consequence of the requested new indication, the MAH is also applying for major changes to sections 4.2 (posology) and 5.1 (Pharmacodynamic properties), and other changes in 4.3, 4.4, 4.8, 5.2 and section 6 of the SPC. In order to treat the STEMI subset of ACS patients, the MAH is also applying for the approval of a new route of administration, namely intravenous, for the already existing 2.5 mg pre-filled syringe. This requested change is being processed through a separate Line Extension application (EMEA/H/C/403/X/25), and the details thereof will not be further discussed in this report. The application is based on 2 large phase III pivotal studies (OASIS 5 and OASIS 6) and 4 phase II supportive trials. -

In Vivo Effects of Contrast Media on Coronary Thrombolysis
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector 1102 JACC Vol. 32, No. 4 October 1998:1102–8 In Vivo Effects of Contrast Media on Coronary Thrombolysis SORIN PISLARU, MD, PHD,*† CRISTINA PISLARU, MD,* MONIKA SZILARD, MD,* JEF ARNOUT, PHD,‡ FRANS VAN DE WERF, MD, PHD, FACC* Leuven, Belgium and Bucharest, Romania Objectives. The aim of the present study was to evaluate the associated with longer reperfusion delays (time to optimal reper- influence of radiographic contrast media (CM) on alteplase- fusion: 67 6 48 min and 65 6 49 min, respectively, vs. 21 6 11 min induced coronary thrombolysis. after placebo; p < 0.05) and shorter periods of coronary perfusion Background. Contrast media inhibit fibrinolysis in vitro and (optimal perfusion time: 21 6 26 min and 21 6 28 min, respec- interact with endothelial cells, platelets and the coagulation tively, vs. 58 6 40 min after placebo; p < 0.05). No significant system. The in vivo effects of CM on thrombolysis are not known. differences were observed between groups with regard to activated Methods. Occlusive coronary artery thrombosis was induced in partial thromboplastin times, circulating thrombin-antithrombin 4 groups of 10 dogs by the copper coil technique. After 70 min of III complex concentrations and fibrinogen. occlusion the dogs were randomized to intracoronary injection of Conclusions. In this animal model administration of iohexol 2 2mlkg 1 of either saline, a low-osmolar ionic CM (ioxaglate), a and amidotrizoate before thrombolysis significantly delayed low-osmolar nonionic CM (iohexol) or a high-osmolar ionic CM reperfusion.