Inclusions and Exclusions for IV
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Interindividual Variability of Apixaban Plasma Concentrations: Influence of Clinical and Genetic Factors in a Real-Life Cohort O
G C A T T A C G G C A T genes Article Interindividual Variability of Apixaban Plasma Concentrations: Influence of Clinical and Genetic Factors in a Real-Life Cohort of Atrial Fibrillation Patients Adela-Nicoleta Ro¸sian 1,2, ¸StefanHoria Ro¸sian 2,3,* , Bela Kiss 4 , Maria Georgia ¸Stefan 4, Adrian Pavel Trifa 5, Camelia Diana Ober 2, Ovidiu Anchidin 2 and Anca Dana Buzoianu 1 1 Department of Pharmacology, Toxicology and Clinical Pharmacology, Iuliu Ha¸tieganuUniversity of Medicine and Pharmacy Cluj-Napoca, 400337 Cluj-Napoca, Romania; [email protected] (A.-N.R.); [email protected] (A.D.B.) 2 “Niculae Stăncioiu” Heart Institute Cluj-Napoca, 400001 Cluj-Napoca, Romania; [email protected] (C.D.O.); [email protected] (O.A.) 3 Department of Cardiology, Heart Institute, Iuliu Ha¸tieganuUniversity of Medicine and Pharmacy Cluj-Napoca, 400001 Cluj-Napoca, Romania 4 Department of Toxicology, Faculty of Pharmacy, Iuliu Ha¸tieganuUniversity of Medicine and Pharmacy Cluj-Napoca, 400349 Cluj-Napoca, Romania; [email protected] (B.K.); [email protected] (M.G.¸S.) 5 Department of Genetics, Iuliu Ha¸tieganuUniversity of Medicine and Pharmacy Cluj-Napoca, 400349 Cluj-Napoca, Romania; [email protected] * Correspondence: [email protected]; Tel.: +4026-459-1224 Received: 11 March 2020; Accepted: 14 April 2020; Published: 17 April 2020 Abstract: (1) Background: Prescribing apixaban for stroke prevention has significantly increased in patients with non-valvular atrial fibrillation (NVAF). The ABCB1 genotype can influence apixaban absorption and bioavailability. The aim of the present study was to assess the factors that influence apixaban’s plasma level and to establish if a certain relationship has clinical relevance. -
Clinical Protocol
CLINICAL PROTOCOL Subject: Page Protocol # EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND 1 of 4 NMH CCP 07.0024 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL ANTICOAGULANTS Version: 1.0 Title: Revision of: Effective Date: EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND NEW 04/29/2013 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL Removal Date: ANTICOAGULANT APIXABAN (ELIQUIS) I. PURPOSE: To standardize management of patients with bleeding and clotting emergencies who are taking novel oral anticoagulants (NOACs). This protocol covers emergent reversal and ischemic stroke in patients on apixaban (Eliquis) therapy. II. CLINICAL PROTOCOL: A. The NOAC apixaban (Eliquis) is FDA approved for stroke prevention in patients with atrial fibrillation. This agent presents clinicians with several challenges because there are no specific antidotes, and no readily available quantitative assay to determine the degree of anticoagulation in a patient on this therapy. B. Patients taking this agent are likely to present to the hospital with; 1. life-threatening bleeding (e.g., intracerebral hemorrhage or GI bleeding), or a need for an emergent invasive procedure (surgery, cardiac Catherization) 2. acute ischemic stroke. The administration of tissue plasminogen activator (IV tPA) in the setting of NOAC use is potentially dangerous. C. There are no accepted evidence-based guidelines for managing these situations. This protocol is a consensus of clinicians from stroke, neurology, neurosurgery, hematology, neurocritical care, laboratory medicine, cardiology, and pharmacy. III. REVERSAL PROTOCOL FOR PATIENTS WITH SEVERE/LIFE-THREATENING BLEEDING TAKING APIXABAN (ELIQUIS) A. Inclusion criteria: 1. Patient has taken any dose of apixaban within last 48 hours. a. If time of last dose is unknown, but patient is suspected of having taken apixaban in last 48 hours, and PT is abnormal and 2. -
STUDY PROTOCOL Study Information Title Apixaban Drug
Apixaban B0661076NON-INTERVENTIONAL STUDY PROTOCOL Final, 15-Feb-2016 NON-INTERVENTIONAL (NI) STUDY PROTOCOL Study information Title Apixaban drug utilization study in Stroke prevention in atrial fibrillation (SPAF) Protocol number B0661076 AEMPS Code PFI-API-2016-01 Protocol version identifier 4.0 Date of last version of protocol 15-Feb-2016 Active substance Apixaban B01AF02 Medicinal product Eliquis® Research question and objectives Evaluate the apixaban utilization according to the approved SPAF indication and recommendations by EMA. The study objectives are: Objective 1: To characterise patients using apixaban according to demographics, comorbidity, risk of thromboembolic events (CHADS2 and CHA2DS2-Vasc scores), risk of bleeding events (HAS-BLED score), comedications and compare it with the profile of patients treated with VKA, dabigatran and rivaroxaban. Objective 2: Describe the level of appropriate usage according to the posology recommended in the apixaban SmPC. Objective 3: Describe the potential interactions with other drugs prescribed concomitantly according with the SmPC recommendations. Objective 4: Estimate the level of apixaban adherence by the medication possession ratio (MPR) and discontinuation rates and compare it with VKA, dabigatran and CT24-GSOP-RF03 NI Study Protocol Template; Version 3.0, Effective Date 10-Oct-2014 Pfizer Confidential Page 1 of 28 Apixaban B0661076NON-INTERVENTIONAL STUDY PROTOCOL Final, 15-Feb-2016 rivaroxaban cohort. Objective 5: To analyze INR (International Normalized Ratio) values during the last 12 months and to obtain TTR (Time in Therapeutic Range) values in patients previously treated with VKA and, during the whole study period for those in the cohort treated with VKA Author Ángeles Quijada Manuitt, IDIAP Jordi Gol Rosa Morros Pedrós, IDIAP Jordi Gol Jordi Cortés, IDIAP Jordi Gol José Chaves Puertas, Pfizer SLU Sponsor Pfizer S.L.U Avda. -

Standard-Dose Apixaban After Very Low-Dose Thrombolysis for Acute Intermediate-High Risk Acute Pulmonary Embolism
SAFE-LYSE | STUDY PROTOCOL Standard-dose Apixaban AFtEr Very Low-dose ThromboLYSis Title: for Acute Intermediate-high Risk Acute Pulmonary Embolism Short Title: SAFE-LYSE Protocol Version: Issue Date: 28/AUG/2019 Principal Victor Tapson1,2, Aaron Weinberg1,2 Investigators: Sub Investigators: Sam Torbati1, Susan Jackman1, Niree Hindoyan1, Joseph Meza1 1Cedars-Sinai Medical Center 8700 Beverly Blvd Los Angeles, CA 90048 Affiliations: 2Cedars-Sinai Medical GrouP 200 N. Robertson Blvd. Beverly Hills, CA 90211 Victor TaPson 8730 Alden Drive, W155 Primary Contact: Los Angeles, CA 90048 (919) 971-6441 Investigator-Initiated Bristol-Myers Squibb Company (BMS) Study Funded By: Version 8.0 | Date: 28Aug2019 1 SAFE-LYSE | STUDY PROTOCOL STUDY SYNOPSIS Funding Provided by BMS/Pfizer Alliance Standard-dose Apixaban AFtEr Very Low-dose ThromboLYSis for Protocol Title Acute Intermediate-high Risk Acute Pulmonary Embolism (SAFE-LYSE) Pulmonary embolism (PE) is a major cause of mortality in the United States, with an estimated 100,000 deaths annually and uP to 30% of Patients dying within the first month of diagnosis. Recent guidelines now risk-stratify intermediate-risk PE Patients to intermediate-low and intermediate-high risk categories, but consensus on treatment for those Patients are controversial, as compared to that of high or low-risk Patients. Because of an increased risk of major, non-major, and intracranial bleeding and an uncertain effect on survival and Post-thrombotic complications, thrombolysis is not routinely recommended in the guidelines for intermediate- risk Patients. However, studies have evaluated half-dose (50 mg dose) tissue Plasminogen activator (tPA) and this aPPears to be effective for treating PE with a reduced yet still significant risk of bleeding. -

New Age of Anticoagulants
New Age of Anticoagulants DP Suresh MD FACC FSCAI Director, Heart and Vascular Group ST Elizabeth Physicians, KY Associate Professor of Medicine, University of Cincinnati. Low-Molecular-Weight Heparins Potential Advantages: • Lack of binding to plasma proteins and endothelium • Good bioavailability • Stable dose response • Long half-life • Resistance does not develop Direct Factor Xa inhibition Tissue XIIa factor XIa VIIa IXa ×Xa Factor II (prothrombin) Fibrinogen Fibrin clot Factor Xa inhibitors FXa may be a better target than thrombin – Has few functions outside coagulation (compared with thrombin) – Has a wider therapeutic window than thrombin (separation of efficacy and bleeding), in vitro – Thrombin inhibitors are associated with rebound thrombin generation – no evidence with FXa inhibitors – Efficacy of heparin-based anticoagulants improves as selectivity for FXa increases: UFH < LMWH < fondaparinux New anticoagulants ORAL PARENTERAL TF/VIIa TFPI (tifacogin) TTP889 X IX IXa APC (drotrecogin alfa) VIIIa sTM (ART-123) Rivaroxaban Apixaban Va AT Fondaparinux LY517717 Xa YM150 Idraparinux DU-176b PRT-054021 II DX-9065a Ximelagatran Otamixaban Dabigatran IIa Fibrinogen Fibrin Adapted from Weitz & Bates, J Thromb Haemost 2005 Oral Factor Xa inhibitors Clinical development Rivaroxaban (JNJ/Bayer) Phase IIb Phase III Apixaban (BMS) Phase III YM150 (Astellas) Phase IIb DU-176b (Daiichi) Phase IIb LY517717 (Lilly) Phase IIb 813893 (GSK) Phase I/II PRT054021(Portola) Phase II Stroke: A significant cause of poor health and Death • Stroke accounts for nearly 10% of all deaths worldwide • The number of strokes per year is predicted to rise dramatically as the population ages • About 20-30% strokes are cardio embolic and 15% relate to AF • Strokes in patients with AF are more severe and have worse outcomes than strokes in people without AF • AF almost doubles the death rate from stroke. -

The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’S Perspective
International Journal of Molecular Sciences Review The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’s Perspective Hau C. Kwaan 1,* and Paul F. Lindholm 2 1 Division of Hematology/Oncology, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA 2 Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; [email protected] * Correspondence: [email protected] Abstract: The novel coronavirus disease (COVID-19) has many characteristics common to those in two other coronavirus acute respiratory diseases, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). They are all highly contagious and have severe pulmonary complications. Clinically, patients with COVID-19 run a rapidly progressive course of an acute respiratory tract infection with fever, sore throat, cough, headache and fatigue, complicated by severe pneumonia often leading to acute respiratory distress syndrome (ARDS). The infection also involves other organs throughout the body. In all three viral illnesses, the fibrinolytic system plays an active role in each phase of the pathogenesis. During transmission, the renin-aldosterone- angiotensin-system (RAAS) is involved with the spike protein of SARS-CoV-2, attaching to its natural receptor angiotensin-converting enzyme 2 (ACE 2) in host cells. Both tissue plasminogen activator (tPA) and plasminogen activator inhibitor 1 (PAI-1) are closely linked to the RAAS. In lesions in the lung, kidney and other organs, the two plasminogen activators urokinase-type plasminogen activator (uPA) and tissue plasminogen activator (tPA), along with their inhibitor, plasminogen activator 1 (PAI-1), are involved. The altered fibrinolytic balance enables the development of a hypercoagulable Citation: Kwaan, H.C.; Lindholm, state. -

Doacs) and the Antidote Idarucizumab
Update overview 2019 of reports on direct oral anticoagulants (DOACs) and the antidote idarucizumab Introduction Lareb previously published yearly overviews of reports (most recently in 2018) in consultation with the Medicines Evaluation Board CBG-MEB, concerning the direct oral anticoagulants (DOACs) dabigatran Pradaxa®, registered in the Netherlands in 2008 [1], rivaroxaban Xarelto®, registered in 2008 [2], apixaban Eliquis®, registered in 2011 [3] and edoxaban (Lixiana®), registered in 2015 [4-9]. The current overview provides a new yearly update of the reports received by Lareb for these DOACs. Furthermore, reports received by Lareb for the antidote idarucizumab are described in this overview. Idarucizumab is a specific antidote for dabigatran and was registered in the Netherlands in 2015 [10]. For this overview, data from the national ADR database were used. These data include reports with serious outcome from the Lareb Intensive Monitoring System (LIM). The DOACs have been monitored with the LIM methodology since September 2012. Prescription data The number of patients using DOACs in the Netherlands according to the GIP database is shown in table 1 [11]. These data are based on extramurally provided medication included in the Dutch health insurance package. Because the antidote idarucizumab is administered in the hospital and not reimbursed directly via the healthcare insurance, these data are not available for this drug. The number of reports received by the Netherlands Pharmacovigilance Centre Lareb per year since 2013 for each DOAC, is also shown in table 1. Furthermore, table 1 shows the calculated number of these reports per 1.000 users according to the GIP database. As noted before, the data from the GIP database represent reimbursed medicines and these may differ from actually prescribed medicines. -

Edoxaban Switch Programme - Frequently Asked Questions
Edoxaban Switch Programme - Frequently Asked Questions What should I tell patients? NHS Tayside is reviewing all patients currently receiving a Direct Oral Anticoagulant (DOAC) for stroke prevention in NV-AF(non-valvular atrial fibrillation) Edoxaban has been identified as the first choice DOAC. It is similarly effective to the other DOAC options but costs considerably less Clinical experts in Tayside are supporting the use of edoxaban All newly diagnosed NV-AF patients will be started on edoxaban as 1st choice for those unsuitable for warfarin Existing patients already on a DOAC for NV-AF are to be reviewed and considered for switch to edoxaban This will help to ensure that the money available to spend on medicines is being used appropriately Is edoxaban as good as the other DOACs? Yes, the evidence is that it is as effective as warfarin and the other DOACs. It is licensed for this indication and has been recommended by the Scottish Medicines Consortium Other Scottish Health Boards are also considering the use of edoxaban A recent Health Improvement Scotland (HIS) summary (http://www.healthcareimprovementscotland.org/our_work/cardiovascular_dis ease/programme_resources/doac_review_report.aspx) is consistent with this Tayside switch recommendation Lead clinicians from cardiology, stroke, vascular medicine, relevant MCN’s and haematology are all supportive of this Tayside guidance on the basis of current evidence Will we need to do a further switch if the price of other DOACs falls? The rebate on edoxaban is in place for five -

Anatomisch-Therapeutisch-Chemische Klassifikation Mit Tagesdosen Für Den Deutschen Arzneimittelmarkt Gemäß § 73 Abs
Wissenschaftliches Institut der AOK GKV-Arzneimittelindex Anatomisch-therapeutisch-chemische Klassifikation mit Tagesdosen für den deutschen Arzneimittelmarkt gemäß § 73 Abs. 8 Satz 5 SGB V. 14. Sitzung der Arbeitsgruppe ATC/DDD des Kuratoriums für Fragen der Klassifikation im Gesundheitswesen am 27. November 2015, BMG in Berlin © WIdO 2015 GKV-Arzneimittelindex Agenda • Das anatomisch-therapeutisch-chemische Klassifikationssystem • Entwicklung der ATC/DDD Klassifikation • Workflow ATC/DDD 2016 • Beschlussvorlage • Stellungnahmen zu der Beschlussvorlage • Workflow ATC/DDD 2017 © WIdO 2015 14. Sitzung der Arbeitsgruppe ATC/DDD des KKG 2 GKV-Arzneimittelindex Agenda • Das anatomisch-therapeutisch-chemische Klassifikationssystem • Entwicklung der ATC/DDD Klassifikation • Workflow ATC/DDD 2016 • Beschlussvorlage • Stellungnahmen zu der Beschlussvorlage • Workflow ATC/DDD 2017 © WIdO 2015 14. Sitzung der Arbeitsgruppe ATC/DDD des KKG 3 GKV-Arzneimittelindex Das Anatomisch-therapeutisch-chemische Klassifikationssystem A Alimentäres System und Stoffwechsel B Blut und blutbildende Organe C Kardiovaskuläres System D Dermatika G Urogenitalsystem und Sexualhormone H Systemische Hormonpräparate, exkl. Sexualhormone u. Insuline J Antiinfektiva zur systemischen Anwendung L Antineoplastische und immunmodulierende Mittel M Muskel- und Skelettsystem N Nervensystem P Antiparasitäre Mittel, Insektizide und Repellenzien R Respirationstrakt S Sinnesorgane V Varia © WIdO 2015 14. Sitzung der Arbeitsgruppe ATC/DDD des KKG 4 GKV-Arzneimittelindex Das Anatomisch-therapeutisch-chemische -
EXAMPLE Alteplase Thrombolytic Central Changes Noted
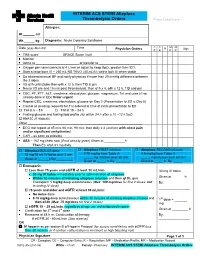
INTERIM ACS STEMI Alteplase Thrombolysis Orders Place Label Here Allergies: Ht. cm Wt. kg Diagnosis: Acute Coronary Syndrome C C M M Date (yyyy-Mon-dd) Time R Sign Physician Orders P E P R TIMI score ____________ GRACE Score (risk) ____________________ Monitor Admit to or transfer to _______________________ Oxygen per nasal cannula at 4 L/min or adjust to keep SpO2 greater than 92% Start a large bore IV – 250 mL NS TKVO (40 mL/h); saline lock IV when stable Do bilateral manual BP and notify physician if more than 20 mmHg difference between the 2 sides VS q1h until stable then q4h x 12 h, then TID & prn Neuro VS pre and 15 min post thrombolysis, then q1h x 4, q4h x 12 h, TID and prn CBC, PT, PTT, ALT, creatinine, electrolytes, glucose, magnesium, TnI and urea (if not already done in ED) Order urgent Repeat CBC, creatinine, electrolytes, glucose on Day 2 (Presentation to ED is Day 0) Cancel all pending requests for TnI ordered at time of initial presentation to ED TnI at 6 – 8 h TnI at 18 – 24 h Fasting glucose and fasting lipid profile (do within 24 h after a 10 –12 h fast) HbA1C (if diabetic) Other _______________________________________________________________ ECG stat repeat at 45 min, 60 min, 90 min: then daily x 3 (and prn with chest pain and/or significant arrhythmias) CXR – as soon as possible ASA – 162 mg chew now (if not already given) Given at h Then EC ASA 81 mg daily. Alteplase BOLUS dose Alteplase FIRST infusion Alteplase SECOND infusion 15 mg/15 mL IV bolus over 2 min 0.75 mg/kg from Table A 0.5 mg/kg from Table A _____ mg infusion over 30 min _____ mg infusion over 60 min Given at ______h By:_________ Given at _____ h By: ________ Given at _____ h By: _____ Enoxaparin Less than 75 years and eGFR at least 30 mL/min 30 mg IV bolus 30 mg IV bolus immediately prior to administration of alteplase Within 30 minutes of initiating alteplase infusion and then q12h, give Given at _______h Enoxaparin 1 mg/kg deep subcutaneous (Max. -

ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent
ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent ). Indications: - Management of acute myocardial infarction for the lysis of thrombi in coronary arteries; management of acute ischemic stroke -Acute myocardial infarction (AMI): Chest pain ≥20 minutes, ≤12-24 hours; S-T elevation ≥0.1 mV in at least two ECG leads -Acute pulmonary embolism (APE): Age ≤75 years: Documented massive pulmonary embolism by pulmonary angiography or echocardiography or high probability lung scan with clinical shock . -Restoration of central venous catheter function *Unlabeled/Investigational :Acute peripheral arterial occlusive disease. Dosage: -Coronary artery thrombi: Front loading dose (weight-based): -Patients >67 kg: Total dose: 100 mg over 1.5 hours; infuse 15 mg over 1-2 minutes. Infuse 50 mg over 30 minutes. Infuse remaining 35 mg of alteplase over the next hour. Maximum total dose: 100 mg -Patients ≤67 kg: Infuse 15 mg I.V. bolus over 1-2 minutes, then infuse 0.75 mg/kg (not to exceed 50 mg) over next 30 minutes, followed by 0.5 mg/kg over next 60 minutes (not to exceed 35 mg) Maximum total dose: 100 mg. See “Notes.” Note: Concurrently, begin heparin 60 units/kg bolus (maximum: 4000 units) followed by continuous infusion of 12 units/kg/hour (maximum: 1000 units/hour) and adjust to aPTT target of 1.5-2 times the upper limit of control. Note: Thrombolytic should be administered within 30 minutes of hospital arrival. Administer concurrent aspirin, clopidogrel, and anticoagulant therapy (ie, unfractionated heparin, enoxaparin, or fondaparinux) with alteplase (O’Gara, 2013). -Acute massive or submassive pulmonary embolism: I.V. (Activase®): 100 mg over 2 hours; may be administered as a 10 mg bolus followed by 90 mg over 2 hours as was done in patients with submassive PE (Konstantinides, 2002). -

Lixiana, INN-Edoxaban
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Lixiana 15 mg film-coated tablets Lixiana 30 mg film-coated tablets Lixiana 60 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Lixiana 15 mg film-coated tablets Each 15 mg film-coated tablet contains 15 mg edoxaban (as tosilate). Lixiana 30 mg film-coated tablets Each 30 mg film-coated tablet contains 30 mg edoxaban (as tosilate). Lixiana 60 mg film-coated tablets Each 60 mg film-coated tablet contains 60 mg edoxaban (as tosilate). For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet. Lixiana 15 mg film-coated tablets Orange, round-shaped film-coated tablets (6.7 mm diameter) debossed with “DSC L15”. Lixiana 30 mg film-coated tablets Pink, round-shaped film-coated tablets (8.5 mm diameter) debossed with “DSC L30”. Lixiana 60 mg film-coated tablets Yellow, round-shaped film-coated tablets (10.5 mm diameter) debossed with “DSC L60”. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Lixiana is indicated in prevention of stroke and systemic embolism in adult patients with nonvalvular atrial fibrillation (NVAF) with one or more risk factors, such as congestive heart failure, hypertension, age ≥ 75 years, diabetes mellitus, prior stroke or transient ischaemic attack (TIA). Lixiana is indicated in treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE), and for the prevention of recurrent DVT and PE in adults (see section 4.4 for haemodynamically unstable PE patients). 2 4.2 Posology and method of administration Posology Prevention of stroke and systemic embolism The recommended dose is 60 mg edoxaban once daily.