Does Migration Destination Affect the Mortality Advantage of Mexican Immigrants? a Comparison of Traditional, New, and Emerging Destinations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
System/370 Model 145 Reference Summary
System/370 Model 145 Reference Summary S229-2239-1 IBM Corporation, Field Support Documentation, Dept 927, Rochester, Minnesota 55901 PREFACE This publication is primarily intended for customer engineers servicing System/370 Model 145. Second Edition (September 1972) This is a major revision of, and makes 8229-2239-0 obsolete. Address any comments concerning the contents of this publication to: IBM, Field Support Documentation, Dept 927, Rochester, Minnesota 55901 © International Business Machines Corporation 1972 CONTENTS Section 1 - Control Words Branch and Module Switch Word "O" . 1. 1 Branch Word . 1.2 GA Function Charts . 1.3 GA Function Charts . 1.4 GA Function Charts . 1.5 Branch and Link or Return Word . 1.6 Word Move Word Version"O" . 1. 7 Word Move Word Version "1" . 1.8 Storage Word, Non K-Addressable . 1.9 Storage Word, K-Addressable . 1.10 Arithmetic Word 10 Byte Version 1.11 Arithmetic Word, Fullword Version 1.12 Arithmetic Word, 11 Direct ByteVersion . 1.13 Arithmetic Word, 10/11 Indirect Byte Version . 1.14 ALU Entry Gating 1.15 Stat Set Symbols . 1.15 BranchSymbols . 1.15 Arithmetic Word Chart Selection 1.16 Address Formation Chart 1.16 Control Word Chart Selection 1.16 Section 2 - CPU 3145 CPU Data Flow . 2.1 I-Cycles Data Flow . 2.2 I-Cycles . 2.3 PSW Locations . 2.3 Expanded Local Storage . 2.3 I-Cycles . 2.3 I-Cycles Control Line Generation . 2.4 Control Word . 2.4 Control Register Decode . 2.4 iii ECCL Board Layout ............ 2.5 Data Bit Location Chart .......... 2.5 Common Test Points ........... -

Template Jurnal JAIC;
Journal of Applied Informatics and Computing (JAIC) Vol.2, No.1, Juli 2018, pp. 7~10 e-ISSN: 2548-6861 7 Simulation Strategic Positioning for Mobile Robot Roccer Wheels Mochamad Mobed Bachtiar1, Iwan Kurnianto Wibowo2, Rakhmat Faizal Ajie3 Teknik Komputer, Politeknik Elektronika Negeri Surabaya [email protected] 1, [email protected] 2, [email protected] 3 Article Info ABSTRACT Article history: Soccer robot is a combination of sports, robotics technology and multi agent system. The achieve goals in playing the ball, requires individual intelligence, and the ability Received 2018-04-30 of cooperation for individual skills. The success of a soccer robot team is influenced Revised 2018-06-01 by the success of the robot player to enter the ball into the opponent's goal. In Accepted 2018-07-01 entering the ball into the opponent's goal needed an appropriate position and strategic. This research makes the design in finding a strategic position at the time Keyword: of attack. The design divides the field into several small areas or the main grid, strategic position; attack where each region gives different action. The position is said to be strategic if the strategy; empty space; naïve robot passing success and has a fairly wide perspective against the goal. The bayes classifier strategic position is gained from the greatest opportunity of some of the decisive conditions. The calculation used is to use the Probability Naïve Bayes Classifier by taking the maximum value that serve as a strategic position. So this research resulted in a design in finding strategic position. Copyright © 2017 Journal of Applied Informatics and Computing. -

The New Tourism Lexicon: Rewriting Our Industry's Narrative
POLICY BRIEF THE NEW TOURISM LEXICON: REWRITING OUR INDUSTRY'S NARRATIVE Last year, Destinations International released a policy "Washington is the problem. Remind voters again and brief entitled, “Advocacy in the Face of Ideology,” which again about Washington spending, Washington waste, made the case that relying on ROI numbers to defend Washington taxation, Washington bureaucracy, the value and relevancy of a destination organization Washington rules and Washington regulations." was no longer a viable advocacy strategy. Instead, we Luntz also suggested replacing "drilling for oil" with argued, destination organizations need to support the "exploring for energy," "undocumented workers" with message of ROI in terms of dollars and cents with an "illegal aliens," and "estate tax" with "death tax." The ideological and value-based appeal to convince political substitutions often work — an Ipsos/NPR poll found that leaders that without a destination organization, these support for abolishing the estate tax jumps to 76% from returns will inevitably vanish. 65% when you call it the death tax. Our industry has unfortunately fallen for what George Lakoff, a professor of Cognitive Science and Linguistics at the University of California at Berkeley, dubs the “Enlightenment Fallacy.” According to this viewpoint, you simply need to tell people the facts in clear language and they’ll reason to the right, true conclusions. The problem, as Lakoff puts it is, “The cognitive and brain sciences have shown this is false… it’s false in every single detail.” The reality is that people tend to frame political arguments, and the facts behind them, in terms of their own values. -
Report on the Most Appropriate Indicators Related to the Basic Concepts
D 4.1 – Report on the most appropriate indicators related to the basic concepts Report on the most appropriate indicators related to the basic concepts Deliverable D4.1 This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 870708 D 4.1 – Report on the most appropriate indicators related to the basic concepts Disclaimer: The contents of this deliverable are the sole responsibility of one or more Parties of the SmartCulTour consortium and can under no circumstances be regarded as reflecting the position of the Research Executive Agency and European Commission under the European Union’s Horizon 2020 programme. Copyright and Reprint Permissions “You may freely reproduce all or part of this paper for non-commercial purposes, provided that the following conditions are fulfilled: (i) to cite the authors, as the copyright owners (ii) to cite the SmartCulTour Project and mention that the EC co-finances it, by means of including this statement “Smart Cultural Tourism as a Driver of Sustainable Development of European Regions - SmartCulTour Project no. H2020-870708 co financed by EC H2020 program” and (iii) not to alter the information.” _______________________________________________________________________________________ How to quote this document: Petrić, L., Mandić, A., Pivčević, S., Škrabić Perić, B., Hell, M., Šimundić, B., Muštra, V., Mikulić, D., & Grgić, J. (2020). Report on the most appropriate indicators related to the basic concepts. Deliverable 4.1 of the Horizon 2020 project SmartCulTour (GA number 870708), published on the project web site on September 2020: http://www.smartcultour.eu/deliverables/ D 4.1 – Report on the most appropriate indicators related to the basic concepts This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No. -

Nv9602 Nv9000 Control Panel
NV9602 NV9000 CONTROL PANEL User’s Guide VERSION 1.2 UG0040-02 2015-07-02 www.grassvalley.com Notices Copyright and Trademark Notice Copyright © 2015, Grass Valley USA, LLC. All rights reserved. Belden, Belden Sending All The Right Signals, and the Belden logo are trademarks or registered trademarks of Belden Inc. or its affiliated companies in the United States and other jurisdictions. Grass Valley USA, LLC, Miranda, NV9602, Kaleido, NVISION, iControl, and Densité are trademarks or registered trademarks of Grass Valley USA, LLC. Belden Inc., Grass Valley USA, LLC, and other parties may also have trademark rights in other terms used herein. Terms and Conditions Please read the following terms and conditions carefully. By using NVISION control panel documentation, you agree to the following terms and conditions. Grass Valley hereby grants permission and license to owners of NVISION control panels to use their product manuals for their own internal business use. Manuals for Grass Valley products may not be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying and recording, for any purpose unless specifically authorized in writing by Grass Valley. A Grass Valley manual may have been revised to reflect changes made to the product during its manufacturing life. Thus, different versions of a manual may exist for any given product. Care should be taken to ensure that one obtains the proper manual version for a specific product serial number. Information in this document is subject to change without notice and does not represent a commitment on the part of Grass Valley. Warranty information is available in the Support section of the Grass Valley Web site (www.grassvalley.com). -
Decnet-Plusftam and Virtual Terminal Use and Management
VSI OpenVMS DECnet-Plus FTAM and Virtual Terminal Use and Management Document Number: DO-FTAMMG-01A Publication Date: June 2020 Revision Update Information: This is a new manual. Operating System and Version: VSI OpenVMS Integrity Version 8.4-2 VSI OpenVMS Alpha Version 8.4-2L1 VMS Software, Inc., (VSI) Bolton, Massachusetts, USA DECnet-PlusFTAM and Virtual Terminal Use and Management Copyright © 2020 VMS Software, Inc. (VSI), Bolton, Massachusetts, USA Legal Notice Confidential computer software. Valid license from VSI required for possession, use or copying. Consistent with FAR 12.211 and 12.212, Commercial Computer Software, Computer Software Documentation, and Technical Data for Commercial Items are licensed to the U.S. Government under vendor's standard commercial license. The information contained herein is subject to change without notice. The only warranties for VSI products and services are set forth in the express warranty statements accompanying such products and services. Nothing herein should be construed as constituting an additional warranty. VSI shall not be liable for technical or editorial errors or omissions contained herein. HPE, HPE Integrity, HPE Alpha, and HPE Proliant are trademarks or registered trademarks of Hewlett Packard Enterprise. Intel, Itanium and IA-64 are trademarks or registered trademarks of Intel Corporation or its subsidiaries in the United States and other countries. UNIX is a registered trademark of The Open Group. The VSI OpenVMS documentation set is available on DVD. ii DECnet-PlusFTAM and Virtual -

VSI X.25 for Openvms Configuration Guide
VSI OpenVMS VSI X.25 for OpenVMS Configuration Guide Document Number: DO-DX25CG-01A Publication Date: August 2018 Revision Update Information: This is a new manual. Operating System and Version: VSI OpenVMS Integrity Version 8.4-2 VSI OpenVMS Alpha Version 8.4-2L1 Software Version: VSI X.25 for OpenVMS Version 2.1 VMS Software, Inc. (VSI) Burlington, Massachusetts, USA VSI X.25 for OpenVMS Configuration Guide Copyright © 2018 VMS Software, Inc. (VSI), Burlington, Massachusetts, USA Legal Notice Confidential computer software. Valid license from VSI required for possession, use or copying. Consistent with FAR 12.211 and 12.212, Commercial Computer Software, Computer Software Documentation, and Technical Data for Commercial Items are licensed to the U.S. Government under vendor's standard commercial license. The information contained herein is subject to change without notice. The only warranties for VSI products and services are set forth in the express warranty statements accompanying such products and services. Nothing herein should be construed as constituting an additional warranty. VSI shall not be liable for technical or editorial errors or omissions contained herein. HPE, HPE Integrity, HPE Alpha, and HPE Proliant are trademarks or registered trademarks of Hewlett Packard Enterprise. Intel and Itanium are trademarks or registered trademarks of Intel Corporation or its subsidiaries in the United States and other countries. Oracle is a registered trademark of Oracle and/or its affiliates. The VSI OpenVMS documentation set is available -

Towards Coordinated, Network-Wide Traffic
Towards Coordinated, Network-Wide Traffic Monitoring for Early Detection of DDoS Flooding Attacks by Saman Taghavi Zargar B.Sc., Computer Engineering (Software Engineering), Azad University of Mashhad, 2004 M.Sc., Computer Engineering (Software Engineering), Ferdowsi University of Mashhad, 2007 Submitted to the Graduate Faculty of the School of Information Sciences in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2014 UNIVERSITY OF PITTSBURGH SCHOOL OF INFORMATION SCIENCES This dissertation was presented by Saman Taghavi Zargar It was defended on June 3, 2014 and approved by James Joshi, Ph.D., Associate Professor, School of Information Sciences David Tipper, Ph.D., Associate Professor, School of Information Sciences Prashant Krishnamurthy, Ph.D., Associate Professor, School of Information Sciences Konstantinos Pelechrinis, Ph.D., Assistant Professor, School of Information Sciences Yi Qian, Ph.D., Associate Professor, College of Engineering, Dissertation Advisors: James Joshi, Ph.D., Associate Professor, School of Information Sciences, David Tipper, Ph.D., Associate Professor, School of Information Sciences ii Copyright c by Saman Taghavi Zargar 2014 iii Towards Coordinated, Network-Wide Traffic Monitoring for Early Detection of DDoS Flooding Attacks Saman Taghavi Zargar, PhD University of Pittsburgh, 2014 DDoS flooding attacks are one of the biggest concerns for security professionals and they are typically explicit attempts to disrupt legitimate users' access to services. Developing a com- prehensive defense mechanism against such attacks requires a comprehensive understanding of the problem and the techniques that have been used thus far in preventing, detecting, and responding to various such attacks. In this thesis, we dig into the problem of DDoS flooding attacks from four directions: (1) We study the origin of these attacks, their variations, and various existing defense mecha- nisms against them. -

A Logical Approach to Representing and Reasoning About Interdomain Routing Policies
A Logical Approach to Representing and Reasoning About Interdomain Routing Policies Anduo Wang and Zhijia Chen Temple University Abstract. The Internet paths connecting independently operated networks, also called domains or autonomous systems (ASes), are driven by semantically rich policies: the interdomain routing protocol that computes the Internet paths allows the ASes to influence path selection with their local policies, such as economic concerns or operational constraints. An AS can promote a policy compliant but globally longer path by carefully tweaking lower level path attributes that are used in the routing protocol. Such operational policies are notoriously complex and hard to understand. This paper takes a step back and asks whether a more principled logical approach can lead to AS policies that are easier to under- stand, reuse, evolve, and coexist. To this end, we propose to represent policies by database integrity constraints, in the form of headless datalog rules about what are the acceptable Internet paths. The simple datalog expression unifies a wide spectrum of AS policies, ranging from classic examples seen in today’s routing practice to futuristic ones proposed in various extensions to Internet routing. More importantly, by leveraging datalog’s connection to the theorem proving technique called the residue method, we developed a new technique for understanding the interactions among the policies — whether a policy can inadvertly affect another, and how to resolve the conflict. We also evaluated our logical policies, show- ing promising result with small overhead for conflict resolution on realistic large networks. 1 Introduction The Internet today is more than connecting remote hosts with valid paths. -
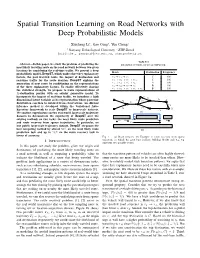
Spatial Transition Learning on Road Networks with Deep Probabilistic Models
Spatial Transition Learning on Road Networks with Deep Probabilistic Models Xiucheng Liy, Gao Congy, Yun Chengz y Nanyang Technological Univeristy, z ETH Zurich fxli055@e., [email protected], [email protected] TABLE I Abstract—In this paper, we study the problem of predicting the EXAMPLE OF TRIPS ON ROAD NETWORK. most likely traveling route on the road network between two given locations by considering the real-time traffic. We present a deep Route Destination Frequency probabilistic model–DeepST–which unifies three key explanatory factors, the past traveled route, the impact of destination and r3 ! r2 ! r4 C 400 real-time traffic for the route decision. DeepST explains the r3 ! r2 ! r5 ! r10 C 100 generation of next route by conditioning on the representations r1 ! r2 ! r5 ! r6 A 100 of the three explanatory factors. To enable effectively sharing r1 ! r2 ! r7 ! r8 B 100 r ! r ! r ! r ! r B 100 the statistical strength, we propose to learn representations of 1 2 5 6 9 K-destination proxies with an adjoint generative model. To incorporate the impact of real-time traffic, we introduce a high C r<latexit sha1_base64="(null)">(null)</latexit> 10 r<latexit sha1_base64="(null)">(null)</latexit> dimensional latent variable as its representation whose posterior r<latexit sha1_base64="(null)">(null)</latexit> 4 6 A r<latexit sha1_base64="lQIphb3ZxX5RFxPPJ2+0wE0HOKM=">AAAB6nicbZBNS8NAEIYn9avWr6hHL4tF8FQSEfRY9OKxov2ANpTNdtMu3WzC7kQooT/BiwdFvPqLvPlv3LY5aOsLCw/vzLAzb5hKYdDzvp3S2vrG5lZ5u7Kzu7d/4B4etUySacabLJGJ7oTUcCkUb6JAyTup5jQOJW+H49tZvf3EtRGJesRJyoOYDpWIBKNorQfd9/tu1at5c5FV8AuoQqFG3/3qDRKWxVwhk9SYru+lGORUo2CSTyu9zPCUsjEd8q5FRWNugny+6pScWWdAokTbp5DM3d8TOY2NmcSh7YwpjsxybWb+V+tmGF0HuVBphlyxxUdRJgkmZHY3GQjNGcqJBcq0sLsSNqKaMrTpVGwI/vLJq9C6qPmW7y+r9ZsijjKcwCmcgw9XUIc7aEATGAzhGV7hzZHOi/PufCxaS04xcwx/5Hz+AAKOjZo=</latexit> -

Strategic Communication in Tourism
STRATEGIC COMMUNICATION IN TOURISM DEPARTMENT OF DESIGN AND COMMUNICATION CENTRE FOR TOURISM, INNOVATION AND CULTURE (TIC) Bodil Stilling Blichfeldt Strategic Communication in Tourism Background, conceptualizations, introduction to analysis and relations to sustainable tourism and tourism innovation TIC TALKS no. 5, September 2017 1 Author info Associate Professor, Ph.D. Bodil Stilling Blichfeldt, TIC and Department of Design and Communication, University of Southern Denmark. Email: [email protected] Place of publication TIC is University of Southern Denmark’s multidisciplinary research center in tourism, innovation and culture. The center is located at the Kolding campus. TIC strives to transform the university to an engaged, collaborative institution where academics and students pursue an unrelenting examination of knowledge, its sources and its uses. TIC defines the university as a center for higher order knowledge creation and for collaboration with, and for, society at large. We do this through research-based education, education-based research and collaborative engagement with society. We aim to charter new territory in international academe, as well as in multi-level collaboration based on interdisciplinary research with a strong foundation in the Humanities. TIC engages in research dialogues through both a traditional peer-review publication strategy and through involvement in securing free access to knowledge. Supplementing traditional journal articles, TIC TALKS is one of TIC’s contributions to open access sharing and collaborative development of knowledge. TIC TALKS are provided by Centre for Tourism, Innovation and Culture, University of Southern Denmark Universitetsparken 1, Kolding, DK-6000 http://www.sdu.dk/en/Om_SDU/Institutter_centre/C_Tik.aspx The present manuscript qualifies as unfinished work-in-progress and the reader should bear in mind that the manuscript is quite likely to contain a series of errors, flaws and weaknesses. -

Catalogue a ‐ Z
Catalogue A ‐ Z A ? MARK AND MYSTERIANS "Same" LP CAMEO 1966 € 60 (US Garage‐Original Canada Pressing VG++++/VG+) 007 & SCENE " Landscapes" LP Detour € 12 (UK mod‐beat ' 70/ ' 80) 1‐2‐5 “Same” LP Misty lane € 13 (Garage punk dall’Olanda) 13th FLOOR ELEVATORS "Easter every Where" CD Spalax € 15,00 ('60 US Psych) 13th FLOOR ELEVATORS "Graeckle Debacle" CD Spalax € 15,00 ('60 US Psych) 13th FLOOR ELEVATORS "The Psychedelic Sound Of…" CD Spalax € 15,00 ('60 US Psych) 13th FLOOR ELEVATORS "Unlock the Secret" CD Spalx € 15,00 ('66 US Psych) 20/20 "Giving It All" 7" LINE 1979 € 15 (US Power Pop) 27 DEVILS JOKING "The Sucking Effect" LP RAVE 1991 € 10 (US Garage VG/M‐) 3 NORMAL BEATLES "We Name Is Justice" DLP BUBACK € 23 (Beat from Germany) 39 CLOCKS "Cold Steel To The Heart " LP WHAT'S SO FUNNY ABOUT 1985 € 35 (Psychedelic Wave from Germany) 39 CLOCKS "Subnarcotic" LP WHAT'S SO FUNNY ABOUT 1982 € 35 (Psychedelic Wave from Germany 1988 Reissue) 39 CLOCKS "The Original Psycho Beat" LP WHAT'S SO FUNNY ABOUT 1993 € 20 (Psychedelic Wave from Germany) 3D INVISIBLES "Robot Monster" 7" NEUROTIC BOP 1994 € 5 (US Punk Rock) 3D INVISIBLES "They Won't StayDead" LP NEUROTIC BOP 1989 € 15 (US Punk Rock) 440’S “Gas Grass Or As” 7” Rockin’ Bones € 5 (US Punk) 5 LES “Littering..” 7” HAGCLAND 198? € 5 (Power Pop dal Belgio M‐/M‐) 5.6.7.8.'S "Can't Help It !" CD AUGOGO € 14 (Japan Garage i 7"M‐/M) 5.6.7.8's "Sho‐Jo‐Ji" 7" THIRD MAN € 9 (Garage Punk from Tokyo) 60 FT DOLLS "Afterglow" 7" DOLENT € 3 (Promo Only) 64 SPIDERS "Potty Swat" 7" REGAL SELECT 1989 € 17 (US Punk M‐/M‐) 68 COMEBACK "Do The Rub" 7" BAG OF HAMMERS 1994 € 7 (US Punk Blues) 68 COMEBACK "Flip,Flop,& Fly" 7" GET HIP 1994 € 13 (US Punk Blues) 68 COMEBACK "Great Million Sellers" 7" 1+2 1994 € 8 (US Punk Blues) 68 COMEBACK "High Scool Confidential" 7" PCP I.