Role of Citicoline in the Management of Traumatic Brain Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lifestyle Drugs” for Men and Women
Development of “Lifestyle Drugs” for Men and Women Armin Schultz CRS - Clinical Research Services Mannheim GmbH AGAH Annual Meeting 2012, Leipzig, March 01 - 02 Lifestyle drugs Smart drugs, Quality-of-life drugs, Vanity drugs etc. Lifestyle? Lifestyle-Drugs? Active development? Discovery by chance? AGAH Annual Meeting 2012, Leipzig, March 01 - 02 Lifestyle A lifestyle is a characteristic bundle of behaviors that makes sense to both others and oneself in a given time and place, including social relations, consumption, entertainment, and dress. The behaviors and practices within lifestyles are a mixture of habits, conventional ways of doing things, and reasoned actions „Ein Lebensstil ist [...] der regelmäßig wiederkehrende Gesamtzusammenhang der Verhaltensweisen, Interaktionen, Meinungen, Wissensbestände und bewertenden Einstellungen eines Menschen“ (Hradil 2005: 46) Different definitions in social sciences, philosophy, psychology or medicine AGAH Annual Meeting 2012, Leipzig, March 01 - 02 Lifestyle Many “subdivisions” LOHAS: “Lifestyles of Health and Sustainability“ LOVOS: “Lifestyles of Voluntary Simplicity“ SLOHAS: “Slow Lifestyles of Happiness and Sustainability” PARKOS: “Partizipative Konsumenten“ ……. ……. ……. AGAH Annual Meeting 2012, Leipzig, March 01 - 02 Lifestyle drugs Lifestyle drug is an imprecise term commonly applied to medications which treat non-life threatening and non-painful conditions such as baldness, impotence, wrinkles, or acne, without any medical relevance at all or only minor medical relevance relative to others. Desire for increase of personal well-being and quality of life It is sometimes intended as a pejorative, bearing the implication that the scarce medical research resources allocated to develop such drugs were spent frivolously when they could have been better spent researching cures for more serious medical conditions. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

Acetylcholine Signaling System in Progression of Lung Cancers
Pharmacology & Therapeutics 194 (2019) 222–254 Contents lists available at ScienceDirect Pharmacology & Therapeutics journal homepage: www.elsevier.com/locate/pharmthera Acetylcholine signaling system in progression of lung cancers Jamie R. Friedman a,1, Stephen D. Richbart a,1,JustinC.Merritta,KathleenC.Browna, Nicholas A. Nolan a, Austin T. Akers a, Jamie K. Lau b, Zachary R. Robateau a, Sarah L. Miles a,PiyaliDasguptaa,⁎ a Department of Biomedical Sciences, Joan C. Edwards School of Medicine, 1700 Third Avenue, Huntington, WV 25755 b Biology Department, Center for the Sciences, Box 6931, Radford University, Radford, Virginia 24142 article info abstract Available online 3 October 2018 The neurotransmitter acetylcholine (ACh) acts as an autocrine growth factor for human lung cancer. Several lines of evidence show that lung cancer cells express all of the proteins required for the uptake of choline (choline Keywords: transporter 1, choline transporter-like proteins) synthesis of ACh (choline acetyltransferase, carnitine acetyl- Lung cancer transferase), transport of ACh (vesicular acetylcholine transport, OCTs, OCTNs) and degradation of ACh (acetyl- Acetylcholine cholinesterase, butyrylcholinesterase). The released ACh binds back to nicotinic (nAChRs) and muscarinic Cholinergic receptors on lung cancer cells to accelerate their proliferation, migration and invasion. Out of all components Proliferation of the cholinergic pathway, the nAChR-signaling has been studied the most intensely. The reason for this trend Invasion Anti-cancer drugs is due to genome-wide data studies showing that nicotinic receptor subtypes are involved in lung cancer risk, the relationship between cigarette smoke and lung cancer risk as well as the rising popularity of electronic ciga- rettes considered by many as a “safe” alternative to smoking. -
Eletriptan Smpc
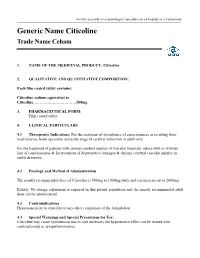
For the use only of a neurologist/ specialist or a Hospital or a Laboratory Generic Name Citicoline Trade Name Ceham 1. NAME OF THE MEDICINAL PRODUCT: Citicoline 2. QUALITATIVE AND QUANTITATIVE COMPOSITION: Each film coated tablet contains: Citicoline sodium equivalent to Citicoline……………………………500mg 3. PHARMACEUTICAL FORM: Film coated tablet 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications: For the treatment of disturbance of consciousness as resulting from head injuries, brain operation and acute stage of cerebral infarction in adult only. For the treatment of patients with serious cerebral injuries of vascular traumatic nature with or without loss of consciousness & for treatment of degenerative damages & chronic cerebral vascular injuries in senile dementia. 4.2 Posology and Method of Administration The usually recommended dose of Citicoline is 500mg to 1000mg daily and can increase up to 2000mg. Elderly: No dosage adjustment is required in this patient population and the usually recommended adult dose can be administered. 4.3 Contraindications Hypersensitivity to citicoline or any other component of the formulation 4.4 Special Warnings and Special Precautions for Use: Citicoline may cause hypotension and in case necessary the hypotensive effect can be treated with corticosteroids or sympathomimetics. 4.5 Interaction with Other Medicinal Products and Other Forms of Interaction: Citicoline must not be used with medicines containing meclophenoxates (or centrophenoxine). Citicoline increases the effects of L-dopa. 4.6 Fertility, Pregnancy and Lactation There are no adequate and well controlled studies of citicoline during pregnancy and lactation. Citicoline should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. -

More Treatments on Deck for Alcohol Use Disorder
News & Analysis Medical News & Perspectives More Treatments on Deck for Alcohol Use Disorder Jeff Lyon hirteen years have passed since the Raye Z. Litten, PhD, acting director of the ment for AUD were actually prescribed an US Food and Drug Administration NIAAA’s Division of Medications Develop- AUD medication. T (FDA) last approved a new medica- ment and principal investigator of the trial, It is a complicated problem, says John tion to help the nation’s millions of people says the agency is “excited.” Rotrosen, MD, a psychiatrist and addiction withalcoholusedisorder(AUD)stopormod- Nevertheless, the science of alcohol ad- specialist at New York University School of erate their drinking. diction has seen its share of medicines that Medicine. “To a large extent primary care Only 3 such formulations exist, and 1, failed to live up to their early promise dur- physicians don’t screen for alcoholism,” he disulfiram, dates to the Prohibition era. ing full-scale testing. So Litten said the said. “When they do, they may note it, but Known commercially as Antabuse and agency isn’t putting all its eggs in one bas- don’t really do anything about it.” introduced in 1923, it makes people memo- ket. “You need as many weapons as pos- As far as the failure to prescribe exist- rably ill if they ingest alcohol, but it doesn’t sible to treat a complex disease like alcohol ing medications for AUD, Rotrosen blames stop the cravings. The other 2, naltrexone use disorder,” he said. a lack of knowledge. “A lot of doctors in and acamprosate, approved in 1994 and But therein lies a second difficulty. -

Alpha-GPC Introduced 2003
Product Information Sheet – January 2015 Alpha-GPC Introduced 2003 What Is It? Are There Any Potential Drug Interactions? l-Alpha-glycerophophatidylcholine (GPC-choline, alpha-GPC) is a water- At this time, there are no known adverse reactions when taken in soluble phospholipid and neurotransmitter precursor naturally conjunction with medications. occurring in the body. Unlike most membrane phospholipids, alpha- GPC is water-soluble because it lacks the hydrophobic tail groups. Alpha-GPC Uses For Alpha-GPC each Caplique® Capsule contains v 0 • Memory And Cognitive Health: Alpha-GPC passes through the alpha-GPC (L-alpha-glycerophosphatidylcholine) ........................ 200 mg blood brain barrier providing a source of choline for acetylcholine other ingredients: glycerin, water, vegetarian Caplique® Capsule (cellulose, water) and phosphatidylcholine biosynthesis. By supporting cell membrane fluidity and integrity, phosphatidylcholine enhances Contains soy healthy neurotransmitter function and signal transduction. 6 Caplique® Capsules daily, in divided doses, with or Alpha-GPC may support healthy phospholipid turnover in the between meals. brain, helping to counteract age-related cellular breakdown of membrane phospholipids. Acetylcholine is a key neurotransmitter Caplique® Capsule is a registered trademark used by Pure Encapsulations in the brain supporting memory and learning. Optimal under license. phospholipid and acetylcholine levels support cognitive, mental Each Caplique® Capsule is preserved with a nitrogen bubble, which may give the and cerebrovascular health.* appearance of the capsule not being full. Contents may appear cloudy or thick and • Growth Hormone Support: Alpha-GPC has the ability to may settle or separate. potentiate growth hormone releasing hormone (GHRH), thereby supporting healthy growth hormone (GH) levels. The mechanism of support appears to involve increased cholinergic tone.* What Is The Source? Alpha-GPC is derived from highly purified soy lecithin. -

Drug-Excipient Interaction and Its Importance in Dosage Form
Journal of Applied Pharmaceutical Science 01 (06); 2011: 66-71 ISSN: 2231-3354 Drug-excipient interacti on and its importance in Received: 29-07-2011 Revised on: 02-08-2011 Accepted: 04-08-2011 dosage form development Nishath Fathima, Tirunagari Mamatha, Husna Kanwal Qureshi, Nandagopal Anitha and Jangala Venkateswara Rao ABSTRACT Excipients are included in dosage forms to aid manufacture, administration or absorption. Although considered pharmacologically inert, excipients can initiate, propagate or participate in Nishath Fathima, Tirunagari chemical or physical interactions with drug compounds, which may compromise the effectiveness Mamatha, Husna Kanwal Qureshi, of a medication. Exicipients are not exquisitely pure. Even for the most commonly used excipients, Nandagopal Anitha and Jangala it is necessary to understand the context of their manufacture in order to identify potential active pharmaceutical ingredients interactions with trace components. Chemical interactions can lead to Venkateswara Rao Sultan-Ul-Uloom College of Pharmacy, degradation of the active ingredient, thereby reducing the amount available for therapeutic effect. Physical interactions can affect rate of dissolution, uniformity of dose or ease of administration. Banjara Hills, Hyderabad - 500034, A.P., India. Key words: Excipient, Drug, Interaction, Physical, Chemical. INTRODUCTION Pharmaceutical dosage form is a combination of active pharmaceutical ingredients (API) and excipients. Excipients are included in dosage forms to aid manufacture, administration or absorption (Crowley and Martini).The ideal excipients must be able to fulfill the important functions i.e. dose, stability and release of API from the formulation. Although considered pharmacologically inert, excipients can initiate, propagate or participate in chemical or physical interactions with drug compounds, which may compromise the effectiveness of a medication. -

Effect of Combined Therapy with Thrombolysis and Citicoline in a Rat
Journal of the Neurological Sciences 247 (2006) 121–129 www.elsevier.com/locate/jns Effect of combined therapy with thrombolysis and citicoline in a rat model of embolic stroke ⁎ María Alonso de Leciñana a,e, , María Gutiérrez a,d, Jose María Roda a,c, Fernando Carceller a,c, Exuperio Díez-Tejedor a,b a Cerebrovascular Research Unit, La Paz University Hospital, Universidad Autónoma de Madrid, Madrid, Spain b Department of Neurology, La Paz University Hospital, Madrid, Spain c Department of Neurosurgery, La Paz University Hospital, Madrid, Spain d Cerebrovascular Experimental Lab, La Paz University Hospital, Madrid, Spain e Department of Neurology, Ramón y Cajal University Hospital, Madrid, Spain Received 28 April 2005; received in revised form 3 January 2006; accepted 3 March 2006 Available online 22 June 2006 Abstract An approach combining reperfusion mediated by thrombolytics with pharmacological neuroprotection aimed at inhibiting the physiopathological disorders responsible for ischemia-reperfusion damage, could provide an optimal treatment of ischemic stroke. We investigate, in a rat embolic stroke model, the combination of rtPA with citicoline as compared to either alone as monotherapy, and whether the neuroprotector should be provided before or after thrombolysis to achieve a greater reduction of ischemic brain damage. One hundred and nine rats have been studied: four were sham-operated and the rest embolized in the right internal carotid artery with an autologous clot and divided among 5 groups: 1) control; 2) iv rtPA 5 mg/kg 30 min post-embolization 3) citicoline 250 mg/kg ip ×3 doses, 10 min, 24 h and 48 h post-embolization; 4) citicoline combined with rtPA following the same pattern; 5) rtPA combined with citicoline, with a first dose 10 min after thrombolysis. -

DNA Modifications in Models of Alcohol Use Disorders
Alcohol 60 (2017) 19e30 Contents lists available at ScienceDirect Alcohol journal homepage: http://www.alcoholjournal.org/ DNA modifications in models of alcohol use disorders * Christopher T. Tulisiak a, R. Adron Harris a, b, Igor Ponomarev a, b, a Waggoner Center for Alcohol and Addiction Research, The University of Texas at Austin, 2500 Speedway, A4800, Austin, TX 78712, USA b The College of Pharmacy, The University of Texas at Austin, 2409 University Avenue, A1900, Austin, TX 78712, USA article info abstract Article history: Chronic alcohol use and abuse result in widespread changes to gene expression, some of which Received 2 September 2016 contribute to the development of alcohol-use disorders (AUD). Gene expression is controlled, in part, by a Received in revised form group of regulatory systems often referred to as epigenetic factors, which includes, among other 3 November 2016 mechanisms, chemical marks made on the histone proteins around which genomic DNA is wound to Accepted 5 November 2016 form chromatin, and on nucleotides of the DNA itself. In particular, alcohol has been shown to perturb the epigenetic machinery, leading to changes in gene expression and cellular functions characteristic of Keywords: AUD and, ultimately, to altered behavior. DNA modifications in particular are seeing increasing research Alcohol fi Epigenetics in the context of alcohol use and abuse. To date, studies of DNA modi cations in AUD have primarily fi fi fi DNA methylation looked at global methylation pro les in human brain and blood, gene-speci c methylation pro les in DNMT animal models, methylation changes associated with prenatal ethanol exposure, and the potential DNA hydroxymethylation therapeutic abilities of DNA methyltransferase inhibitors. -

Anticraving Therapy for Alcohol Use Disorder: a Clinical Review
Received: 10 April 2018 | Revised: 11 June 2018 | Accepted: 11 June 2018 DOI: 10.1002/npr2.12028 INVITED REVIEW Anticraving therapy for alcohol use disorder: A clinical review Winston W. Shen1,2 1Department of Psychiatry, Wan Fang Medical Center, Taipei Medical University, Abstract Taipei, Taiwan Aim: In this review, the author focused on anticraving therapy for alcohol use disor- 2Department of Psychiatry, College of der (AUD) defined by DMS‐5. A comprehensive review was carried out on the avail- Medicine, Taipei Medical University, Taipei, Taiwan able published papers on anticraving drugs for treating AUD patients. Methods: The author described all drugs with anticraving benefits for treating Correspondence Winston W. Shen, Department of AUD patients approved by the Food and Drug Administration of the United States Psychiatry, Wan Fang Medical Center, No. (US FDA) and European Medicines Agency of the European Union. Then, the com- 111, Section 3, Hsing Long Road, Taipei 116, Taiwan. monly prescribed anticraving drugs and those under development were also Email: [email protected] described. Results: The US FDA‐approved anticraving drugs included acamprosate and naltrex- one, and those approved by European Medicines Agency were gamma‐hydroxybuty- rate and nalmefene. The author also highlighted topiramate, gabapentin, ondansetron, LY196044, ifenprodil, varenicline, ABT‐436, mifepristone, citicoline, and baclofen. The putative mechanisms of action of and the use in clinical practice of those anticraving drugs were also described. Conclusion: Although slowly developing, the field of anticraving drugs is getting into shape as a promising entity of a pharmaceutical class of drugs. Then, the author addressed on the underused issues of those recommended, and suggested anticraving drugs by the practice guideline of the American Psychiatric Association. -

A Single-Label Phenylpyrrolocytidine Provides a Molecular Beacon-Like Response Reporting HIV-1 RT Rnase H Activity Alexander S
1048–1056 Nucleic Acids Research, 2010, Vol. 38, No. 3 Published online 20 November 2009 doi:10.1093/nar/gkp1022 A single-label phenylpyrrolocytidine provides a molecular beacon-like response reporting HIV-1 RT RNase H activity Alexander S. Wahba1, Abbasali Esmaeili2, Masad J. Damha1 and Robert H. E. Hudson3,* 1Department of Chemistry, McGill University, Montreal, QC, H3A 2K6 Canada, 2Department of Chemistry, University of Birjand, Birjand, Iran and 3Department of Chemistry, University of Western Ontario, London, ON, N6A 5B7 Canada Downloaded from https://academic.oup.com/nar/article/38/3/1048/3112336 by guest on 27 September 2021 Received August 15, 2009; Revised and Accepted October 19, 2009 ABSTRACT identified as a potential target for antiretroviral therapy as it is required for virus infectivity (3); yet there are no 6-Phenylpyrrolocytidine (PhpC), a structurally con- antiRNase H agents in clinical use. Few inhibitors of HIV- servative and highly fluorescent cytidine analog, 1 RNase H were identified until the transition of testing was incorporated into oligoribonucleotides. The methods from gel-based techniques to fluorescent assays PhpC-containing RNA formed native-like duplex amenable to high-throughput screening (HTS) (4–8). The structures with complementary DNA or RNA. The most widely used assay was developed by Parniak and co- PhpC-modification was found to act as a sensitive workers (6) and utilizes a two label, molecular beacon reporter group being non-disruptive to structure and strategy (9) in which the RNA strand is labeled with a 0 the enzymatic activity of RNase H. A RNA/DNA 3 -terminal fluorophore (fluorescein, F) and a DNA 0 hybrid possessing a single PhpC insert was an strand with a quencher (dabcyl, Q) at the 5 -terminus excellent substrate for HIV-1 RT Ribonuclease H (Scheme 1). -

Présentation Powerpoint
Table S1- List of metabolites analyzed with the AbsoluteIDQ p180 kit Metabolite Short name Biochemical Name Metabolite Short name Biochemical Name Class Class C0 L-Carnitine Ala Alanine C10 Decanoyl-L-carnitine Arg Arginine C10:1 Decenoyl-L-carnitine Asn Asparagine C10:2 Decadienyl-L-carnitine Asp Aspartate C12 Dodecanoyl-L-carnitine Cit Citrulline C12:1 Dodecenoyl-L-carnitine Gln Glutamine C12-DC Dodecanedioyl-L-carnitine Glu Glutamate C14 Tetradecanoyl-L-carnitine Gly Glycine C14:1 Tetradecenoyl-L-carnitine His Histidine C14:1-OH Hydroxytetradecenoyl-L-carnitine acids Ile Isoleucine C14:2 Tetradecadienyl-L-carnitine Leu Leucine C14:2-OH Hydroxytetradecadienyl-L-carnitine Lys Lysine C16 Hexadecanoyl-L-carnitine C16:1 Hexadecenoyl-L-carnitine Met Methionine C16:1-OH Hydroxyhexadecenoyl-L-carnitine Orn Ornithine C16:2 Hexadecadienyl-L-carnitine Amino Phe Phenylalanine C16:2-OH Hydroxyhexadecadienyl-L-carnitine Pro Proline Ser Serine carnitines C16-OH Hydroxyhexadecanoyl-L-carnitine - C18 Octadecanoyl-L-carnitine Thr Threonine L - C18:1 Octadecenoyl-L-carnitine Trp Tryptophan C18:1-OH Hydroxyoctadecenoyl-L-carnitine Tyr Tyrosine C18:2 Octadecadienyl-L-carnitine Val Valine acyl C2 Acetyl-L-carnitine Ac-Orn Acetylornithine C3 Propionyl-L-carnitine ADMA Asymmetric dimethylarginine & C3:1 Propenyl-L-carnitine SDMA Symmetric dimethylarginine C3-DC / C4-OH Malonyl-L-carnitine / Hydroxybutyryl-L- alpha-AAA alpha-Aminoadipic acid carnitine Carnosine Carnosine C3-DC-M / C5-OH Methylmalonyl-L-carnitine / Creatinine Creatinine Hydroxyvaleryl-L-carnitine