Spray-Dried Bioadhesive Formulations for Pulmonary Delivery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Role of Citicoline in the Management of Traumatic Brain Injury
pharmaceuticals Review Role of Citicoline in the Management of Traumatic Brain Injury Julio J. Secades Medical Department, Ferrer, 08029 Barcelona, Spain; [email protected] Abstract: Head injury is among the most devastating types of injury, specifically called Traumatic Brain Injury (TBI). There is a need to diminish the morbidity related with TBI and to improve the outcome of patients suffering TBI. Among the improvements in the treatment of TBI, neuroprotection is one of the upcoming improvements. Citicoline has been used in the management of brain ischemia related disorders, such as TBI. Citicoline has biochemical, pharmacological, and pharmacokinetic characteristics that make it a potentially useful neuroprotective drug for the management of TBI. A short review of these characteristics is included in this paper. Moreover, a narrative review of almost all the published or communicated studies performed with this drug in the management of patients with head injury is included. Based on the results obtained in these clinical studies, it is possible to conclude that citicoline is able to accelerate the recovery of consciousness and to improve the outcome of this kind of patient, with an excellent safety profile. Thus, citicoline could have a potential role in the management of TBI. Keywords: CDP-choline; citicoline; pharmacological neuroprotection; brain ischemia; traumatic brain injury; head injury Citation: Secades, J.J. Role of 1. Introduction Citicoline in the Management of Traumatic brain injury (TBI) is among the most devastating types of injury and can Traumatic Brain Injury. result in a different profile of neurological and cognitive deficits, and even death in the most Pharmaceuticals 2021, 14, 410. -

Acetylcholine Signaling System in Progression of Lung Cancers
Pharmacology & Therapeutics 194 (2019) 222–254 Contents lists available at ScienceDirect Pharmacology & Therapeutics journal homepage: www.elsevier.com/locate/pharmthera Acetylcholine signaling system in progression of lung cancers Jamie R. Friedman a,1, Stephen D. Richbart a,1,JustinC.Merritta,KathleenC.Browna, Nicholas A. Nolan a, Austin T. Akers a, Jamie K. Lau b, Zachary R. Robateau a, Sarah L. Miles a,PiyaliDasguptaa,⁎ a Department of Biomedical Sciences, Joan C. Edwards School of Medicine, 1700 Third Avenue, Huntington, WV 25755 b Biology Department, Center for the Sciences, Box 6931, Radford University, Radford, Virginia 24142 article info abstract Available online 3 October 2018 The neurotransmitter acetylcholine (ACh) acts as an autocrine growth factor for human lung cancer. Several lines of evidence show that lung cancer cells express all of the proteins required for the uptake of choline (choline Keywords: transporter 1, choline transporter-like proteins) synthesis of ACh (choline acetyltransferase, carnitine acetyl- Lung cancer transferase), transport of ACh (vesicular acetylcholine transport, OCTs, OCTNs) and degradation of ACh (acetyl- Acetylcholine cholinesterase, butyrylcholinesterase). The released ACh binds back to nicotinic (nAChRs) and muscarinic Cholinergic receptors on lung cancer cells to accelerate their proliferation, migration and invasion. Out of all components Proliferation of the cholinergic pathway, the nAChR-signaling has been studied the most intensely. The reason for this trend Invasion Anti-cancer drugs is due to genome-wide data studies showing that nicotinic receptor subtypes are involved in lung cancer risk, the relationship between cigarette smoke and lung cancer risk as well as the rising popularity of electronic ciga- rettes considered by many as a “safe” alternative to smoking. -

Alpha-GPC Introduced 2003
Product Information Sheet – January 2015 Alpha-GPC Introduced 2003 What Is It? Are There Any Potential Drug Interactions? l-Alpha-glycerophophatidylcholine (GPC-choline, alpha-GPC) is a water- At this time, there are no known adverse reactions when taken in soluble phospholipid and neurotransmitter precursor naturally conjunction with medications. occurring in the body. Unlike most membrane phospholipids, alpha- GPC is water-soluble because it lacks the hydrophobic tail groups. Alpha-GPC Uses For Alpha-GPC each Caplique® Capsule contains v 0 • Memory And Cognitive Health: Alpha-GPC passes through the alpha-GPC (L-alpha-glycerophosphatidylcholine) ........................ 200 mg blood brain barrier providing a source of choline for acetylcholine other ingredients: glycerin, water, vegetarian Caplique® Capsule (cellulose, water) and phosphatidylcholine biosynthesis. By supporting cell membrane fluidity and integrity, phosphatidylcholine enhances Contains soy healthy neurotransmitter function and signal transduction. 6 Caplique® Capsules daily, in divided doses, with or Alpha-GPC may support healthy phospholipid turnover in the between meals. brain, helping to counteract age-related cellular breakdown of membrane phospholipids. Acetylcholine is a key neurotransmitter Caplique® Capsule is a registered trademark used by Pure Encapsulations in the brain supporting memory and learning. Optimal under license. phospholipid and acetylcholine levels support cognitive, mental Each Caplique® Capsule is preserved with a nitrogen bubble, which may give the and cerebrovascular health.* appearance of the capsule not being full. Contents may appear cloudy or thick and • Growth Hormone Support: Alpha-GPC has the ability to may settle or separate. potentiate growth hormone releasing hormone (GHRH), thereby supporting healthy growth hormone (GH) levels. The mechanism of support appears to involve increased cholinergic tone.* What Is The Source? Alpha-GPC is derived from highly purified soy lecithin. -

Présentation Powerpoint
Table S1- List of metabolites analyzed with the AbsoluteIDQ p180 kit Metabolite Short name Biochemical Name Metabolite Short name Biochemical Name Class Class C0 L-Carnitine Ala Alanine C10 Decanoyl-L-carnitine Arg Arginine C10:1 Decenoyl-L-carnitine Asn Asparagine C10:2 Decadienyl-L-carnitine Asp Aspartate C12 Dodecanoyl-L-carnitine Cit Citrulline C12:1 Dodecenoyl-L-carnitine Gln Glutamine C12-DC Dodecanedioyl-L-carnitine Glu Glutamate C14 Tetradecanoyl-L-carnitine Gly Glycine C14:1 Tetradecenoyl-L-carnitine His Histidine C14:1-OH Hydroxytetradecenoyl-L-carnitine acids Ile Isoleucine C14:2 Tetradecadienyl-L-carnitine Leu Leucine C14:2-OH Hydroxytetradecadienyl-L-carnitine Lys Lysine C16 Hexadecanoyl-L-carnitine C16:1 Hexadecenoyl-L-carnitine Met Methionine C16:1-OH Hydroxyhexadecenoyl-L-carnitine Orn Ornithine C16:2 Hexadecadienyl-L-carnitine Amino Phe Phenylalanine C16:2-OH Hydroxyhexadecadienyl-L-carnitine Pro Proline Ser Serine carnitines C16-OH Hydroxyhexadecanoyl-L-carnitine - C18 Octadecanoyl-L-carnitine Thr Threonine L - C18:1 Octadecenoyl-L-carnitine Trp Tryptophan C18:1-OH Hydroxyoctadecenoyl-L-carnitine Tyr Tyrosine C18:2 Octadecadienyl-L-carnitine Val Valine acyl C2 Acetyl-L-carnitine Ac-Orn Acetylornithine C3 Propionyl-L-carnitine ADMA Asymmetric dimethylarginine & C3:1 Propenyl-L-carnitine SDMA Symmetric dimethylarginine C3-DC / C4-OH Malonyl-L-carnitine / Hydroxybutyryl-L- alpha-AAA alpha-Aminoadipic acid carnitine Carnosine Carnosine C3-DC-M / C5-OH Methylmalonyl-L-carnitine / Creatinine Creatinine Hydroxyvaleryl-L-carnitine -

The Effects of Α-Gpc Supplementation On
THE EFFECTS OF -GPC SUPPLEMENTATION ON GROWTH HORMONE, FAT LOSS, AND BODY COMPOSITION IN OVERWEIGHT ADULTS by WILLIAM G. MALDONADO A thesis submitted to the School of Graduate Studies Rutgers, The State University of New Jersey In partial fulfillment of the requirements For the degree of Master of Science Graduate Program in Kinesiology and Applied Physiology Written under the direction of Shawn M. Arent And approved by New Brunswick, New Jersey October, 2019 ABSTRACT OF THE THESIS The Effects of -GPC Supplementation on Growth Hormone, Fat Loss, and Body Composition in Overweight Adults By WILLIAM GERARD MALDONADO Thesis Director Shawn M. Arent In the United States, there is an increasing prevalence of obesity that is associated with health risks, and, as such, the need for effective weight loss methods is becoming increasingly more important. In the elderly, α-GPC has been shown to significantly increase growth hormone (GH) concentrations, a major stimulator of lipolysis and protein synthesis. However, very little work has been done in younger individuals. PURPOSE: to investigate if α-GPC, an acetylcholine precursor, could confer additional GH or weight loss benefits to active, overweight individuals while exercise and nutrition are maintained. METHODS: Participants were randomly assigned to either α-GPC (n=15, Mage=25.8±9.1y, MBF%=35.48±1.75%) or placebo (n=13 Mage=24.4±10.4y, MBF%=35.65±1.98%) after health/fitness screening. Both groups were instructed to consume two capsules of their respective supplement for a total of 1200 mg/day, one dose before their workout or on non-workout days with their midday meal, and the second dose before going to sleep, for eight weeks. -

The Guinea Pig Model for Organophosphate Toxicology and Therapeutic Development
THE GUINEA PIG MODEL FOR ORGANOPHOSPHATE TOXICOLOGY AND THERAPEUTIC DEVELOPMENT A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy By Christopher Ruark B.S., Miami University, 2007 M.S., Wright State University, 2010 ______________________________________ 2015 Wright State University WRIGHT STATE UNIVERSITY GRADUATE SCHOOL May 2, 2015 I HEREBY RECOMMEND THAT THE DISSERTATION PREPARED UNDER MY SUPERVISION BY Christopher Ruark ENTITLED The Guinea Pig Model for Organophosphate Toxicology and Therapeutic Development BE ACCEPTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF Doctor of Philosophy. __________________________ Jeffery M. Gearhart, Ph.D. Dissertation Director ___________________________ Mill W. Miller Ph.D. Director, Biomedical Sciences Ph.D. Program ___________________________ Robert E. W. Fyffe, Ph.D. Committee on Vice President for Research and Final Examination Dean of the Graduate School ___________________________ Jeffery M. Gearhart, Ph.D. ___________________________ Adrian M. Corbett, Ph.D. ___________________________ James B. Lucot, Ph.D. ___________________________ Mateen M. Rizki, Ph.D. ___________________________ Gerald M. Alter, Ph.D. ABSTRACT Ruark, Christopher Ph.D., Biomedical Sciences Ph.D. program, Wright State University, 2015. The Guinea Pig Model for Organophosphate Toxicology and Therapeutic Development. Organophosphates (OPs) are highly toxic insecticides and nerve agents that have been designed to inhibit the hydrolysis of acetylcholine by binding to the serine active site of acetylcholinesterase (AChE). They are one of the most common causes of human poisoning worldwide and are frequently intentionally used in suicides in agricultural areas. For this reason, there is a need for therapeutics to rescue those from intoxication. Obvious ethical concerns prevent humans from being subjected to OP exposure for therapeutic efficacy and safety testing. -

Skeletal Muscle Phosphatidylcholine and Phosphatidylethanolamine
www.nature.com/scientificreports Correction: Author Correction OPEN Skeletal muscle phosphatidylcholine and phosphatidylethanolamine respond to exercise and infuence Received: 8 December 2017 Accepted: 5 April 2018 insulin sensitivity in men Published online: 25 April 2018 Sindre Lee1,2, Frode Norheim1,3, Hanne L. Gulseth2, Torgrim M. Langleite1, Andreas Aker4, Thomas E. Gundersen4, Torgeir Holen1, Kåre I. Birkeland2,5 & Christian A. Drevon1 Phosphatidylcholine (PC) and phosphatidylethanolamine (PE) composition in skeletal muscle have been linked to insulin sensitivity. We evaluated the relationships between skeletal muscle PC:PE, physical exercise and insulin sensitivity. We performed lipidomics and measured PC and PE in m. vastus lateralis biopsies obtained from 13 normoglycemic normal weight men and 13 dysglycemic overweight men at rest, immediately after 45 min of cycling at 70% maximum oxygen uptake, and 2 h post-exercise, before as well as after 12 weeks of combined endurance- and strength-exercise intervention. Insulin sensitivity was monitored by euglycemic-hyperinsulinemic clamp. RNA-sequencing was performed on biopsies, and mitochondria and lipid droplets were quantifed on electron microscopic images. Exercise intervention for 12 w enhanced insulin sensitivity by 33%, skeletal muscle levels of PC by 21%, PE by 42%, and reduced PC:PE by 16%. One bicycle session reduced PC:PE by 5%. PC:PE correlated negatively with insulin sensitivity (β = −1.6, P < 0.001), percent area of mitochondria (ρ = −0.52, P = 0.035), and lipid droplet area (ρ = 0.55, P = 0.017) on EM pictures, and negatively with oxidative phosphorylation and mTOR based on RNA-sequencing. In conclusion, PC and PE contents of skeletal muscle respond to exercise, and PC:PE is inversely related to insulin sensitivity. -
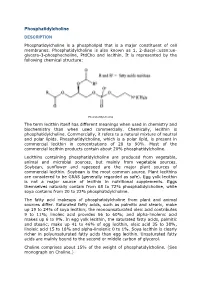
Phosphatidylcholine DESCRIPTION
Phosphatidylcholine DESCRIPTION Phosphatidylcholine is a phospholipid that is a major constituent of cell membranes. Phosphatidylcholine is also known as 1, 2-diacyl-:ussn:ue- glycero-3-phosphocholine, PtdCho and lecithin. It is represented by the following chemical structure: Phosphatidylcholine The term lecithin itself has different meanings when used in chemistry and biochemistry than when used commercially. Chemically, lecithin is phosphatidylcholine. Commercially, it refers to a natural mixture of neutral and polar lipids. Phosphatidylcholine, which is a polar lipid, is present in commercial lecithin in concentrations of 20 to 90%. Most of the commercial lecithin products contain about 20% phosphatidylcholine. Lecithins containing phosphatidylcholine are produced from vegetable, animal and microbial sources, but mainly from vegetable sources. Soybean, sunflower and rapeseed are the major plant sources of commercial lecithin. Soybean is the most common source. Plant lecithins are considered to be GRAS (generally regarded as safe). Egg yolk lecithin is not a major source of lecithin in nutritional supplements. Eggs themselves naturally contain from 68 to 72% phosphatidylcholine, while soya contains from 20 to 22% phosphatidylcholine. The fatty acid makeups of phosphatidylcholine from plant and animal sources differ. Saturated fatty acids, such as palmitic and stearic, make up 19 to 24% of soya lecithin; the monounsaturated oleic acid contributes 9 to 11%; linoleic acid provides 56 to 60%; and alpha-linolenic acid makes up 6 to 9%. In egg yolk lecithin, the saturated fatty acids, palmitic and stearic, make up 41 to 46% of egg lecithin, oleic acid 35 to 38%, linoleic acid 15 to 18% and alpha-linolenic 0 to 1%. -

Phosphatidylcholine Treatment to Induce Lipolysis
Journal Innoventions PhosphatidylcholineBlackwell Publishing Inc treatment to induce lipolysis Franz Hasengschwandtner Therapy-Clinic Center, Bad Leonfelden, Austria Summary The medicine Lipostabil N® has been in widespread use in Europe since 2002 by doctors working in the field of esthetics to achieve a reduction in the volume of smaller fat deposits by means of injections into the subcutaneous fatty tissue. The lipases released from the adipocytes by means of phosphatidylcholine produce a local breakdown of fat that is then discharged over the liver and metabolized via beta- oxidation. The medicine has been authorized for intravenous use in the prophylaxis and therapy of fat embolisms and liver diseases. Keywords: detergents, lecithins, lipolysis, phosphatidylcholine her lower eye pads by injecting phosphatidylcholine History under her eyes.2 In Europe, further study of the medica- Phosphatidylcholine was first isolated in Odessa, Ukraine ment started in 2001, and the first treatments were made some 50 years ago. This was followed by further research by the author in late 2002. In 2003 “Network Lipolysis” in Germany and Russia. It has been marketed by Sanofi- was founded in Germany by Ulrich Bunzek and Dirk Aventis for over 30 years and, at present, the substance Brandl and with this started the European investigation phosphatidylcholine is registered in 53 countries. Its main of the scientific background of this new esthetic therapy. application nowadays lies in the intravenous treatment Phosphatidylcholine makes up the largest choline and prevention of fat embolisms in polytraumatized (lecithin) reservoir in the body and is found in bile. It patients in the treatment of metabolic disorders and as a facilitates the emulsification of fat into the tiniest particles liver-protecting substance. -

The Intrinsic Pka Values for Phosphatidylcholine, Phosphatidylethanolamine, and Phosphatidylserine in Monolayers Deposited on Mercury Electrodes
Biophysical Journal Volume 66 June 1994 1969-1980 1 969 The Intrinsic pKa Values for Phosphatidylcholine, Phosphatidylethanolamine, and Phosphatidylserine in Monolayers Deposited on Mercury Electrodes Maria Rosa Moncelli, Lucia Becucci, and Rolando Guidelli Department of Chemistry, Florence University, Florence, Italy ABSTRACT The intrinsic PKa values of the phosphate groups of phosphatidyicholine (PC) and phosphatidylethanolamine (PE) and of the phosphate and carboxyl groups of phosphatidylserine (PS) in self-organized monolayers deposited on a hanging mercury drop electrode were determined by a novel procedure based on measurements of the differential capacity C of this lipid-coated electrode. In view of the Gouy-Chapman theory, plots of 1/C at constant bulk pH and variable KCI concentration against the reciprocal of the calculated diffuse-layer capacity Cdo at zero charge exhibit slopes that decrease from an almost unit value to vanishingly low values as the absolute value of the charge density on the lipid increases from zero to -2 pC cm-2. The intrinsic PKa values so determined are 0.5 for PE and 0.8 for PC. The plots of 1/C against 1/Cd 0 for pure PS exhibit slopes that pass from zero to a maximum value and then back to zero as pH is varied from 7.5 to 3, indicating that the charge density of the lipid film passes from slight negative to slight positive values over this pH range. An explanation for this anomalous behavior, which is ascribed to the phosphate group of PS, is provided. Interdispersion of PS and PC molecules in the film decreases the "formal" PKa value of the latter group by about three orders of magnitude. -
![Dimethylethanolamine (DMAE) [108-01-0] and Selected Salts](https://docslib.b-cdn.net/cover/5743/dimethylethanolamine-dmae-108-01-0-and-selected-salts-2695743.webp)
Dimethylethanolamine (DMAE) [108-01-0] and Selected Salts
Dimethylethanolamine (DMAE) [108-01-0] and Selected Salts and Esters DMAE Aceglutamate [3342-61-8] DMAE p-Acetamidobenzoate [281131-6] and [3635-74-3] DMAE Bitartrate [5988-51-2] DMAE Dihydrogen Phosphate [6909-62-2] DMAE Hydrochloride [2698-25-1] DMAE Orotate [1446-06-6] DMAE Succinate [10549-59-4] Centrophenoxine [3685-84-5] Centrophenoxine Orotate [27166-15-0] Meclofenoxate [51-68-3] Review of Toxicological Literature (Update) November 2002 Dimethylethanolamine (DMAE) [108-01-0] and Selected Salts and Esters DMAE Aceglutamate [3342-61-8] DMAE p-Acetamidobenzoate [281131-6] and [3635-74-3] DMAE Bitartrate [5988-51-2] DMAE Dihydrogen Phosphate [6909-62-2] DMAE Hydrochloride [2698-25-1] DMAE Orotate [1446-06-6] DMAE Succinate [10549-59-4] Centrophenoxine [3685-84-5] Centrophenoxine Orotate [27166-15-0] Meclofenoxate [51-68-3] Review of Toxicological Literature (Update) Prepared for Scott Masten, Ph.D. National Institute of Environmental Health Sciences P.O. Box 12233 Research Triangle Park, North Carolina 27709 Contract No. N01-ES-65402 Submitted by Karen E. Haneke, M.S. Integrated Laboratory Systems, Inc. P.O. Box 13501 Research Triangle Park, North Carolina 27709 November 2002 Toxicological Summary for Dimethylethanolamine and Selected Salts and Esters 11/2002 Executive Summary Nomination Dimethylethanolamine (DMAE) was nominated by the NIEHS for toxicological characterization, including metabolism, reproductive and developmental toxicity, subchronic toxicity, carcinogenicity and mechanistic studies. The nomination is based on the potential for widespread human exposure to DMAE through its use in industrial and consumer products and an inadequate toxicological database. Studies to address potential hazards of consumer (e.g. dietary supplement) exposures, including use by pregnant women and children, and the potential for reproductive effects and carcinogenic effects are limited. -

Choline: the Neurocognitive Essential Nutrient of Interest to Obstetricians and Gynecologists
Journal of Dietary Supplements ISSN: 1939-0211 (Print) 1939-022X (Online) Journal homepage: https://www.tandfonline.com/loi/ijds20 Choline: The Neurocognitive Essential Nutrient of Interest to Obstetricians and Gynecologists Taylor C. Wallace, Jan Krzysztof Blusztajn, Marie A. Caudill, Kevin C. Klatt & Steven H. Zeisel To cite this article: Taylor C. Wallace, Jan Krzysztof Blusztajn, Marie A. Caudill, Kevin C. Klatt & Steven H. Zeisel (2019): Choline: The Neurocognitive Essential Nutrient of Interest to Obstetricians and Gynecologists, Journal of Dietary Supplements, DOI: 10.1080/19390211.2019.1639875 To link to this article: https://doi.org/10.1080/19390211.2019.1639875 Published online: 06 Aug 2019. Submit your article to this journal View Crossmark data Full Terms & Conditions of access and use can be found at https://www.tandfonline.com/action/journalInformation?journalCode=ijds20 JOURNAL OF DIETARY SUPPLEMENTS https://doi.org/10.1080/19390211.2019.1639875 Choline: The Neurocognitive Essential Nutrient of Interest to Obstetricians and Gynecologists Taylor C. Wallace, PhD, CFS, FACNa,b, Jan Krzysztof Blusztajn, PhDc, Marie A., PhD, RD Caudilld, Kevin C. Klatt, PhDe, and Steven H., MD, PhD Zeiself aDepartment of Nutrition and Food Studies, George Mason University, Fairfax, VA, USA; bThink Healthy Group, Inc, Washington, DC, USA; cDepartment of Pathology and Laboratory Medicine, Boston University School of Medicine, Boston, MA, USA; dDivision of Nutritional Sciences, Cornell University, Ithaca, NY, USA; eUSDA/ARS Children’s Nutrition Research Center, Baylor College of Medicine, Houston, TX, USA; fResearch Institute, University of North Carolina, Kannapolis, NC, USA ABSTRACT KEYWORDS Choline is an essential nutrient for proper liver, muscle, and brain brain; choline; cognition; functions as well as for lipid metabolism and cellular membrane dietary guidelines; placenta; composition and repair.