Alteplase: the Clot Buster
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Enoxaparin Sodium Solution for Injection, Manufacturer's Standard
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION PrLOVENOX® Enoxaparin sodium solution for injection 30 mg in 0.3 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 40 mg in 0.4 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 60 mg in 0.6 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 80 mg in 0.8 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 100 mg in 1 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 300 mg in 3 mL solution (100 mg/mL), multidose vials for subcutaneous or intravenous injection PrLOVENOX® HP Enoxaparin sodium (High Potency) solution for injection 120 mg in 0.8 mL solution (150 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 150 mg in 1 mL solution (150 mg/mL), pre-filled syringes for subcutaneous or intravenous injection Manufacturer’s standard Anticoagulant/Antithrombotic Agent ATC Code: B01AB05 Product Monograph – LOVENOX (enoxaparin) Page 1 of 113 sanofi-aventis Canada Inc. Date of Initial Approval: 2905 Place Louis-R.-Renaud February 9, 1993 Laval, Quebec H7V 0A3 Date of Revision September 7, 2021 Submission Control Number: 252514 s-a version 15.0 dated September 7, 2021 Product Monograph – LOVENOX (enoxaparin) Page 2 of 113 TABLE OF CONTENTS Sections or subsections that are not applicable at the time of authorization are not listed. TABLE OF CONTENTS .............................................................................................................. -

The Evolving Role of Direct Thrombin Inhibitors in Acute Coronary
View metadata, citation and similar papers at core.ac.uk brought to you by CORE Journal of the American College of Cardiology providedVol. by 41, Elsevier No. 4 - SupplPublisher S Connector © 2003 by the American College of Cardiology Foundation ISSN 0735-1097/03/$30.00 Published by Elsevier Science Inc. PII S0735-1097(02)02687-6 The Evolving Role of Direct Thrombin Inhibitors in Acute Coronary Syndromes John Eikelboom, MBBS, MSC, FRACP, FRCPA,* Harvey White, MB, CHB, DSC, FRACP, FACC,† Salim Yusuf, MBBS, DPHIL, FRCP (UK), FRCPC, FACC‡ Perth, Australia; Auckland, New Zealand; and Hamilton, Ontario, Canada The central role of thrombin in the initiation and propagation of intravascular thrombus provides a strong rationale for direct thrombin inhibitors in acute coronary syndromes (ACS). Direct thrombin inhibitors are theoretically likely to be more effective than indirect thrombin inhibitors, such as unfractionated heparin or low-molecular-weight heparin, because the heparins block only circulating thrombin, whereas direct thrombin inhibitors block both circulating and clot-bound thrombin. Several initial phase 3 trials did not demonstrate a convincing benefit of direct thrombin inhibitors over unfractionated heparin. However, the Direct Thrombin Inhibitor Trialists’ Collaboration meta-analysis confirms the superiority of direct thrombin inhibitors, particularly hirudin and bivalirudin, over unfractionated heparin for the prevention of death or myocardial infarction (MI) during treatment in patients with ACS, primarily due to a reduction in MI (odds ratio, 0.80; 95% confidence interval, 0.70 to 0.91) with little impact on death. The absolute risk reduction in the composite of death or MI at the end of treatment (0.8%) was similar at 30 days (0.7%), indicating no loss of benefit after cessation of therapy. -

Streptokinase) and Streptococcal Desoxyribonuclease on Fibrinous, Purulent, and Sanguinous Pleural Exudations
THE EFFECT IN PATIENTS OF STREPTOCOCCAL FIBRINOLYSIN (STREPTOKINASE) AND STREPTOCOCCAL DESOXYRIBONUCLEASE ON FIBRINOUS, PURULENT, AND SANGUINOUS PLEURAL EXUDATIONS William S. Tillett, Sol Sherry J Clin Invest. 1949;28(1):173-190. https://doi.org/10.1172/JCI102046. Research Article Find the latest version: https://jci.me/102046/pdf THE EFFECT IN PATIENTS OF STREPTOCOCCAL FIBRINOLYSIN (STREPTOKINASE) AND STREPTOCOCCAL DESOXYRIBO- NUCLEASE ON FIBRINOUS, PURULENT, AND SAN- GUINOUS PLEURAL EXUDATIONS' By WILLIAM S. TILLETT AND SOL SHERRY (From the Department of Medicine, New York University College of Medicine, and the Third Medical Division of Bellevue Hospital, New York City) (Received for publication August 6, 1948) The results described in this article were ob- coccal groups C and G (3). The product is tained by the injection of concentrated and par- abundantly excreted into the culture medium in tially purified preparations derived from broth which the organisms are grown and is readily ob- cultures of hemolytic streptococci into the pleural tainable free from the bacterial cells in sterile cavity of selected patients who were suffering filtrates. from different types of diseases that gave rise to The fibrinolytic action, in tests conducted un- pleural exudations. The possibility has been ex- der optimal laboratory conditions, is unusually plored of utilizing two of the defined properties rapid in action on the fibrin coagulum of normal elaborated by hemolytic streptococci that have the human blood, requiring only a few minutes when unique capacity of causing rapid lysis of the solid whole plasma is employed as a source of fibrin, elements (fibrin and nucleoprotein) that are sig- and an even shorter time when preparations of nificant parts of exudates. -

Streptokinase Available Forms Indications & Dosages Interactions
streptomycin sulfate 145 streptokinase streptomycin sulfate Kabikinase, Streptase Aminoglycoside; antibiotic Plasminogen activator; thrombolytic PRC: D enzyme PRC: C Available forms Injection: 400 mg/ml; Lyophilized cake/ Available forms powder for injection: 200 mg/ml Injection: 250,000, 750,000, 1,500,000 IU in vials for reconstitution Indications & dosages ➤ TB—Adult: 1 g or 15 mg/kg IM daily, Indications & dosages or 25-30 mg/kg (max 1.5 g) 2-3 times/wk ➤ Arteriovenous cannula occlusion— ϫ ≥ 1 yr. Elderly: Reduce daily dosage Adult: 250,000 IU in 2 ml IV solution in based on age, renal function, and 8th cra- each cannula limb over 25-35 min. Clamp nial nerve function. Suggested dosage cannula 2 hr. Aspirate, flush, and re- 10 mg/kg (max 750 mg) IM daily. Child: connect. 20-40 mg/kg (max 1 g) IM daily, or 25- ➤ Venous thrombosis, PE, arterial throm- 30 mg/kg (max 1.5 g) 2-3 times/wk ≥ bosis and embolism—Adult: 250,000 IU 1yr.† IV over 30 min. Then 100,000 IU/hr IV ϫ ➤ Enterococcal endocarditis—Adult: 1 g 72 hr for DVT and 100,000 IU/hr ϫ 24- IM q 12 hr ϫ 2 wk; then 500 mg IM q 72 hr for PE and arterial thrombosis or 12 hr ϫ 4 wk with a PCN.† embolism. ➤ Tularemia—Adult: 1-2 g IM daily in di- ➤ Lysis of coronary artery thrombi asso- vided doses ϫ 7-14 d or until patient ciated with MI—Adult: 20,000 IU IV bolus afebrile for 5-7 d.† via coronary catheter; then 2,000 IU/min ➤ Plague—Adult: 2 g (30 mg/kg) IM daily infusion over 60 min. -
EXAMPLE Alteplase Thrombolytic Central Changes Noted
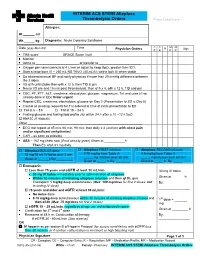
INTERIM ACS STEMI Alteplase Thrombolysis Orders Place Label Here Allergies: Ht. cm Wt. kg Diagnosis: Acute Coronary Syndrome C C M M Date (yyyy-Mon-dd) Time R Sign Physician Orders P E P R TIMI score ____________ GRACE Score (risk) ____________________ Monitor Admit to or transfer to _______________________ Oxygen per nasal cannula at 4 L/min or adjust to keep SpO2 greater than 92% Start a large bore IV – 250 mL NS TKVO (40 mL/h); saline lock IV when stable Do bilateral manual BP and notify physician if more than 20 mmHg difference between the 2 sides VS q1h until stable then q4h x 12 h, then TID & prn Neuro VS pre and 15 min post thrombolysis, then q1h x 4, q4h x 12 h, TID and prn CBC, PT, PTT, ALT, creatinine, electrolytes, glucose, magnesium, TnI and urea (if not already done in ED) Order urgent Repeat CBC, creatinine, electrolytes, glucose on Day 2 (Presentation to ED is Day 0) Cancel all pending requests for TnI ordered at time of initial presentation to ED TnI at 6 – 8 h TnI at 18 – 24 h Fasting glucose and fasting lipid profile (do within 24 h after a 10 –12 h fast) HbA1C (if diabetic) Other _______________________________________________________________ ECG stat repeat at 45 min, 60 min, 90 min: then daily x 3 (and prn with chest pain and/or significant arrhythmias) CXR – as soon as possible ASA – 162 mg chew now (if not already given) Given at h Then EC ASA 81 mg daily. Alteplase BOLUS dose Alteplase FIRST infusion Alteplase SECOND infusion 15 mg/15 mL IV bolus over 2 min 0.75 mg/kg from Table A 0.5 mg/kg from Table A _____ mg infusion over 30 min _____ mg infusion over 60 min Given at ______h By:_________ Given at _____ h By: ________ Given at _____ h By: _____ Enoxaparin Less than 75 years and eGFR at least 30 mL/min 30 mg IV bolus 30 mg IV bolus immediately prior to administration of alteplase Within 30 minutes of initiating alteplase infusion and then q12h, give Given at _______h Enoxaparin 1 mg/kg deep subcutaneous (Max. -

ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent
ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent ). Indications: - Management of acute myocardial infarction for the lysis of thrombi in coronary arteries; management of acute ischemic stroke -Acute myocardial infarction (AMI): Chest pain ≥20 minutes, ≤12-24 hours; S-T elevation ≥0.1 mV in at least two ECG leads -Acute pulmonary embolism (APE): Age ≤75 years: Documented massive pulmonary embolism by pulmonary angiography or echocardiography or high probability lung scan with clinical shock . -Restoration of central venous catheter function *Unlabeled/Investigational :Acute peripheral arterial occlusive disease. Dosage: -Coronary artery thrombi: Front loading dose (weight-based): -Patients >67 kg: Total dose: 100 mg over 1.5 hours; infuse 15 mg over 1-2 minutes. Infuse 50 mg over 30 minutes. Infuse remaining 35 mg of alteplase over the next hour. Maximum total dose: 100 mg -Patients ≤67 kg: Infuse 15 mg I.V. bolus over 1-2 minutes, then infuse 0.75 mg/kg (not to exceed 50 mg) over next 30 minutes, followed by 0.5 mg/kg over next 60 minutes (not to exceed 35 mg) Maximum total dose: 100 mg. See “Notes.” Note: Concurrently, begin heparin 60 units/kg bolus (maximum: 4000 units) followed by continuous infusion of 12 units/kg/hour (maximum: 1000 units/hour) and adjust to aPTT target of 1.5-2 times the upper limit of control. Note: Thrombolytic should be administered within 30 minutes of hospital arrival. Administer concurrent aspirin, clopidogrel, and anticoagulant therapy (ie, unfractionated heparin, enoxaparin, or fondaparinux) with alteplase (O’Gara, 2013). -Acute massive or submassive pulmonary embolism: I.V. (Activase®): 100 mg over 2 hours; may be administered as a 10 mg bolus followed by 90 mg over 2 hours as was done in patients with submassive PE (Konstantinides, 2002). -

ACTIVASE (Alteplase) for Injection, for Intravenous Use Initial U.S
Application 103172 This document contains: Label for ACTIVASE [Supplement 5203, Action Date 02/13/2015] Also available: Label for CATHFLO ACTIVASE [Supplement 5071, Action Date 01/04/2005] HIGHLIGHTS OF PRESCRIBING INFORMATION Acute Ischemic Stroke These highlights do not include all the information needed to use • Current intracranial hemorrhage. (4.1) ACTIVASE safely and effectively. See full prescribing information for • Subarachnoid hemorrhage. (4.1) ACTIVASE. Acute Myocardial Infarction or Pulmonary Embolism • History of recent stroke. (4.2) ACTIVASE (alteplase) for injection, for intravenous use Initial U.S. Approval: 1987 -----------------------WARNINGS AND PRECAUTIONS----------------------- • Increases the risk of bleeding. Avoid intramuscular injections. Monitor for ---------------------------INDICATIONS AND USAGE-------------------------- bleeding. If serious bleeding occurs, discontinue Activase. (5.1) Activase is a tissue plasminogen activator (tPA) indicated for the treatment of • Monitor patients during and for several hours after infusion for orolingual • Acute Ischemic Stroke (AIS). (1.1) angioedema. If angioedema develops, discontinue Activase. (5.2) • Acute Myocardial Infarction (AMI) to reduce mortality and incidence of • Cholesterol embolism has been reported rarely in patients treated with heart failure. (1.2) thrombolytic agents. (5.3) Limitation of Use in AMI: the risk of stroke may be greater than the benefit • Consider the risk of reembolization from the lysis of underlying deep in patients at low risk of death -

Nda 9-218/S-101
CENTER FOR DRUG EVALUATION AND RESEARCH Approval Package for: APPLICATION NUMBER: NDA 9-218/S-101 ® ® Name: Coumadin Tablets and Coumadin Injection Sponsor: Bristol-Myers Squibb Company Approval Date: September 2, 2005 CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: NDA 9-218/S-101 CONTENTS Reviews / Information Included in this Review Approval Letter X Approvable Letter Labeling X Division Director’s Memo Labeling Reviews X Medical Review Chemistry Review Environmental Assessment Pharmacology / Toxicology Review Statistical Review Microbiology Review Clinical Pharmacology & Biopharmaceutics Review Administrative and Correspondence Documents X CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: NDA 9-218/S-101 APPROVAL LETTER DEPARTMENT OF HEALTH & HUMAN SERVICES Public Health Service Food and Drug Administration Rockville, MD 20857 NDA 9-218/S-101 Bristol-Myers Squibb Company Attention: David L. Silberstein Associate Director New Opportunities and Product Development Global Regulatory Strategy P.O. Box 4000 Princeton, NJ 08543-4000 Dear Mr. Silberstein: Please refer to your supplemental new drug application dated April 6, 2005, received April 7, 2005, submitted under section 505(b) of the Federal Food, Drug, and Cosmetic Act for COUMADIN® Tablets (Warfarin Sodium Tablets, USP) Crystalline and COUMADIN® for Injection (Warfarin Sodium for Injection, USP). This “Changes Being Effected” supplemental new drug application provides for revisions to the Coumadin package insert to include information relating to drug interactions with Proton Pump Inhibitors (PPIs) and language cautioning against the ingestion of cranberry products, which have been reported to affect the response of patients to Coumadin. We completed our review of this application. This application is approved, effective on the date of this letter, for use as recommended in the agreed-upon labeling text with the correction listed below. -
Protocol-IV-Alteplase.Pdf
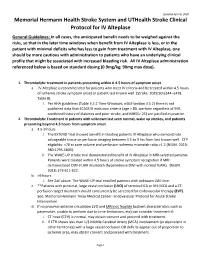
Updated April 6, 2020 Memorial Hermann Health Stroke System and UTHealth Stroke Clinical Protocol for IV Alteplase General Guidelines: In all cases, the anticipated benefit needs to be weighed against the risks, so that in the later time windows when benefit from IV Alteplase is less, or in the patient with minimal deficits who has less to gain from treatment with IV Alteplase, one should be more cautious with administration to patients who have an underlying clinical profile that might be associated with increased bleeding risk. All IV Alteplase administration referenced below is based on standard dosing (0.9mg/kg; 90mg max dose). 1. Thrombolytic treatment in patients presenting within 0-4.5 hours of symptom onset. a. IV Alteplase is recommended for patients who meet IV criteria and be treated within 4.5 hours of ischemic stroke symptom onset or patient last known well. (Stroke. 2019;50:e344–e418. Table 8). i. Per AHA guidelines (Table 3.5.2 Time Windows; e363-Section 3.5.2) there is not published data that ECASS III exclusion criteria (age > 80, warfarin regardless of INR, combined history of diabetes and prior stroke, and NIHSS> 25) are justified in practice. 2. Thrombolytic Treatment in patients with unknown last seen normal, wake up strokes, and patients presenting beyond 4.5 hours from symptom onset. a. 4.5-9 hours i. The EXTEND Trial showed benefit in treating patients IV Alteplase who demonstrate salvageable tissue on perfusion imaging between 4.5 to 9 hrs from last known well. CTP eligibility: <70 cc core volume and perfusion-ischemia mismatch ratio >1.2 (NEJM. -
1D1d1d0d0d0d1d0d0 Heparin Sodium Injection 5000 I.U./Ml
318476.0212:Layout 1 23.02.2012 13:33 Uhr Seite 1 126/318476/0212 Directions for Use B. Braun Melsungen AG · 34209 Melsungen, Germany Heparin Sodium Injection 5000 I.U./ml 1d1d1d0d0d0d1d0d0 Composition Weakening of the heparin effect 1 ml of solution for injection contains The heparin effect may be weakened by Heparin Sodium (porcine mucosa) 5,000 I.U. • doxorubicin according to WHO standard • intravenous glyceryl trinitrate (nitro-glycerine) 1 vial (5 ml) of solution for injection contains After discontinuation of glyceryl trinitrate the aPTT may rise suddenly. If Heparin Sodium 25,000 I.U. heparin is administered during nitro-glycerine infusion, close monitoring of the aPTT and adjustment of the heparin dose are necessary. Excipients: Benzyl alcohol (antimicrobial preservative; 10 mg/ml), sodium chloride, Inhibition of the heparin effect water for injections The effect of heparin may be inhibited by: • Ascorbic acid, Pharmaceutical form • antihistamines, Solution for injection • digitalis (cardiac glycosides), Clear, colourless or faintly straw-coloured aqueous solution • tetracyclins, Pharmaco-therapeutic group Influence of heparin on the effect of other drug substances: Anti-thrombotic agents, heparin group, ATC code B01A B01. • Other drug substances being bound to plasma proteins (e.g. propranolol): Indications Heparin may displace these from protein binding, leading to an enhance- • Prophylaxis of thrombo-embolism; ment of their effect. • Use as anticoagulant in the therapy of acute venous and arterial throm- • Drugs that lead to an increase of the serum potassium level: bo-embolism (including early treatment of myocardial infarction and should only be administered together with heparin under careful monitor- unstable angina pectoris); ing. -

The Treatment and Prevention Ofacute Ischemic Stroke
EDITORIAL Alvaro Nagib Atallah* The treatment and prevention of acute ischemic stroke rotecting the brain from the consequences .of alternated with placebo (lower dose) and placebo injections vascular obstruction is obviously very important. every 12 hours, for 10 days. The evaluation at 6 months PHowever, how to manage this is a very complex showed that the treated group had a lower incidence rate task. Three recent studies have provided evidence that of poor outcomes, death or dependency in daily activities, I 3 should not be ignored or misinterpreted by physicians. - 45 vs. 65%. In other words, it was necessary to treat 5 The National Institute of Neurological Disorders and patients to benefit one. Evaluations at 10 days did not show Stroke rt-PA Stroke Study Groupl shows the results of a differences in death rates or haemorrhage transformation randomized, collaborative placebo-controlled trial. Six of the cerebral infarction. hundred and twenty-four patients were studied. The The Multicentre Acute Stroke Trial-Italy (MAST-I) treatment was started before 90' of the start of the stroke Group compared the effectiveness of streptokinase, aspirin or before 180'. Patients received recombinant rt-PA and a combination of both for the treatment of ischemic (alteplase) 0.9 mg/kg or placebo. A careful neurological stroke. Six hundred and twenty-two patients were evaluation was done at 24 hours and 3 months after the randomized to receive I hour infusions of 1.5 mD of stroke. streptokinase alone, the same dose of streptokinase plus There were no significant differences between the 300 mg of buffered aspirin, or 300 mg of aspirin alone for groups at 24 hours after the stroke. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole