Protocol-IV-Alteplase.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
EXAMPLE Alteplase Thrombolytic Central Changes Noted
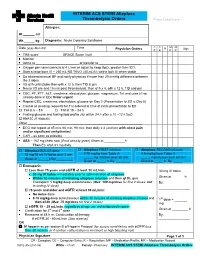
INTERIM ACS STEMI Alteplase Thrombolysis Orders Place Label Here Allergies: Ht. cm Wt. kg Diagnosis: Acute Coronary Syndrome C C M M Date (yyyy-Mon-dd) Time R Sign Physician Orders P E P R TIMI score ____________ GRACE Score (risk) ____________________ Monitor Admit to or transfer to _______________________ Oxygen per nasal cannula at 4 L/min or adjust to keep SpO2 greater than 92% Start a large bore IV – 250 mL NS TKVO (40 mL/h); saline lock IV when stable Do bilateral manual BP and notify physician if more than 20 mmHg difference between the 2 sides VS q1h until stable then q4h x 12 h, then TID & prn Neuro VS pre and 15 min post thrombolysis, then q1h x 4, q4h x 12 h, TID and prn CBC, PT, PTT, ALT, creatinine, electrolytes, glucose, magnesium, TnI and urea (if not already done in ED) Order urgent Repeat CBC, creatinine, electrolytes, glucose on Day 2 (Presentation to ED is Day 0) Cancel all pending requests for TnI ordered at time of initial presentation to ED TnI at 6 – 8 h TnI at 18 – 24 h Fasting glucose and fasting lipid profile (do within 24 h after a 10 –12 h fast) HbA1C (if diabetic) Other _______________________________________________________________ ECG stat repeat at 45 min, 60 min, 90 min: then daily x 3 (and prn with chest pain and/or significant arrhythmias) CXR – as soon as possible ASA – 162 mg chew now (if not already given) Given at h Then EC ASA 81 mg daily. Alteplase BOLUS dose Alteplase FIRST infusion Alteplase SECOND infusion 15 mg/15 mL IV bolus over 2 min 0.75 mg/kg from Table A 0.5 mg/kg from Table A _____ mg infusion over 30 min _____ mg infusion over 60 min Given at ______h By:_________ Given at _____ h By: ________ Given at _____ h By: _____ Enoxaparin Less than 75 years and eGFR at least 30 mL/min 30 mg IV bolus 30 mg IV bolus immediately prior to administration of alteplase Within 30 minutes of initiating alteplase infusion and then q12h, give Given at _______h Enoxaparin 1 mg/kg deep subcutaneous (Max. -

ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent
ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent ). Indications: - Management of acute myocardial infarction for the lysis of thrombi in coronary arteries; management of acute ischemic stroke -Acute myocardial infarction (AMI): Chest pain ≥20 minutes, ≤12-24 hours; S-T elevation ≥0.1 mV in at least two ECG leads -Acute pulmonary embolism (APE): Age ≤75 years: Documented massive pulmonary embolism by pulmonary angiography or echocardiography or high probability lung scan with clinical shock . -Restoration of central venous catheter function *Unlabeled/Investigational :Acute peripheral arterial occlusive disease. Dosage: -Coronary artery thrombi: Front loading dose (weight-based): -Patients >67 kg: Total dose: 100 mg over 1.5 hours; infuse 15 mg over 1-2 minutes. Infuse 50 mg over 30 minutes. Infuse remaining 35 mg of alteplase over the next hour. Maximum total dose: 100 mg -Patients ≤67 kg: Infuse 15 mg I.V. bolus over 1-2 minutes, then infuse 0.75 mg/kg (not to exceed 50 mg) over next 30 minutes, followed by 0.5 mg/kg over next 60 minutes (not to exceed 35 mg) Maximum total dose: 100 mg. See “Notes.” Note: Concurrently, begin heparin 60 units/kg bolus (maximum: 4000 units) followed by continuous infusion of 12 units/kg/hour (maximum: 1000 units/hour) and adjust to aPTT target of 1.5-2 times the upper limit of control. Note: Thrombolytic should be administered within 30 minutes of hospital arrival. Administer concurrent aspirin, clopidogrel, and anticoagulant therapy (ie, unfractionated heparin, enoxaparin, or fondaparinux) with alteplase (O’Gara, 2013). -Acute massive or submassive pulmonary embolism: I.V. (Activase®): 100 mg over 2 hours; may be administered as a 10 mg bolus followed by 90 mg over 2 hours as was done in patients with submassive PE (Konstantinides, 2002). -

ACTIVASE (Alteplase) for Injection, for Intravenous Use Initial U.S
Application 103172 This document contains: Label for ACTIVASE [Supplement 5203, Action Date 02/13/2015] Also available: Label for CATHFLO ACTIVASE [Supplement 5071, Action Date 01/04/2005] HIGHLIGHTS OF PRESCRIBING INFORMATION Acute Ischemic Stroke These highlights do not include all the information needed to use • Current intracranial hemorrhage. (4.1) ACTIVASE safely and effectively. See full prescribing information for • Subarachnoid hemorrhage. (4.1) ACTIVASE. Acute Myocardial Infarction or Pulmonary Embolism • History of recent stroke. (4.2) ACTIVASE (alteplase) for injection, for intravenous use Initial U.S. Approval: 1987 -----------------------WARNINGS AND PRECAUTIONS----------------------- • Increases the risk of bleeding. Avoid intramuscular injections. Monitor for ---------------------------INDICATIONS AND USAGE-------------------------- bleeding. If serious bleeding occurs, discontinue Activase. (5.1) Activase is a tissue plasminogen activator (tPA) indicated for the treatment of • Monitor patients during and for several hours after infusion for orolingual • Acute Ischemic Stroke (AIS). (1.1) angioedema. If angioedema develops, discontinue Activase. (5.2) • Acute Myocardial Infarction (AMI) to reduce mortality and incidence of • Cholesterol embolism has been reported rarely in patients treated with heart failure. (1.2) thrombolytic agents. (5.3) Limitation of Use in AMI: the risk of stroke may be greater than the benefit • Consider the risk of reembolization from the lysis of underlying deep in patients at low risk of death -

The Treatment and Prevention Ofacute Ischemic Stroke
EDITORIAL Alvaro Nagib Atallah* The treatment and prevention of acute ischemic stroke rotecting the brain from the consequences .of alternated with placebo (lower dose) and placebo injections vascular obstruction is obviously very important. every 12 hours, for 10 days. The evaluation at 6 months PHowever, how to manage this is a very complex showed that the treated group had a lower incidence rate task. Three recent studies have provided evidence that of poor outcomes, death or dependency in daily activities, I 3 should not be ignored or misinterpreted by physicians. - 45 vs. 65%. In other words, it was necessary to treat 5 The National Institute of Neurological Disorders and patients to benefit one. Evaluations at 10 days did not show Stroke rt-PA Stroke Study Groupl shows the results of a differences in death rates or haemorrhage transformation randomized, collaborative placebo-controlled trial. Six of the cerebral infarction. hundred and twenty-four patients were studied. The The Multicentre Acute Stroke Trial-Italy (MAST-I) treatment was started before 90' of the start of the stroke Group compared the effectiveness of streptokinase, aspirin or before 180'. Patients received recombinant rt-PA and a combination of both for the treatment of ischemic (alteplase) 0.9 mg/kg or placebo. A careful neurological stroke. Six hundred and twenty-two patients were evaluation was done at 24 hours and 3 months after the randomized to receive I hour infusions of 1.5 mD of stroke. streptokinase alone, the same dose of streptokinase plus There were no significant differences between the 300 mg of buffered aspirin, or 300 mg of aspirin alone for groups at 24 hours after the stroke. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

In Vivo Effects of Contrast Media on Coronary Thrombolysis
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector 1102 JACC Vol. 32, No. 4 October 1998:1102–8 In Vivo Effects of Contrast Media on Coronary Thrombolysis SORIN PISLARU, MD, PHD,*† CRISTINA PISLARU, MD,* MONIKA SZILARD, MD,* JEF ARNOUT, PHD,‡ FRANS VAN DE WERF, MD, PHD, FACC* Leuven, Belgium and Bucharest, Romania Objectives. The aim of the present study was to evaluate the associated with longer reperfusion delays (time to optimal reper- influence of radiographic contrast media (CM) on alteplase- fusion: 67 6 48 min and 65 6 49 min, respectively, vs. 21 6 11 min induced coronary thrombolysis. after placebo; p < 0.05) and shorter periods of coronary perfusion Background. Contrast media inhibit fibrinolysis in vitro and (optimal perfusion time: 21 6 26 min and 21 6 28 min, respec- interact with endothelial cells, platelets and the coagulation tively, vs. 58 6 40 min after placebo; p < 0.05). No significant system. The in vivo effects of CM on thrombolysis are not known. differences were observed between groups with regard to activated Methods. Occlusive coronary artery thrombosis was induced in partial thromboplastin times, circulating thrombin-antithrombin 4 groups of 10 dogs by the copper coil technique. After 70 min of III complex concentrations and fibrinogen. occlusion the dogs were randomized to intracoronary injection of Conclusions. In this animal model administration of iohexol 2 2mlkg 1 of either saline, a low-osmolar ionic CM (ioxaglate), a and amidotrizoate before thrombolysis significantly delayed low-osmolar nonionic CM (iohexol) or a high-osmolar ionic CM reperfusion. -

General Catheter Management Brochure
Adult Catheter Management Brochure Hold ourselves accountable to the standard of care Use evidence-based guidelines to deliver quality care to patients with central lines Central venous access devices (CVADs) deliver life-sustaining therapies An evidence-based list of indications for CVAD use includes but is not limited to1: Clinical instability of the patient and/or complexity of infusion regimen 1 (multiple infusates) 2 Episodic chemotherapy treatment Prescribed continuous infusion therapy (eg, parenteral nutrition, fluid and 3 electrolytes, medications) 4 Invasive hemodynamic monitoring Long-term intermittent infusion therapy (eg, any medication including 5 anti-infectives in patients with a known or suspected infection) History of failed or difficult peripheral venous access, if use of ultrasound 6 guidance has failed Catheters can be used either short or long term for the infusion of 2,3: • Antibiotics • Parenteral nutrition • Medication/solutions in patients with limited peripheral access • Chemotherapy or other vesicant or irritating solutions • Blood and blood products • Therapy that is ongoing or continued at home 2 catheter management Why is it important to ensure central line patency? An occluded line may complicate patient care by3-5: • Disrupting therapies or delaying procedures • Interrupting administration of medications and solutions • Delays in discharge • Additional procedures, such as catheter replacement “Foster a just culture and individual accountability through a focus on improving systems and processes by clinicians and leaders.”1 INS Infusion Therapy Standards of Practice, 2021, page S31, standard 6A “Catheter salvage is preferred over catheter removal for management of CVAD occlusion with choice of clearing agents based on a thorough assessment of potential causes of occlusion.” INS Infusion Therapy Standards of Practice, 2021, page S149, standard 49.2 INS=Infusion Nurses Society. -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

Cleveland Clinic Anticoagulation Management Program (C-Camp)
CLEVELAND CLINIC ANTICOAGULATION MANAGEMENT PROGRAM (C-CAMP) 1 Table of Contents I. EXECUTIVE SUMMARY ......................................................................................................................................... 6 II. VENOUS THROMBOEMBOLISM RISK ASSESSMENT AND PROPHYLAXIS ............................................. 9 III. RECOMMENDED PROPHYLAXIS OPTIONS FOR THE PREVENTION OF VENOUS THROMBOEMBOLISM. ........................................................................................................................................ 10 IIIA. RECOMMENDED PROPHYLAXIS OPTIONS FOR THE PREVENTION OF VENOUS THROMBOEMBOLISM BASED ON RISK FACTOR ASSESSMENT ............................................................. 12 A) UNFRACTIONATED HEPARIN (UFH) ................................................................................................................... 14 B) LOW MOLECULAR WEIGHT HEPARIN (LMWH) ENOXAPARIN (LOVENOX®) .............................................. 14 C) FONDAPARINUX/ (ARIXTRA®) …………………………………………………………………………..……16 D) RIVAROXABAN (XARELTO®) .......................................................................................................................... 16 E) DESIRUDIN (IPRIVASK®)………………………………………………………………………………..…….17 F) WARFARIN/COUMADIN®) ............................................................................................................................... 16 G) ASPIRIN……………………………………………………………………………………………………..……18 H) INTERMITTENT PNEUMATIC COMPRESSION DEVICES ..................................................................................... -
A Review of the Exclusion Criteria for IV Rtpa for Acute Ischaemic Stroke
A Review of the Exclusion Criteria for IV rtPA for Acute Ischaemic Stroke Dr Gary Pratt Consultant Stroke Physician Sheffield Teaching Hospitals Background • Criteria from NINDs trial – expert consensus • Great deal of experience since – RCT’s /registry data/case series • Evidence for IV thrombolysis has strengthened over time • Rationale for avoiding therapy has reduced • Low rates of thrombolysis – multifactorial but at least in part due to exclusion criteria • AHA updated guidelines 2015 • Time for us regionally to review Agenda • Stroke severity – severe/mild • Resolving • Early ischemic change on CT imaging • Recent bleeding • Blood glucose • INR • DOAC usage • Previous ICH • Intracranial aneurysms • Malignancy Stroke Severity Severe • Original FDA label, risks may be increased with NIHSS >22 • NINDS – max NIHSS 37 (few with NIHSS > 25) Mild stroke predicted good outcome but significant effect seen in strokes with NIHSS > 20. • ECASS excluded pts with NIHSS >25 Stroke Severity Severe Pts achieving primary endpoint (alive and independent) Stroke Severity Severe Recommendations • Increased risk of haemorrhage should not be used as a reason not to treat. • On the basis of available literature there should be no upper limit of NIHSS score for pts otherwise eligible for tPA within 3hrs • FDA label has removed stroke severity (either “too mild” or NIHSS > 22) Stroke Severity Mild • Disability among “mild” stroke pts is significant – not just motor - further stroke - deterioration - disability from problems not picked up on NIHSS • Prediction difficult • Risk of haemorrhagic transformation low • Few mild pts in clinical trials therefore risk to benefit ratio unknown • A number of case series and small clinical trials to suggest there may be benefit from thrombolysis especially if have vessel occlusion. -

Protocols for Anticoagulant and Thrombolytic Therapy Mar 2020
PROTOCOLS FOR ANTICOAGULANT AND THROMBOLYTIC THERAPY Written by Drs. Evan Shereck and John Wu, Division of Hematology/Oncology/BMT and Alison MacDonald, pharmacist References: • Antithrombotic Therapy. In: The 2009 Formulary of the Hospital for Sick Children, 11th edition. Toronto 2008. rd • Monagle P et al (eds). Andrew’s Pediatric Thromboembolism and Stroke 3 ed. 2006; BC Decker Inc. Hamilton. • Monagle P et al. Antithrombotic therapy in neonates and children: ACCP evidence-based clinical practice guidelines (8th edition). Chest 2008; 133: 887S-968S • Malowwany JI, Monagle P, Wu J et al. Enoxaparin for neonatal thrombosis: A call for a higher dose for neonates. Thrombosis Research 2008; 122: 826-30. Contents: Protocol for heparin therapy………………………….……………………….page 2 Protocol for warfarin therapy………..……………………………..………….page 3 Protocol for enoxaparin therapy………………………….……………..…….page 4 Protocol for systemic thrombolytic therapy………………………………….page 6 Heparin Information Sheet ………………………….…………….………….page 7 Warfarin Information Sheet………………………….………………….…….page 8 Enoxaparin Information Sheet……………………………………………..….page 10 Information sheet for thrombolytic therapy………….……………………….page 12 Protocols for Anticoagulant and Thrombolytic Therapy 1 PROTOCOL FOR HEPARIN THERAPY (for patients > 1 month of age) • Always obtain baseline PT/INR, APTT, CBC and fibrinogen before starting therapy • Once APTT is in the therapeutic range, repeat APTT daily; CBC and platelets are to be checked twice weekly LOADING DOSE: 75 units/kg (maximum: 5000 units/dose) -infuse IV over 10 minutes by syringe pump INITIAL MAINTENANCE DOSE: < 1 year of age: 28 units/kg/hr > 1 year of age: 20 units/kg/hr Adolescents and adults 18 units/kg/hr (maximum 1000 units/hr) Obtain APTT 4 hours after loading dose and adjust dose according to nomogram. -

Inclusions and Exclusions for IV
Inclusion and Exclusion Criteria for IV Alteplase (tissue plasminogen activator, IV-tPA) Treatment of Ischemic Stroke For consideration of eligibility within 0-4.5 hours of Time Last Known Well INCLUSION CRITERIA – Patients who should receive IV alteplase □ Symptoms suggestive of ischemic stroke that are deemed to be disabling, regardless of improvement (See Reference Table at end of document) □ Able to initiate treatment within 4.5 hours of Time Last Known Well (document clock time) □ Age 18 years or older EXCLUSION CRITERIA – If patient has any of these, do not initiate IV alteplase □ CT scan demonstrating intracranial hemorrhage □ CT exhibits extensive regions (> 1/3 MCA Territory on CT) of clear hypoattenuation □ Unable to maintain BP <185/110 despite aggressive antihypertensive treatment □ Blood glucose <50 mg/dL (however should treat if stroke symptoms persist after glucose normalized) □ Laboratory (results not required before treatment unless patient is on anticoagulant therapy or there is another reason to suspect the patient may have an abnormality): o INR >1.7 o Platelet count <100,000 o PT >15 sec o aPTT >40 sec □ Medications: o **Full dose low molecular weight heparin (LMWH) within last 24 hours (patients on prophylactic dose of LMWH should NOT be excluded) o Received novel oral anticoagulant (NOAC) within last 48 hours (assuming normal renal metabolizing function) o Commonly prescribed NOACs: apixaban (Eliquis), dabigatran (Pradaxa), rivaroxaban (Xarelto), edoxaban (Savaysa) □ Severe head trauma within last 3 months □ Active