The Relationship Between Choline Bioavailability from Diet, Intestinal Microbiota Composition, and Its Modulation of Human Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Aseptic Addition Method for Lactobacillus Casei Assay of Folate Activity in Human Serum
J Clin Pathol: first published as 10.1136/jcp.19.1.12 on 1 January 1966. Downloaded from J. clin. Path. (1966), 19, 12 Aseptic addition method for Lactobacillus casei assay of folate activity in human serum VICTOR HERBERT From the Department of Haematology, The Mount Sinai Hospital, New York, U.S.A. SYNOPSIS An 'aseptic addition' method is described for microbiological assay with Lactobacillis casei of folate activity in human serum. It has the following advantages over the previously reported 'standard' method. 1 The manipulations involved in the assay are halved, by deleting autoclaving of serum in buffers. 2 The use of 1 g. % ascorbate better preserves serum folates than the lower amounts of ascorbate which are the maximum quantities usable in the standard methods. 3 Only 03 ml. of serum is required (0 1 ml. for one sample; 02 ml. for its duplicate). Herbert, Wasserman, Frank, Pasher, and Baker in or after transfer of blood from syringes to acid-washed 1959 reported that folate deficiency could be screw-top tubes). The clots are 'rimmed' with glass rods measured in man using microbiological assay of or wooden applicator sticks, the tubes centrifuged for serum folate activity with Lactobacillus casei. Many five minutes at 3,000 r.p.m. and the supernatant serum aspirated with acid-washed or disposable pipettes andcopyright. other workers have confirmed this work (see review frozen at -20°C. until assay. On the day of assay, the by Herbert, 1965). Various minor modifications of sera are thawed. A 0-1 ml. and a 0-2 ml. -

The Effect of Selected Herbal Extracts on Lactic Acid Bacteria Activity
applied sciences Article The Effect of Selected Herbal Extracts on Lactic Acid Bacteria Activity Małgorzata Ziarno 1,* , Mariola Kozłowska 2 , Iwona Scibisz´ 3 , Mariusz Kowalczyk 4 , Sylwia Pawelec 4 , Anna Stochmal 4 and Bartłomiej Szleszy ´nski 5 1 Division of Milk Technology, Department of Food Technology and Assessment, Institute of Food Science, Warsaw University of Life Sciences–SGGW (WULS–SGGW), 02-787 Warsaw, Poland 2 Department of Chemistry, Institute of Food Science, Warsaw University of Life Sciences–SGGW (WULS–SGGW), 02-787 Warsaw, Poland; [email protected] 3 Division of Fruit, Vegetable and Cereal Technology, Department of Food Technology and Assessment, Institute of Food Science, Warsaw University of Life Sciences–SGGW (WULS–SGGW), 02-787 Warsaw, Poland; [email protected] 4 Department of Biochemistry and Crop Quality, Institute of Soil Science and Plant Cultivation, State Research Institute, 24-100 Puławy, Poland; [email protected] (M.K.); [email protected] (S.P.); [email protected] (A.S.) 5 Institute of Horticultural Sciences, Warsaw University of Life Sciences–SGGW (WULS–SGGW), 02-787 Warsaw, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-225-937-666 Abstract: This study aimed to investigate the effect of plant extracts (valerian Valeriana officinalis L., sage Salvia officinalis L., chamomile Matricaria chamomilla L., cistus Cistus L., linden blossom Tilia L., ribwort plantain Plantago lanceolata L., marshmallow Althaea L.) on the activity and growth of lactic acid bacteria (LAB) during the fermentation and passage of milk through a digestive system model. Citation: Ziarno, M.; Kozłowska, M.; The tested extracts were also characterized in terms of their content of polyphenolic compounds and Scibisz,´ I.; Kowalczyk, M.; Pawelec, S.; antioxidant activity. -

Choline for a Healthy Pregnancy
To support healthy for a Healthy weight gain and keep up with the nutritional needs of both mom and Pregnancy the developing baby, CHOLINE additional nutrients are necessary. Nine out of 10 Americans don’t meet the daily recommended choline intake of 550 mg1,2 and it can be challenging to reach this goal even when choosing choline-containing foods like beef, eggs, wheat germ and Brussels sprouts. Choline is particularly important during pregnancy for both mom and baby because it supports healthy brain growth and offers protection against neural tube defects. Women are encouraged to take a prenatal supplement before and during pregnancy to ensure they’re meeting vitamin and mineral recommendations. In fact, the American Medical Association recommends that choline be included in all prenatal vitamins to help ensure women get enough choline to maintain a normal pregnancy.3 Look for a prenatal supplement that contains folic acid, iron, DHA (omega-3s), vitamin D and choline. Consider smart swaps to get the most choline in your diet for a healthy pregnancy, as well as optimal health after baby arrives. PREGNANCY EATING PATTERN* CHOLINE-FOCUSED PREGNANCY EATING PATTERN* 1 1 hard-cooked egg 1 2 cups toasted whole grain oat cereal / 1 large peach 1 cup nonfat milk 1 1 slice whole grain bread /3 cup blueberries 1 1 tablespoon jelly /3 cup sliced banana BREAKFAST 1 cup nonfat milk 1 /2 whole grain bagel 1 whole wheat tortilla 2 tablespoons peanut butter 2 tablespoons peanut butter 1 small apple 1 SNACK 1 /2 large banana /2 cup nonfat vanilla Greek yogurt 2 slices whole grain bread 3 oz. -

Influence of Dietary Fiber Addition on the Properties of Probiotic Yogurt
International Journal of Chemical Engineering and Applications, Vol. 5, No. 5, October 2014 Influence of Dietary Fiber Addition on the Properties of Probiotic Yogurt T. Ozcan and O. Kurtuldu low energy density, and should promote satiation and satiety, Abstract—In this study, the effects of using dietary fiber and play a role in the control of energy balance. These foods barley and oat β-glucan as a prebiotic on the viability of have the capacity of binding bile acids and metabolites of Bifidobacterium bifidum in probiotic yoghurt and properties of cholesterol that play an important role in digestion and yogurt during storage were investigated. The survival of B. absorption of lipids in the small intestine, lowering blood bifidum was within biotherapeutic level (> 7 log cfu/g) as a result of the prebiotic effect of barley and oat based β-glucan. cholesterol, regulating blood glucose levels for diabetes The addition of β-glucan to yogurt significantly affected management, producing short chain fatty acids and physicochemical properties including pH, titratable acidity promoting the growth of beneficial gut microflora (i.e. as a (LA %), whey seperation, color (L*, a*, b*) and sensorial prebiotic) [18]–[23]. Due to beneficiary health effects the properties of yogurts. In conclusion, β-glucan can be used on recommended daily intake of fiber is about 38 g for men and the development of cereal-based functional dairy products with sufficient viability and acceptable sensory characteristics. 25 g for women [24]. Fiber can be used for improvement of some functional Index Terms—Yoghurt, probiotic, dietary fiber, β-glucan. properties such as texture, water holding capacity, oil holding capacity, emulsification and/or gel formation, bulking agent in reduced-sugar applications, and shelf-life of I. -

Probiotic Sufficiency™ Brochure
Everybody - Everyday - For Life!TM Everybody Everyday For Life! ® RESEARCH INDICATES THAT: 1. Probiotic bacteria are ESSENTIAL for wellness and prevention. ® The human body contains 90% microorganisms Energy and only 10% human cells. Dietary sufficiency of healthy microorganisms (probiotics) is necessary for Vitality the proper function of the digestive and immune Strength systems and for overall wellness and prevention. Balance Natural Health 2. The Western diet is DANGEROUSLY DEFICIENT in Probiotic bacteria. Purity Research shows that we now consume one millionth of the healthy probiotic bacteria that we did before pesticides, herbicides, and industrial farming. We also kill many of our probiotic bacteria with poor nutrition, prescription drugs, and stress. This PROBIOTIC deficiency of healthy probiotic bacteria is implicated TM as a casual factor in lack of health and vitality and an alarming number of preventable illnesses from SUFFICIENCY infancy to old age. The Innate Human Probiotic Formula 3. The only way to obtain sufficient amounts of Everybody - Everyday - For Life!™ ® healthy probiotic bacteria is through daily How to consume Innate Choice PROBIOTIC SUFFICIENCY™ SUPPLEMENTATION. Please visit www.innatechoice.com for The dietary sources of probiotic bacteria are virtually The World’s Premier Multi-Strain a complete list of references supporting the A Dietary Supplement to Promote unavailable in industrialized society. Our fruits Probiotic Supplement importance of daily probiotic supplementation for Healthy Intestinal Flora and vegetables are sprayed with pesticides, much Adults should consume 2 capsules per day with a meal wellness and prevention. of our food is pasteurized or irradiated, and we do containing raw fruit or vegetables. not consume sufficient amounts of fresh, raw, local foods. -

L-Carnitine, Mecobalamin and Folic Acid Tablets) TRINERVE-LC
For the use of a Registered Medical Practitioner or a Hospital or a Laboratory only (L-Carnitine, Mecobalamin and Folic acid Tablets) TRINERVE-LC 1. Name of the medicinal product Trinerve-LC Tablets 2. Qualitative and quantitative composition Each film- coated tablets contains L-Carnitine…………………….500 mg Mecobalamin……………….1500 mcg Folic acid IP…………………..1.5mg 3. Pharmaceutical form Film- coated tablets 4. Clinical particulars 4.1 Therapeutic indications Vitamin and micronutrient supplementation in the management of chronic disease. 4.2 Posology and method of administration For oral administration only. One tablet daily or as directed by physician. 4.3 Contraindications Hypersensitivity to any constituent of the product. 4.4 Special warnings and precautions for use L-Carnitine The safety and efficacy of oral L-Carnitine has not been evaluated in patients with renal insufficiency. Chronic administration of high doses of oral L-Carnitine in patients with severely compromised renal function or in ESRD patients on dialysis may result in accumulation of the potentially toxic metabolites, trimethylamine (TMA) and trimethylamine-N-oxide (TMAO), since these metabolites are normally excreted in the urine. Mecobalamin Should be given with caution in patients suffering from folate deficiency. The following warnings and precautions suggested with parent form – vitamin B12 The treatment of vitamin B12 deficiency can unmask the symptoms of polycythemia vera. Megaloblastic anemia is sometimes corrected by treatment with vitamin B12. But this can have very serious side effects. Don’t attempt vitamin B12 therapy without close supervision by healthcare provider. Do not take vitamin B12 if Leber’s disease, a hereditary eye disease. -

Analysis of the Effects of Three Commercially Available Supplements on Performance, Exercise Induced Changes and Bio-Markers in Recreationally Trained Young Males
Analysis of the effects of three commercially available supplements on performance, exercise induced changes and bio-markers in recreationally trained young males Robert Cooper A thesis is submitted in partial fulfilment of the requirements of the University of Greenwich for the Degree of Doctor of Philosophy This research programme was carried out in collaboration with GlaxoSmithKline Maxinutrition division December 2013 School of Science University of Greenwich, Medway Campus Chatham Maritime, Kent ME4 4TB, UK i DECLARATION “I certify that this work has not been accepted in substance for any degree, and is not concurrently being submitted for any degree other than that of Doctor of Philosophy being studied at the University of Greenwich. I also declare that this work is the result of my own investigations except where otherwise identified by references and that I have not plagiarised the work of others”. Signed Date Mr Robert Cooper (Candidate) …………………………………………………………………………………………………………………………… PhD Supervisors Signed Date Dr Fernando Naclerio (1st supervisor) Signed Date Dr Mark Goss-Sampson (2nd supervisor) ii ACKNOWLEDGEMENTS Thank you to my supervisory team, Dr Fernando Naclerio, Dr Mark Goss Sampson and Dr Judith Allgrove for their support and guidance throughout my PhD. Particular thanks to Dr Fernando Naclerio for his tireless efforts, guidance and support in developing the research and my own research and communication skills. Thank you to Dr Eneko Larumbe Zabala for the statistics support. I would like to take this opportunity to thank my wonderful mother and sister who continue to give me the support and drive to succeed. Also on a personal level thank you to my amazing fiancée, Jennie Swift. -

Flow Cytometric Analysis Reveals Culture-Condition Dependent Variations in Phenotypic Heterogeneity of Limosilactobacillus Reuteri
Flow Cytometric Analysis Reveals Culture-condition Dependent Variations in Phenotypic Heterogeneity of Limosilactobacillus Reuteri Nikhil Seshagiri Rao Lund University Ludwig Lundberg Swedish University of Agricultural Sciences Shuai Palmkron Lund University Sebastian Håkansson BioGaia Björn Bergenståhl Lund University Magnus Carlquist ( [email protected] ) Lund University Research Article Keywords: Physical stress, heterogeneity, morphology, freeze-thaw, freeze-drying, ow cytometry Posted Date: June 22nd, 2021 DOI: https://doi.org/10.21203/rs.3.rs-625422/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/23 Abstract Optimisation of cultivation conditions in the industrial production of probiotics is crucial to reach a high- quality product with retained probiotic functionality. Flow cytometry-based descriptors of bacterial morphology may be used as markers to estimate physiological tness during cultivation, and can be applied for online monitoring to avoid suboptimal growth. In the current study, the effects of temperature, pH and oxygen levels on cell growth and cell size distributions of Limosilactobacillus reuteri DSM 17938 were measured using multivariate ow cytometry. A pleomorphic behaviour was evident from the measurement of light scatter and pulse width distributions. A pattern of high growth yielding smaller cells and less heterogeneous populations could be observed. Analysis of pulse width distributions revealed signicant morphological heterogeneities within the bacterial cell population under non-optimal growth conditions, and pointed towards low temperature, high pH, and high oxygen levels all being triggers for changes in morphology towards cell chain formation. However, cell size did not correlate to survivability after freeze-thaw or freeze-drying stress, indicating that it is not a key determinant for physical stress tolerance. -

L-Carnitine and Acylcarnitines: Mitochondrial Biomarkers for Precision Medicine
H OH metabolites OH Review L-Carnitine and Acylcarnitines: Mitochondrial Biomarkers for Precision Medicine Marc R. McCann 1 , Mery Vet George De la Rosa 2 , Gus R. Rosania 2 and Kathleen A. Stringer 1,3,4,* 1 The NMR Metabolomics Laboratory, Department of Clinical Pharmacy, College of Pharmacy, University of Michigan, Ann Arbor, MI 48109, USA; [email protected] 2 Department of Pharmaceutical Sciences, College of Pharmacy, University of Michigan, 428 Church Street, Ann Arbor, MI 48109, USA; [email protected] (M.V.G.); [email protected] (G.R.R.) 3 Division of Pulmonary and Critical Care Medicine, Department of Medicine, School of Medicine, University of Michigan, Ann Arbor, MI 48109, USA 4 Michigan Center for Integrative Research in Critical Care, University of Michigan, Ann Arbor, MI 48109, USA * Correspondence: [email protected]; Tel.: +1-734-647-4775 Abstract: Biomarker discovery and implementation are at the forefront of the precision medicine movement. Modern advances in the field of metabolomics afford the opportunity to readily identify new metabolite biomarkers across a wide array of disciplines. Many of the metabolites are derived from or directly reflective of mitochondrial metabolism. L-carnitine and acylcarnitines are established mitochondrial biomarkers used to screen neonates for a series of genetic disorders affecting fatty acid oxidation, known as the inborn errors of metabolism. However, L-carnitine and acylcarnitines are not routinely measured beyond this screening, despite the growing evidence that shows their clinical utility outside of these disorders. Measurements of the carnitine pool have been used to identify the disease and prognosticate mortality among disorders such as diabetes, sepsis, cancer, and heart failure, as well as identify subjects experiencing adverse drug reactions from various medications like valproic acid, clofazimine, zidovudine, cisplatin, propofol, and cyclosporine. -

Clinical Significance of Small Molecule Metabolites in the Blood of Patients
www.nature.com/scientificreports OPEN Clinical signifcance of small molecule metabolites in the blood of patients with diferent types of liver injury Hui Li1,2,5, Yan Wang1,5, Shizhao Ma1,3, Chaoqun Zhang1,4, Hua Liu2 & Dianxing Sun1,4* To understand the characteristic of changes of serum metabolites between healthy people and patients with hepatitis B virus (HBV) infection at diferent stages of disease, and to provide reference metabolomics information for clinical diagnosis of liver disease patients. 255 patients with diferent stages of HBV infection were selected. 3 mL blood was collected from each patient in the morning to detect diferences in serum lysophosphatidylcholine, acetyl-l-carnitine, oleic acid amide, and glycocholic acid concentrations by UFLC-IT-TOF/MS. The diagnostic values of four metabolic substances were evaluated by receiver operating characteristic (ROC) curve. The results showed that the optimal cut-of value of oleic acid amide concentration of the liver cirrhosis and HCC groups was 23.6 mg/L, with a diagnostic sensitivity of 88.9% and specifcity of 70.6%. The diagnostic efcacies of the three substances were similar in the hepatitis and HCC groups, with an optimal cut-of value of 2.04 mg/L, and a diagnostic sensitivity and specifcity of 100% and 47.2%, respectively. The optimal cut-of value of lecithin of the HBV-carrier and HCC groups was 132.85 mg/L, with a diagnostic sensitivity and specifcity of 88.9% and 66.7%, respectively. The optimal cut-of value of oleic acid amide of the healthy and HCC groups was 129.03 mg/L, with a diagnostic sensitivity and specifcity of 88.4% and 83.3%, respectively. -
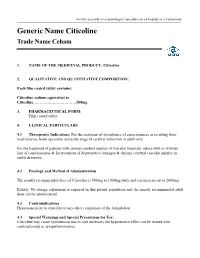
Eletriptan Smpc
For the use only of a neurologist/ specialist or a Hospital or a Laboratory Generic Name Citicoline Trade Name Ceham 1. NAME OF THE MEDICINAL PRODUCT: Citicoline 2. QUALITATIVE AND QUANTITATIVE COMPOSITION: Each film coated tablet contains: Citicoline sodium equivalent to Citicoline……………………………500mg 3. PHARMACEUTICAL FORM: Film coated tablet 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications: For the treatment of disturbance of consciousness as resulting from head injuries, brain operation and acute stage of cerebral infarction in adult only. For the treatment of patients with serious cerebral injuries of vascular traumatic nature with or without loss of consciousness & for treatment of degenerative damages & chronic cerebral vascular injuries in senile dementia. 4.2 Posology and Method of Administration The usually recommended dose of Citicoline is 500mg to 1000mg daily and can increase up to 2000mg. Elderly: No dosage adjustment is required in this patient population and the usually recommended adult dose can be administered. 4.3 Contraindications Hypersensitivity to citicoline or any other component of the formulation 4.4 Special Warnings and Special Precautions for Use: Citicoline may cause hypotension and in case necessary the hypotensive effect can be treated with corticosteroids or sympathomimetics. 4.5 Interaction with Other Medicinal Products and Other Forms of Interaction: Citicoline must not be used with medicines containing meclophenoxates (or centrophenoxine). Citicoline increases the effects of L-dopa. 4.6 Fertility, Pregnancy and Lactation There are no adequate and well controlled studies of citicoline during pregnancy and lactation. Citicoline should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. -

Alpha-GPC Introduced 2003
Product Information Sheet – January 2015 Alpha-GPC Introduced 2003 What Is It? Are There Any Potential Drug Interactions? l-Alpha-glycerophophatidylcholine (GPC-choline, alpha-GPC) is a water- At this time, there are no known adverse reactions when taken in soluble phospholipid and neurotransmitter precursor naturally conjunction with medications. occurring in the body. Unlike most membrane phospholipids, alpha- GPC is water-soluble because it lacks the hydrophobic tail groups. Alpha-GPC Uses For Alpha-GPC each Caplique® Capsule contains v 0 • Memory And Cognitive Health: Alpha-GPC passes through the alpha-GPC (L-alpha-glycerophosphatidylcholine) ........................ 200 mg blood brain barrier providing a source of choline for acetylcholine other ingredients: glycerin, water, vegetarian Caplique® Capsule (cellulose, water) and phosphatidylcholine biosynthesis. By supporting cell membrane fluidity and integrity, phosphatidylcholine enhances Contains soy healthy neurotransmitter function and signal transduction. 6 Caplique® Capsules daily, in divided doses, with or Alpha-GPC may support healthy phospholipid turnover in the between meals. brain, helping to counteract age-related cellular breakdown of membrane phospholipids. Acetylcholine is a key neurotransmitter Caplique® Capsule is a registered trademark used by Pure Encapsulations in the brain supporting memory and learning. Optimal under license. phospholipid and acetylcholine levels support cognitive, mental Each Caplique® Capsule is preserved with a nitrogen bubble, which may give the and cerebrovascular health.* appearance of the capsule not being full. Contents may appear cloudy or thick and • Growth Hormone Support: Alpha-GPC has the ability to may settle or separate. potentiate growth hormone releasing hormone (GHRH), thereby supporting healthy growth hormone (GH) levels. The mechanism of support appears to involve increased cholinergic tone.* What Is The Source? Alpha-GPC is derived from highly purified soy lecithin.