The Effects of Α-Gpc Supplementation On
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Role of Citicoline in the Management of Traumatic Brain Injury
pharmaceuticals Review Role of Citicoline in the Management of Traumatic Brain Injury Julio J. Secades Medical Department, Ferrer, 08029 Barcelona, Spain; [email protected] Abstract: Head injury is among the most devastating types of injury, specifically called Traumatic Brain Injury (TBI). There is a need to diminish the morbidity related with TBI and to improve the outcome of patients suffering TBI. Among the improvements in the treatment of TBI, neuroprotection is one of the upcoming improvements. Citicoline has been used in the management of brain ischemia related disorders, such as TBI. Citicoline has biochemical, pharmacological, and pharmacokinetic characteristics that make it a potentially useful neuroprotective drug for the management of TBI. A short review of these characteristics is included in this paper. Moreover, a narrative review of almost all the published or communicated studies performed with this drug in the management of patients with head injury is included. Based on the results obtained in these clinical studies, it is possible to conclude that citicoline is able to accelerate the recovery of consciousness and to improve the outcome of this kind of patient, with an excellent safety profile. Thus, citicoline could have a potential role in the management of TBI. Keywords: CDP-choline; citicoline; pharmacological neuroprotection; brain ischemia; traumatic brain injury; head injury Citation: Secades, J.J. Role of 1. Introduction Citicoline in the Management of Traumatic brain injury (TBI) is among the most devastating types of injury and can Traumatic Brain Injury. result in a different profile of neurological and cognitive deficits, and even death in the most Pharmaceuticals 2021, 14, 410. -

Endogenous Metabolites: JHU NIMH Center Page 1
S. No. Amino Acids (AA) 24 L-Homocysteic acid 1 Glutaric acid 25 L-Kynurenine 2 Glycine 26 N-Acetyl-Aspartic acid 3 L-arginine 27 N-Acetyl-L-alanine 4 L-Aspartic acid 28 N-Acetyl-L-phenylalanine 5 L-Glutamine 29 N-Acetylneuraminic acid 6 L-Histidine 30 N-Methyl-L-lysine 7 L-Isoleucine 31 N-Methyl-L-proline 8 L-Leucine 32 NN-Dimethyl Arginine 9 L-Lysine 33 Norepinephrine 10 L-Methionine 34 Phenylacetyl-L-glutamine 11 L-Phenylalanine 35 Pyroglutamic acid 12 L-Proline 36 Sarcosine 13 L-Serine 37 Serotonin 14 L-Tryptophan 38 Stachydrine 15 L-Tyrosine 39 Taurine 40 Urea S. No. AA Metabolites and Conjugates 1 1-Methyl-L-histidine S. No. Carnitine conjugates 2 2-Methyl-N-(4-Methylphenyl)alanine 1 Acetyl-L-carnitine 3 3-Methylindole 2 Butyrylcarnitine 4 3-Methyl-L-histidine 3 Decanoyl-L-carnitine 5 4-Aminohippuric acid 4 Isovalerylcarnitine 6 5-Hydroxylysine 5 Lauroyl-L-carnitine 7 5-Hydroxymethyluracil 6 L-Glutarylcarnitine 8 Alpha-Aspartyl-lysine 7 Linoleoylcarnitine 9 Argininosuccinic acid 8 L-Propionylcarnitine 10 Betaine 9 Myristoyl-L-carnitine 11 Betonicine 10 Octanoylcarnitine 12 Carnitine 11 Oleoyl-L-carnitine 13 Creatine 12 Palmitoyl-L-carnitine 14 Creatinine 13 Stearoyl-L-carnitine 15 Dimethylglycine 16 Dopamine S. No. Krebs Cycle 17 Epinephrine 1 Aconitate 18 Hippuric acid 2 Citrate 19 Homo-L-arginine 3 Ketoglutarate 20 Hydroxykynurenine 4 Malate 21 Indolelactic acid 5 Oxalo acetate 22 L-Alloisoleucine 6 Succinate 23 L-Citrulline 24 L-Cysteine-glutathione disulfide Semi-quantitative analysis of endogenous metabolites: JHU NIMH Center Page 1 25 L-Glutathione, reduced Table 1: Semi-quantitative analysis of endogenous molecules and their derivatives by Liquid Chromatography- Mass Spectrometry (LC-TripleTOF “or” LC-QTRAP). -

Clinical Significance of Small Molecule Metabolites in the Blood of Patients
www.nature.com/scientificreports OPEN Clinical signifcance of small molecule metabolites in the blood of patients with diferent types of liver injury Hui Li1,2,5, Yan Wang1,5, Shizhao Ma1,3, Chaoqun Zhang1,4, Hua Liu2 & Dianxing Sun1,4* To understand the characteristic of changes of serum metabolites between healthy people and patients with hepatitis B virus (HBV) infection at diferent stages of disease, and to provide reference metabolomics information for clinical diagnosis of liver disease patients. 255 patients with diferent stages of HBV infection were selected. 3 mL blood was collected from each patient in the morning to detect diferences in serum lysophosphatidylcholine, acetyl-l-carnitine, oleic acid amide, and glycocholic acid concentrations by UFLC-IT-TOF/MS. The diagnostic values of four metabolic substances were evaluated by receiver operating characteristic (ROC) curve. The results showed that the optimal cut-of value of oleic acid amide concentration of the liver cirrhosis and HCC groups was 23.6 mg/L, with a diagnostic sensitivity of 88.9% and specifcity of 70.6%. The diagnostic efcacies of the three substances were similar in the hepatitis and HCC groups, with an optimal cut-of value of 2.04 mg/L, and a diagnostic sensitivity and specifcity of 100% and 47.2%, respectively. The optimal cut-of value of lecithin of the HBV-carrier and HCC groups was 132.85 mg/L, with a diagnostic sensitivity and specifcity of 88.9% and 66.7%, respectively. The optimal cut-of value of oleic acid amide of the healthy and HCC groups was 129.03 mg/L, with a diagnostic sensitivity and specifcity of 88.4% and 83.3%, respectively. -

Acetylcholine Signaling System in Progression of Lung Cancers
Pharmacology & Therapeutics 194 (2019) 222–254 Contents lists available at ScienceDirect Pharmacology & Therapeutics journal homepage: www.elsevier.com/locate/pharmthera Acetylcholine signaling system in progression of lung cancers Jamie R. Friedman a,1, Stephen D. Richbart a,1,JustinC.Merritta,KathleenC.Browna, Nicholas A. Nolan a, Austin T. Akers a, Jamie K. Lau b, Zachary R. Robateau a, Sarah L. Miles a,PiyaliDasguptaa,⁎ a Department of Biomedical Sciences, Joan C. Edwards School of Medicine, 1700 Third Avenue, Huntington, WV 25755 b Biology Department, Center for the Sciences, Box 6931, Radford University, Radford, Virginia 24142 article info abstract Available online 3 October 2018 The neurotransmitter acetylcholine (ACh) acts as an autocrine growth factor for human lung cancer. Several lines of evidence show that lung cancer cells express all of the proteins required for the uptake of choline (choline Keywords: transporter 1, choline transporter-like proteins) synthesis of ACh (choline acetyltransferase, carnitine acetyl- Lung cancer transferase), transport of ACh (vesicular acetylcholine transport, OCTs, OCTNs) and degradation of ACh (acetyl- Acetylcholine cholinesterase, butyrylcholinesterase). The released ACh binds back to nicotinic (nAChRs) and muscarinic Cholinergic receptors on lung cancer cells to accelerate their proliferation, migration and invasion. Out of all components Proliferation of the cholinergic pathway, the nAChR-signaling has been studied the most intensely. The reason for this trend Invasion Anti-cancer drugs is due to genome-wide data studies showing that nicotinic receptor subtypes are involved in lung cancer risk, the relationship between cigarette smoke and lung cancer risk as well as the rising popularity of electronic ciga- rettes considered by many as a “safe” alternative to smoking. -
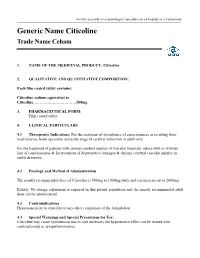
Eletriptan Smpc
For the use only of a neurologist/ specialist or a Hospital or a Laboratory Generic Name Citicoline Trade Name Ceham 1. NAME OF THE MEDICINAL PRODUCT: Citicoline 2. QUALITATIVE AND QUANTITATIVE COMPOSITION: Each film coated tablet contains: Citicoline sodium equivalent to Citicoline……………………………500mg 3. PHARMACEUTICAL FORM: Film coated tablet 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications: For the treatment of disturbance of consciousness as resulting from head injuries, brain operation and acute stage of cerebral infarction in adult only. For the treatment of patients with serious cerebral injuries of vascular traumatic nature with or without loss of consciousness & for treatment of degenerative damages & chronic cerebral vascular injuries in senile dementia. 4.2 Posology and Method of Administration The usually recommended dose of Citicoline is 500mg to 1000mg daily and can increase up to 2000mg. Elderly: No dosage adjustment is required in this patient population and the usually recommended adult dose can be administered. 4.3 Contraindications Hypersensitivity to citicoline or any other component of the formulation 4.4 Special Warnings and Special Precautions for Use: Citicoline may cause hypotension and in case necessary the hypotensive effect can be treated with corticosteroids or sympathomimetics. 4.5 Interaction with Other Medicinal Products and Other Forms of Interaction: Citicoline must not be used with medicines containing meclophenoxates (or centrophenoxine). Citicoline increases the effects of L-dopa. 4.6 Fertility, Pregnancy and Lactation There are no adequate and well controlled studies of citicoline during pregnancy and lactation. Citicoline should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. -

Alpha-GPC Introduced 2003
Product Information Sheet – January 2015 Alpha-GPC Introduced 2003 What Is It? Are There Any Potential Drug Interactions? l-Alpha-glycerophophatidylcholine (GPC-choline, alpha-GPC) is a water- At this time, there are no known adverse reactions when taken in soluble phospholipid and neurotransmitter precursor naturally conjunction with medications. occurring in the body. Unlike most membrane phospholipids, alpha- GPC is water-soluble because it lacks the hydrophobic tail groups. Alpha-GPC Uses For Alpha-GPC each Caplique® Capsule contains v 0 • Memory And Cognitive Health: Alpha-GPC passes through the alpha-GPC (L-alpha-glycerophosphatidylcholine) ........................ 200 mg blood brain barrier providing a source of choline for acetylcholine other ingredients: glycerin, water, vegetarian Caplique® Capsule (cellulose, water) and phosphatidylcholine biosynthesis. By supporting cell membrane fluidity and integrity, phosphatidylcholine enhances Contains soy healthy neurotransmitter function and signal transduction. 6 Caplique® Capsules daily, in divided doses, with or Alpha-GPC may support healthy phospholipid turnover in the between meals. brain, helping to counteract age-related cellular breakdown of membrane phospholipids. Acetylcholine is a key neurotransmitter Caplique® Capsule is a registered trademark used by Pure Encapsulations in the brain supporting memory and learning. Optimal under license. phospholipid and acetylcholine levels support cognitive, mental Each Caplique® Capsule is preserved with a nitrogen bubble, which may give the and cerebrovascular health.* appearance of the capsule not being full. Contents may appear cloudy or thick and • Growth Hormone Support: Alpha-GPC has the ability to may settle or separate. potentiate growth hormone releasing hormone (GHRH), thereby supporting healthy growth hormone (GH) levels. The mechanism of support appears to involve increased cholinergic tone.* What Is The Source? Alpha-GPC is derived from highly purified soy lecithin. -

Functional and Structural Variation Among Sticholysins, Pore-Forming Proteins from the Sea Anemone Stichodactyla Helianthus
International Journal of Molecular Sciences Review Functional and Structural Variation among Sticholysins, Pore-Forming Proteins from the Sea Anemone Stichodactyla helianthus Esperanza Rivera-de-Torre 1,2,3 , Juan Palacios-Ortega 1,2 , J. Peter Slotte 1,2, José G. Gavilanes 1, Álvaro Martínez-del-Pozo 1 and Sara García-Linares 1,* 1 Departamento de Bioquímica y Biología Molecular, Universidad Complutense, 28040 Madrid, Spain; [email protected] (E.R.-d.-T.); [email protected] (J.P.-O.); jpslotte@abo.fi (J.P.S.); [email protected] (J.G.G.); [email protected] (Á.M.-d.-P.) 2 Department of Biochemistry, Faculty of Science and Engineering, Åbo Akademi University, 20500 Turku, Finland 3 Department of Biotechnology and Biomedicine, Technical University of Denmark, 2800 Kongens Lyngby, Denmark * Correspondence: [email protected] Received: 19 October 2020; Accepted: 20 November 2020; Published: 24 November 2020 Abstract: Venoms constitute complex mixtures of many different molecules arising from evolution in processes driven by continuous prey–predator interactions. One of the most common compounds in these venomous cocktails are pore-forming proteins, a family of toxins whose activity relies on the disruption of the plasmatic membranes by forming pores. The venom of sea anemones, belonging to the oldest lineage of venomous animals, contains a large amount of a characteristic group of pore-forming proteins known as actinoporins. They bind specifically to sphingomyelin-containing membranes and suffer a conformational metamorphosis that drives them to make pores. This event usually leads cells to death by osmotic shock. Sticholysins are the actinoporins produced by Stichodactyla helianthus. Three different isotoxins are known: Sticholysins I, II, and III. -

Biochemical Development of Surface Activity in Mammalian Lung. IV
Pediat. Res. 6: 81-99 (1972) Developmental physiology lung hyaline membrane disease phospholipids infants respiratory distress syndrome lecithin surfactant Biochemical Development of Surface Activity in Mammalian Lung. IV. Pulmonary Lecithin Synthesis in the Human Fetus and Newborn and Etiology of the Respiratory Distress Syndrome Louis GLUCK1391, MARIE V. KULOVIGH, ARTHUR I. EIDELMAN, LEANDRO CORDERO, AND AIDA F. KHAZIN Department of Pediatrics, University of California, San Diego, School of Medicine, La Jolla, California, USA Extract The surface-active complex lining alveoli in normal lung lowers surface tension on ex- piration, thus preventing alveolar collapse. Surface activity follows a developmental timetable. Infants with idiopathic respiratory distress syndrome (RDS) almost ex- clusively are prematurely born, and their lungs lack adequate surface activity and are deficient in the principal surface-active component, lecithin. This deficiency implies that RDS is a "disease of development," with fetal and neonatal timetables for lecithin synthesis. The biosynthesis of lung lecithin in the living human infant was studied by examining phospholipids in lung effluent (pharyngeal aspirates, mucus), which have identical phospholipids to those in lung lavage (alveolar wash). The fatty acid esters of isolated lecithin and phosphatidyl dimethylethanolamine (PDME) were examined. The fi-carbon fatty acids are indicators of the primary pathways of synthesis of lecithin: (1) a preponderance of palmitic acid signifying cytidine diphosphate choline (CDP-choline) + D-a,{3-diglyceride -+lecithin (choline incorporation pathway) and (2) a preponder- ance of myristic acid signifying phosphatidyl ethanolamine (PE) + 2 CH3 —»• PDME + CHZ —> lecithin (methylation pathway). Fetal lung of 18 and 20 weeks showed slight incorporation by GDP-choline pathway, absence of PDME, and almost no methylation. -

Présentation Powerpoint
Table S1- List of metabolites analyzed with the AbsoluteIDQ p180 kit Metabolite Short name Biochemical Name Metabolite Short name Biochemical Name Class Class C0 L-Carnitine Ala Alanine C10 Decanoyl-L-carnitine Arg Arginine C10:1 Decenoyl-L-carnitine Asn Asparagine C10:2 Decadienyl-L-carnitine Asp Aspartate C12 Dodecanoyl-L-carnitine Cit Citrulline C12:1 Dodecenoyl-L-carnitine Gln Glutamine C12-DC Dodecanedioyl-L-carnitine Glu Glutamate C14 Tetradecanoyl-L-carnitine Gly Glycine C14:1 Tetradecenoyl-L-carnitine His Histidine C14:1-OH Hydroxytetradecenoyl-L-carnitine acids Ile Isoleucine C14:2 Tetradecadienyl-L-carnitine Leu Leucine C14:2-OH Hydroxytetradecadienyl-L-carnitine Lys Lysine C16 Hexadecanoyl-L-carnitine C16:1 Hexadecenoyl-L-carnitine Met Methionine C16:1-OH Hydroxyhexadecenoyl-L-carnitine Orn Ornithine C16:2 Hexadecadienyl-L-carnitine Amino Phe Phenylalanine C16:2-OH Hydroxyhexadecadienyl-L-carnitine Pro Proline Ser Serine carnitines C16-OH Hydroxyhexadecanoyl-L-carnitine - C18 Octadecanoyl-L-carnitine Thr Threonine L - C18:1 Octadecenoyl-L-carnitine Trp Tryptophan C18:1-OH Hydroxyoctadecenoyl-L-carnitine Tyr Tyrosine C18:2 Octadecadienyl-L-carnitine Val Valine acyl C2 Acetyl-L-carnitine Ac-Orn Acetylornithine C3 Propionyl-L-carnitine ADMA Asymmetric dimethylarginine & C3:1 Propenyl-L-carnitine SDMA Symmetric dimethylarginine C3-DC / C4-OH Malonyl-L-carnitine / Hydroxybutyryl-L- alpha-AAA alpha-Aminoadipic acid carnitine Carnosine Carnosine C3-DC-M / C5-OH Methylmalonyl-L-carnitine / Creatinine Creatinine Hydroxyvaleryl-L-carnitine -

Effect of Exogenous Lecithin on Ethanol- Induced Testicular Injuries
Indian J Physiol Pharmacol 2005; 49 (3) : 297–304 EFFECT OF EXOGENOUS LECITHIN ON ETHANOL-INDUCED TESTICULAR INJURIES IN WISTAR RATS M. MANEESH*, H. JAYALEKSHMI*, SANJIBA DUTTA**, AMIT CHAKRABARTI*** AND D. M. VASUDEVAN@ Department of *Biochemistry, **Psychiatry and ***Pharmacology, Sikkim Manipal Institute of Medical Sciences, Gangtok – 737 102 and @Department of Biochemistry, Amrita Institute of Medical Sciences, Kochi – 662 026 ( Received on November 22, 2004 ) Abstract : Infertility is well-established harmful effect in chronic alcoholism and so far, there is no effective treatment for this condition. The study was conducted to determine the effects of lecithin, a known hepatoprotective on ethanol induced testicular injuries in male albino rats of Wistar strain. Five groups (n=6) of animals were used. Group I served as control. Group II received daily 1.6 g ethanol/kg body weight/day for 4 weeks orally. Group III received 1.6 g ethanol + 500 mg lecithin/kg body weight/day for four weeks orally. Group IV received 1.6 g ethanol/kg body weight for/day 4 weeks and followed by 500 mg lecithin/kg body weight/ day for four weeks orally. Group V received 1.6 g ethanol/kg body weight/ day orally for 4 weeks, followed by 4 weeks abstinence. Twenty-four hours after the last treatment the rats were sacrificed using anesthetic ether. Testes were removed and used for the estimation of extent of lipid peroxidation and tissue levels of antioxidants and steroidogenic enzymes. Lecithin protected testes from ethanol induced oxidative stress. However, the drug did not show any considerable effect on the activities of testicular ∆ 5, 3β-HSD and 17β-HSD. -

The Relationship Between Choline Bioavailability from Diet, Intestinal Microbiota Composition, and Its Modulation of Human Diseases
nutrients Review The Relationship between Choline Bioavailability from Diet, Intestinal Microbiota Composition, and Its Modulation of Human Diseases Natalia Arias 1,2,*, Silvia Arboleya 3 , Joseph Allison 2, Aleksandra Kaliszewska 2, Sara G. Higarza 1,4 , Miguel Gueimonde 3 and Jorge L. Arias 1,4 1 Instituto de Neurociencias del Principado de Asturias (INEUROPA), 33003 Oviedo, Asturias, Spain; [email protected] (S.G.H.); [email protected] (J.L.A.) 2 Department of Basic and Clinical Neuroscience, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, Denmark Hill, London SE5 8AF, UK; [email protected] (J.A.); [email protected] (A.K.) 3 Department of Microbiology and Biochemistry of Dairy Products, Instituto de Productos Lácteos de Asturias (IPLA-CSIC), 33003 Oviedo, Asturias, Spain; [email protected] (S.A.); [email protected] (M.G.) 4 Laboratory of Neuroscience, Department of Psychology, University of Oviedo, Plaza Feijóo, s/n, 33003 Oviedo, Asturias, Spain * Correspondence: [email protected] Received: 14 July 2020; Accepted: 30 July 2020; Published: 5 August 2020 Abstract: Choline is a water-soluble nutrient essential for human life. Gut microbial metabolism of choline results in the production of trimethylamine (TMA), which, upon absorption by the host is converted into trimethylamine-N-oxide (TMAO) in the liver. A high accumulation of both components is related to cardiovascular disease, inflammatory bowel disease, non-alcoholic fatty liver disease, and chronic kidney disease. However, the relationship between the microbiota production of these components and its impact on these diseases still remains unknown. In this review, we will address which microbes contribute to TMA production in the human gut, the extent to which host factors (e.g., the genotype) and diet affect TMA production, and the colonization of these microbes and the reversal of dysbiosis as a therapy for these diseases. -

Spray-Dried Bioadhesive Formulations for Pulmonary Delivery
SPRAY-DRIED BIOADHESIVE FORMULATIONS FOR PULMONARY DELIVERY BY HUNER KAMAL OMER A THESIS SUBMITTED IN PARTIAL FULFILMENT FOR THE REQUIRMENTS OF THE DEGREE OF DOCTOR OF PHILOSOPHY AT THE UNIVERSITY OF CENTRAL LANCASHIRE July/2014 ABSTRACT This study describes developments and in vitro characterisation of lipid microparticles prepared using spray-drying for drug delivery to the lung via dry powder inhalers. Bioadhesive formulations such as prochitosome or chitosome powders have been introduced to overcome the drawbacks of liposome instability and potentially provide significant increase in the residence time of drug in the lung. Mannitol or lactose monohydrate (LMH) aqueous solutions were spray dried at inlet temperatures of 90, 130, 170 or 210ºC. Soy phosphatidylcholine and cholestrol (1:1 mole ratio) were used in all formulations. Cholesterol was added to increase vesicle membrane rigidity. Proliposomes containing salbutamol sulphate (SS) were prepared by incorporating various lipid:carrier (mannitol or LMH; 1:2, 1:4, 1:6, 1:8 and 1:10 w/w). Prochitosomes including SS or beclomethason dipropionate (BDP) were prepared by adding various chitosan glutamate:lipid ratios of 1:10, 2:10, 3:10 and 5:10 w/w. Chitosomes, including various cryoprotectants (mannitol, LMH, trehalose or sucrose), were prepared by including chitosan glutamate to liposomes generated from ethanol-based proliposomes in the ratio of 3:10 w/w chitosan to lipid. The spray-drying parameters for generation of dry powders were optimised by using an inlet temperature of 120ºC, outlet temperature of 73 ± 3°C, aspirator rate of 100%, suspension feed rate of 11%, and spray flow rate of 600 L/h using B-290 Buchi mini spray-dryer.