Clinical Significance of Small Molecule Metabolites in the Blood of Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -
Eletriptan Smpc
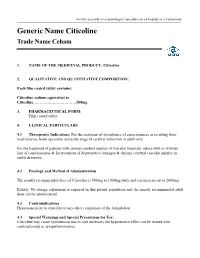
For the use only of a neurologist/ specialist or a Hospital or a Laboratory Generic Name Citicoline Trade Name Ceham 1. NAME OF THE MEDICINAL PRODUCT: Citicoline 2. QUALITATIVE AND QUANTITATIVE COMPOSITION: Each film coated tablet contains: Citicoline sodium equivalent to Citicoline……………………………500mg 3. PHARMACEUTICAL FORM: Film coated tablet 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications: For the treatment of disturbance of consciousness as resulting from head injuries, brain operation and acute stage of cerebral infarction in adult only. For the treatment of patients with serious cerebral injuries of vascular traumatic nature with or without loss of consciousness & for treatment of degenerative damages & chronic cerebral vascular injuries in senile dementia. 4.2 Posology and Method of Administration The usually recommended dose of Citicoline is 500mg to 1000mg daily and can increase up to 2000mg. Elderly: No dosage adjustment is required in this patient population and the usually recommended adult dose can be administered. 4.3 Contraindications Hypersensitivity to citicoline or any other component of the formulation 4.4 Special Warnings and Special Precautions for Use: Citicoline may cause hypotension and in case necessary the hypotensive effect can be treated with corticosteroids or sympathomimetics. 4.5 Interaction with Other Medicinal Products and Other Forms of Interaction: Citicoline must not be used with medicines containing meclophenoxates (or centrophenoxine). Citicoline increases the effects of L-dopa. 4.6 Fertility, Pregnancy and Lactation There are no adequate and well controlled studies of citicoline during pregnancy and lactation. Citicoline should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. -

Alpha-GPC Introduced 2003
Product Information Sheet – January 2015 Alpha-GPC Introduced 2003 What Is It? Are There Any Potential Drug Interactions? l-Alpha-glycerophophatidylcholine (GPC-choline, alpha-GPC) is a water- At this time, there are no known adverse reactions when taken in soluble phospholipid and neurotransmitter precursor naturally conjunction with medications. occurring in the body. Unlike most membrane phospholipids, alpha- GPC is water-soluble because it lacks the hydrophobic tail groups. Alpha-GPC Uses For Alpha-GPC each Caplique® Capsule contains v 0 • Memory And Cognitive Health: Alpha-GPC passes through the alpha-GPC (L-alpha-glycerophosphatidylcholine) ........................ 200 mg blood brain barrier providing a source of choline for acetylcholine other ingredients: glycerin, water, vegetarian Caplique® Capsule (cellulose, water) and phosphatidylcholine biosynthesis. By supporting cell membrane fluidity and integrity, phosphatidylcholine enhances Contains soy healthy neurotransmitter function and signal transduction. 6 Caplique® Capsules daily, in divided doses, with or Alpha-GPC may support healthy phospholipid turnover in the between meals. brain, helping to counteract age-related cellular breakdown of membrane phospholipids. Acetylcholine is a key neurotransmitter Caplique® Capsule is a registered trademark used by Pure Encapsulations in the brain supporting memory and learning. Optimal under license. phospholipid and acetylcholine levels support cognitive, mental Each Caplique® Capsule is preserved with a nitrogen bubble, which may give the and cerebrovascular health.* appearance of the capsule not being full. Contents may appear cloudy or thick and • Growth Hormone Support: Alpha-GPC has the ability to may settle or separate. potentiate growth hormone releasing hormone (GHRH), thereby supporting healthy growth hormone (GH) levels. The mechanism of support appears to involve increased cholinergic tone.* What Is The Source? Alpha-GPC is derived from highly purified soy lecithin. -

Biochemical Development of Surface Activity in Mammalian Lung. IV
Pediat. Res. 6: 81-99 (1972) Developmental physiology lung hyaline membrane disease phospholipids infants respiratory distress syndrome lecithin surfactant Biochemical Development of Surface Activity in Mammalian Lung. IV. Pulmonary Lecithin Synthesis in the Human Fetus and Newborn and Etiology of the Respiratory Distress Syndrome Louis GLUCK1391, MARIE V. KULOVIGH, ARTHUR I. EIDELMAN, LEANDRO CORDERO, AND AIDA F. KHAZIN Department of Pediatrics, University of California, San Diego, School of Medicine, La Jolla, California, USA Extract The surface-active complex lining alveoli in normal lung lowers surface tension on ex- piration, thus preventing alveolar collapse. Surface activity follows a developmental timetable. Infants with idiopathic respiratory distress syndrome (RDS) almost ex- clusively are prematurely born, and their lungs lack adequate surface activity and are deficient in the principal surface-active component, lecithin. This deficiency implies that RDS is a "disease of development," with fetal and neonatal timetables for lecithin synthesis. The biosynthesis of lung lecithin in the living human infant was studied by examining phospholipids in lung effluent (pharyngeal aspirates, mucus), which have identical phospholipids to those in lung lavage (alveolar wash). The fatty acid esters of isolated lecithin and phosphatidyl dimethylethanolamine (PDME) were examined. The fi-carbon fatty acids are indicators of the primary pathways of synthesis of lecithin: (1) a preponderance of palmitic acid signifying cytidine diphosphate choline (CDP-choline) + D-a,{3-diglyceride -+lecithin (choline incorporation pathway) and (2) a preponder- ance of myristic acid signifying phosphatidyl ethanolamine (PE) + 2 CH3 —»• PDME + CHZ —> lecithin (methylation pathway). Fetal lung of 18 and 20 weeks showed slight incorporation by GDP-choline pathway, absence of PDME, and almost no methylation. -

Effect of Exogenous Lecithin on Ethanol- Induced Testicular Injuries
Indian J Physiol Pharmacol 2005; 49 (3) : 297–304 EFFECT OF EXOGENOUS LECITHIN ON ETHANOL-INDUCED TESTICULAR INJURIES IN WISTAR RATS M. MANEESH*, H. JAYALEKSHMI*, SANJIBA DUTTA**, AMIT CHAKRABARTI*** AND D. M. VASUDEVAN@ Department of *Biochemistry, **Psychiatry and ***Pharmacology, Sikkim Manipal Institute of Medical Sciences, Gangtok – 737 102 and @Department of Biochemistry, Amrita Institute of Medical Sciences, Kochi – 662 026 ( Received on November 22, 2004 ) Abstract : Infertility is well-established harmful effect in chronic alcoholism and so far, there is no effective treatment for this condition. The study was conducted to determine the effects of lecithin, a known hepatoprotective on ethanol induced testicular injuries in male albino rats of Wistar strain. Five groups (n=6) of animals were used. Group I served as control. Group II received daily 1.6 g ethanol/kg body weight/day for 4 weeks orally. Group III received 1.6 g ethanol + 500 mg lecithin/kg body weight/day for four weeks orally. Group IV received 1.6 g ethanol/kg body weight for/day 4 weeks and followed by 500 mg lecithin/kg body weight/ day for four weeks orally. Group V received 1.6 g ethanol/kg body weight/ day orally for 4 weeks, followed by 4 weeks abstinence. Twenty-four hours after the last treatment the rats were sacrificed using anesthetic ether. Testes were removed and used for the estimation of extent of lipid peroxidation and tissue levels of antioxidants and steroidogenic enzymes. Lecithin protected testes from ethanol induced oxidative stress. However, the drug did not show any considerable effect on the activities of testicular ∆ 5, 3β-HSD and 17β-HSD. -

An Integrated Meta-Analysis of Peripheral Blood Metabolites and Biological Functions in Major Depressive Disorder
Molecular Psychiatry https://doi.org/10.1038/s41380-020-0645-4 ARTICLE An integrated meta-analysis of peripheral blood metabolites and biological functions in major depressive disorder 1,2,3 1,2,3 1,2,3 1,3 1,3 4,5 1,3 1,3 Juncai Pu ● Yiyun Liu ● Hanping Zhang ● Lu Tian ● Siwen Gui ● Yue Yu ● Xiang Chen ● Yue Chen ● 1,2,3 1,3 1,3 1,3 1,3 1,2,3 Lining Yang ● Yanqin Ran ● Xiaogang Zhong ● Shaohua Xu ● Xuemian Song ● Lanxiang Liu ● 1,2,3 1,3 1,2,3 Peng Zheng ● Haiyang Wang ● Peng Xie Received: 3 June 2019 / Revised: 24 December 2019 / Accepted: 10 January 2020 © The Author(s) 2020. This article is published with open access Abstract Major depressive disorder (MDD) is a serious mental illness, characterized by high morbidity, which has increased in recent decades. However, the molecular mechanisms underlying MDD remain unclear. Previous studies have identified altered metabolic profiles in peripheral tissues associated with MDD. Using curated metabolic characterization data from a large sample of MDD patients, we meta-analyzed the results of metabolites in peripheral blood. Pathway and network analyses were then performed to elucidate the biological themes within these altered metabolites. We identified 23 differentially 1234567890();,: 1234567890();,: expressed metabolites between MDD patients and controls from 46 studies. MDD patients were characterized by higher levels of asymmetric dimethylarginine, tyramine, 2-hydroxybutyric acid, phosphatidylcholine (32:1), and taurochenode- soxycholic acid and lower levels of L-acetylcarnitine, creatinine, L-asparagine, L-glutamine, linoleic acid, pyruvic acid, palmitoleic acid, L-serine, oleic acid, myo-inositol, dodecanoic acid, L-methionine, hypoxanthine, palmitic acid, L-tryptophan, kynurenic acid, taurine, and 25-hydroxyvitamin D compared with controls. -

The Relationship Between Choline Bioavailability from Diet, Intestinal Microbiota Composition, and Its Modulation of Human Diseases
nutrients Review The Relationship between Choline Bioavailability from Diet, Intestinal Microbiota Composition, and Its Modulation of Human Diseases Natalia Arias 1,2,*, Silvia Arboleya 3 , Joseph Allison 2, Aleksandra Kaliszewska 2, Sara G. Higarza 1,4 , Miguel Gueimonde 3 and Jorge L. Arias 1,4 1 Instituto de Neurociencias del Principado de Asturias (INEUROPA), 33003 Oviedo, Asturias, Spain; [email protected] (S.G.H.); [email protected] (J.L.A.) 2 Department of Basic and Clinical Neuroscience, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, Denmark Hill, London SE5 8AF, UK; [email protected] (J.A.); [email protected] (A.K.) 3 Department of Microbiology and Biochemistry of Dairy Products, Instituto de Productos Lácteos de Asturias (IPLA-CSIC), 33003 Oviedo, Asturias, Spain; [email protected] (S.A.); [email protected] (M.G.) 4 Laboratory of Neuroscience, Department of Psychology, University of Oviedo, Plaza Feijóo, s/n, 33003 Oviedo, Asturias, Spain * Correspondence: [email protected] Received: 14 July 2020; Accepted: 30 July 2020; Published: 5 August 2020 Abstract: Choline is a water-soluble nutrient essential for human life. Gut microbial metabolism of choline results in the production of trimethylamine (TMA), which, upon absorption by the host is converted into trimethylamine-N-oxide (TMAO) in the liver. A high accumulation of both components is related to cardiovascular disease, inflammatory bowel disease, non-alcoholic fatty liver disease, and chronic kidney disease. However, the relationship between the microbiota production of these components and its impact on these diseases still remains unknown. In this review, we will address which microbes contribute to TMA production in the human gut, the extent to which host factors (e.g., the genotype) and diet affect TMA production, and the colonization of these microbes and the reversal of dysbiosis as a therapy for these diseases. -

The Effects of Α-Gpc Supplementation On
THE EFFECTS OF -GPC SUPPLEMENTATION ON GROWTH HORMONE, FAT LOSS, AND BODY COMPOSITION IN OVERWEIGHT ADULTS by WILLIAM G. MALDONADO A thesis submitted to the School of Graduate Studies Rutgers, The State University of New Jersey In partial fulfillment of the requirements For the degree of Master of Science Graduate Program in Kinesiology and Applied Physiology Written under the direction of Shawn M. Arent And approved by New Brunswick, New Jersey October, 2019 ABSTRACT OF THE THESIS The Effects of -GPC Supplementation on Growth Hormone, Fat Loss, and Body Composition in Overweight Adults By WILLIAM GERARD MALDONADO Thesis Director Shawn M. Arent In the United States, there is an increasing prevalence of obesity that is associated with health risks, and, as such, the need for effective weight loss methods is becoming increasingly more important. In the elderly, α-GPC has been shown to significantly increase growth hormone (GH) concentrations, a major stimulator of lipolysis and protein synthesis. However, very little work has been done in younger individuals. PURPOSE: to investigate if α-GPC, an acetylcholine precursor, could confer additional GH or weight loss benefits to active, overweight individuals while exercise and nutrition are maintained. METHODS: Participants were randomly assigned to either α-GPC (n=15, Mage=25.8±9.1y, MBF%=35.48±1.75%) or placebo (n=13 Mage=24.4±10.4y, MBF%=35.65±1.98%) after health/fitness screening. Both groups were instructed to consume two capsules of their respective supplement for a total of 1200 mg/day, one dose before their workout or on non-workout days with their midday meal, and the second dose before going to sleep, for eight weeks. -

Effects of Long-Term Acetyl-L-Carnitine Administration in Ratsfii: Protection Against the Disrupting Effect of Stress on the Acquisition of Appetitive Behavior
Neuropsychopharmacology (2003) 28, 683–693 & 2003 Nature Publishing Group All rights reserved 0893-133X/03 $25.00 www.neuropsychopharmacology.org Effects of Long-Term Acetyl-L-Carnitine Administration in RatsFII: Protection Against the Disrupting Effect of Stress on the Acquisition of Appetitive Behavior 1 1 1 1 2 Flavio Masi , Benedetta Leggio , Giulio Nanni , Simona Scheggi , M Graziella De Montis , Alessandro 1 1 ,1 Tagliamonte , Silvia Grappi and Carla Gambarana* 1 2 Department of Neuroscience, Pharmacology Unit, University of Siena, Siena, Italy; Department of ‘Scienze del Farmaco’, University of Sassari, Sassari, Italy Long-term acetyl-L-carnitine (ALCAR) administration prevents the development of escape deficit produced by acute exposure to unavoidable stress. However, it does not revert the escape deficit sustained by chronic stress exposure. Rats exposed to chronic stress show a low dopamine (DA) output in the nucleus accumbens shell (NAcS) and do not acquire an appetitive behavior sustained by the earning of vanilla sugar (VS) made contingent on the choice of one of the two divergent arms of a Y-maze (VS-sustained appetitive behavior, VAB), while control rats consistently do. The present study shows that ALCAR treatment in rats exposed to a 7-day stress protocol prevented a decrease in DA output in the NAcS and medial prefrontal cortex (mPFC) of rats, and that it strengthened the DA response to VS consummation in the same two areas. Moreover, rats treated with long-term ALCAR or exposed to chronic stress while treated with ALCAR acquired VAB as efficiently as control rats. Moreover, VAB acquisition in stressed rats treated with ALCAR coincided with the reversal of the deficits in escape and in dopaminergic transmission in the NAcS. -

GRAS Notice 682, Lecithin from Canola
GRAS Notice (GRN) No. 682 http://www.fda.gov/Food/IngredientsPackagingLabeling/GRAS/NoticeInventory/default.htm ORIGINAL SUBMISSION •. Tox Strateg~es Innovative solutions Sound science November 22,2016 Dr. Antonia Mattia Director, Division of Biotechnology and GRAS Notice Review Office of Food Additive Safety (HFS-200) Center for Food Safety and Applied Nutrition Food and Drug Administration 51 00 Paint Branch Parkway College Park, MD 20740-3835 Subject: GRAS Notification- Canola Lecithin Dear Dr. Mattia: On behalf of Cargill, Incorporated, ToxStrategies, Inc. (its agent) is submitting, for FDA review, a copy ofthe GRAS notification as required. The enclosed document provides notice ofa claim that the food ingredient, canola lecithin, described in the enclosed notification is exempt from the premarket approval requirement of the Federal Food, Drug, and Cosmetic Act because it has been determined to be generally recognized as safe (GRAS), based on scientific procedures, for addition to food. If you have any questions or require additional information, please do not hesitate to contact me at 630-352-0303, or [email protected]. Sincerely, (b) (6) Donald F. Schmitt, M.P.H. Senior Managing Scientist ToxStrategies, Inc .. 931 W. 75th St., Suite 137, PMB 263, Naperville, IL 60565 1 Office (630) 352-0303 • www.toxstrategies.com GRAS Determination of Canola Lecitltin for Use in Food +~ OCTOBER 26, 2016 " GRAS Determination of Canola Lecithin for Use in Food SUBMITTED BY: Cargill, Incorporated 15407 McGinty Road West Wayzata, MN 55391 SUBMITTED TO: U.S. Food and Drug Administration Center for Food Safety and Applied Nutrition Office of Food Additive Safety HFS-200 5100 Paint Branch Parkway College Park MD 20740-3835 CONTACT FOR TECHNICAL OR OTHER INFORMATION Donald F. -

Potential Role of L-Carnitine in Autism Spectrum Disorder
Journal of Clinical Medicine Review Potential Role of L-Carnitine in Autism Spectrum Disorder Alina K˛epka 1,† , Agnieszka Ochoci ´nska 1,*,† , Sylwia Chojnowska 2 , Małgorzata Borzym-Kluczyk 3, Ewa Skorupa 1, Małgorzata Kna´s 2 and Napoleon Waszkiewicz 4 1 Department of Biochemistry, Radioimmunology and Experimental Medicine, The Children’s Memorial Health Institute, 04-730 Warsaw, Poland; [email protected] (A.K.); [email protected] (E.S.) 2 Faculty of Health Sciences, Lomza State University of Applied Sciences, 18-400 Lomza, Poland; [email protected] (S.C.); [email protected] (M.K.) 3 Department of Pharmaceutical Biochemistry, Medical University of Bialystok, 15-089 Bialystok, Poland; [email protected] 4 Department of Psychiatry, Medical University of Bialystok, 15-089 Bialystok, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-22-815-73-01 † These authors are sharing the first place. Both contributed equally to this work. Abstract: L-carnitine plays an important role in the functioning of the central nervous system, and especially in the mitochondrial metabolism of fatty acids. Altered carnitine metabolism, abnormal fatty acid metabolism in patients with autism spectrum disorder (ASD) has been documented. ASD is a complex heterogeneous neurodevelopmental condition that is usually diagnosed in early child- hood. Patients with ASD require careful classification as this heterogeneous clinical category may include patients with an intellectual disability or high functioning, epilepsy, language impairments, or associated Mendelian genetic conditions. L-carnitine participates in the long-chain oxidation of fatty acids in the brain, stimulates acetylcholine synthesis (donor of the acyl groups), stimulates ex- pression of growth-associated protein-43, prevents cell apoptosis and neuron damage and stimulates Citation: K˛epka,A.; Ochoci´nska,A.; neurotransmission. -

Acetylcarnitine Is a Candidate Diagnostic and Prognostic
Published OnlineFirst March 14, 2016; DOI: 10.1158/0008-5472.CAN-15-3199 Cancer Integrated Systems and Technologies Research Acetylcarnitine Is a Candidate Diagnostic and Prognostic Biomarker of Hepatocellular Carcinoma Yonghai Lu1, Ning Li2, Liang Gao3, Yong-Jiang Xu4, Chong Huang2, Kangkang Yu2, Qingxia Ling2, Qi Cheng2, Shengsen Chen2, Mengqi Zhu2, Jinling Fang1, Mingquan Chen2, and Choon Nam Ong1,3 Abstract The identification of serum biomarkers to improve the diag- carcinoma tumors and matched normal tissues. Post hoc analysis nosis and prognosis of hepatocellular carcinoma has been elusive to evaluate serum diagnosis and progression potential further to date. In this study, we took a mass spectroscopic approach to confirmed the diagnostic capability of serum acetylcarnitine. characterize metabolic features of the liver in hepatocellular Finally, an external validation in an independent batch of 58 carcinoma patients to discover more sensitive and specific serum samples (18 hepatocellular carcinoma patients, 20 liver biomarkers for diagnosis and progression. Global metabolic cirrhosis patients, and 20 healthy individuals) verified that profiling of 50 pairs of matched liver tissue samples from hepa- serum acetylcarnitine was a meaningful biomarker reflecting tocellular carcinoma patients was performed. A series of 62 hepatocellular carcinoma diagnosis and progression. These find- metabolites were found to be altered significantly in liver tumors; ings present a strong new candidate biomarker for hepatocellular however, levels of acetylcarnitine correlated most strongly with carcinoma with potentially significant diagnostic and prognostic tumor grade and could discriminate between hepatocellular capabilities. Cancer Res; 76(10); 2912–20. Ó2016 AACR. Introduction early and accurate diagnosis of hepatocellular carcinoma, there have been a number of previous investigations on gene expres- Hepatocellular carcinoma is the most common type of pri- sion, miRNA profiles, and protein expression of hepatocellular mary liver cancer and has become a major global health issue.