The Integumentary System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Development and Maintenance of Epidermal Stem Cells in Skin Adnexa
International Journal of Molecular Sciences Review Development and Maintenance of Epidermal Stem Cells in Skin Adnexa Jaroslav Mokry * and Rishikaysh Pisal Medical Faculty, Charles University, 500 03 Hradec Kralove, Czech Republic; [email protected] * Correspondence: [email protected] Received: 30 October 2020; Accepted: 18 December 2020; Published: 20 December 2020 Abstract: The skin surface is modified by numerous appendages. These structures arise from epithelial stem cells (SCs) through the induction of epidermal placodes as a result of local signalling interplay with mesenchymal cells based on the Wnt–(Dkk4)–Eda–Shh cascade. Slight modifications of the cascade, with the participation of antagonistic signalling, decide whether multipotent epidermal SCs develop in interfollicular epidermis, scales, hair/feather follicles, nails or skin glands. This review describes the roles of epidermal SCs in the development of skin adnexa and interfollicular epidermis, as well as their maintenance. Each skin structure arises from distinct pools of epidermal SCs that are harboured in specific but different niches that control SC behaviour. Such relationships explain differences in marker and gene expression patterns between particular SC subsets. The activity of well-compartmentalized epidermal SCs is orchestrated with that of other skin cells not only along the hair cycle but also in the course of skin regeneration following injury. This review highlights several membrane markers, cytoplasmic proteins and transcription factors associated with epidermal SCs. Keywords: stem cell; epidermal placode; skin adnexa; signalling; hair pigmentation; markers; keratins 1. Epidermal Stem Cells as Units of Development 1.1. Development of the Epidermis and Placode Formation The embryonic skin at very early stages of development is covered by a surface ectoderm that is a precursor to the epidermis and its multiple derivatives. -

Anatomy and Physiology of Hair
Chapter 2 Provisional chapter Anatomy and Physiology of Hair Anatomy and Physiology of Hair Bilgen Erdoğan ğ AdditionalBilgen Erdo informationan is available at the end of the chapter Additional information is available at the end of the chapter http://dx.doi.org/10.5772/67269 Abstract Hair is one of the characteristic features of mammals and has various functions such as protection against external factors; producing sebum, apocrine sweat and pheromones; impact on social and sexual interactions; thermoregulation and being a resource for stem cells. Hair is a derivative of the epidermis and consists of two distinct parts: the follicle and the hair shaft. The follicle is the essential unit for the generation of hair. The hair shaft consists of a cortex and cuticle cells, and a medulla for some types of hairs. Hair follicle has a continuous growth and rest sequence named hair cycle. The duration of growth and rest cycles is coordinated by many endocrine, vascular and neural stimuli and depends not only on localization of the hair but also on various factors, like age and nutritional habits. Distinctive anatomy and physiology of hair follicle are presented in this chapter. Extensive knowledge on anatomical and physiological aspects of hair can contribute to understand and heal different hair disorders. Keywords: hair, follicle, anatomy, physiology, shaft 1. Introduction The hair follicle is one of the characteristic features of mammals serves as a unique miniorgan (Figure 1). In humans, hair has various functions such as protection against external factors, sebum, apocrine sweat and pheromones production and thermoregulation. The hair also plays important roles for the individual’s social and sexual interaction [1, 2]. -

Hair Histology As a Tool for Forensic Identification of Some Domestic Animal Species
EXCLI Journal 2018;17:663-670 – ISSN 1611-2156 Received: June 28, 2018, accepted: July 02, 2018, published: July 06, 2018 Original article: HAIR HISTOLOGY AS A TOOL FOR FORENSIC IDENTIFICATION OF SOME DOMESTIC ANIMAL SPECIES Yasser A. Ahmed1, Safwat Ali2, Ahmed Ghallab3* 1 Department of Histology, Faculty of Veterinary Medicine, South Valley University, Qena, Egypt 2 Department of Anatomy and Embryology, Faculty of Veterinary Medicine, Minia University, Minia, Egypt 3 Department of Forensic Medicine and Toxicology, Faculty of Veterinary Medicine, South Valley University, Qena, Egypt * Corresponding author: E-mail: [email protected] http://dx.doi.org/10.17179/excli2018-1478 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/). ABSTRACT Animal hair examination at a criminal scene may provide valuable information in forensic investigations. How- ever, local reference databases for animal hair identification are rare. In the present study, we provide differential histological analysis of hair of some domestic animals in Upper Egypt. For this purpose, guard hair of large rumi- nants (buffalo, camel and cow), small ruminants (sheep and goat), equine (horse and donkey) and canine (dog and cat) were collected and comparative analysis was performed by light microscopy. Based on the hair cuticle scale pattern, type and diameter of the medulla, and the pigmentation, characteristic differential features of each animal species were identified. The cuticle scale pattern was imbricate in all tested animals except in donkey, in which coronal scales were identified. The cuticle scale margin type, shape and the distance in between were characteristic for each animal species. -

Nail Anatomy and Physiology for the Clinician 1
Nail Anatomy and Physiology for the Clinician 1 The nails have several important uses, which are as they are produced and remain stored during easily appreciable when the nails are absent or growth. they lose their function. The most evident use of It is therefore important to know how the fi ngernails is to be an ornament of the hand, but healthy nail appears and how it is formed, in we must not underestimate other important func- order to detect signs of pathology and understand tions, such as the protective value of the nail plate their pathogenesis. against trauma to the underlying distal phalanx, its counterpressure effect to the pulp important for walking and for tactile sensation, the scratch- 1.1 Nail Anatomy ing function, and the importance of fi ngernails and Physiology for manipulation of small objects. The nails can also provide information about What we call “nail” is the nail plate, the fi nal part the person’s work, habits, and health status, as of the activity of 4 epithelia that proliferate and several well-known nail features are a clue to sys- differentiate in a specifi c manner, in order to form temic diseases. Abnormal nails due to biting or and protect a healthy nail plate [1 ]. The “nail onychotillomania give clues to the person’s emo- unit” (Fig. 1.1 ) is composed by: tional/psychiatric status. Nail samples are uti- • Nail matrix: responsible for nail plate production lized for forensic and toxicology analysis, as • Nail folds: responsible for protection of the several substances are deposited in the nail plate nail matrix Proximal nail fold Nail plate Fig. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Nestin Expression in Hair Follicle Sheath Progenitor Cells
Nestin expression in hair follicle sheath progenitor cells Lingna Li*, John Mignone†, Meng Yang*, Maja Matic‡, Sheldon Penman§, Grigori Enikolopov†, and Robert M. Hoffman*¶ *AntiCancer, Inc., 7917 Ostrow Street, San Diego, CA 92111; †Cold Spring Harbor Laboratory, 1 Bungtown Road, Cold Spring Harbor, NY 11724; §Department of Biology, Massachusetts Institute of Technology, 77 Massachusetts Avenue, Cambridge, MA 02139-4307; and ‡Stony Brook University, Stony Brook, NY 11794 Contributed by Sheldon Penman, June 25, 2003 The intermediate filament protein, nestin, marks progenitor expression of the neural stem cell protein nestin in hair follicle cells of the CNS. Such CNS stem cells are selectively labeled by stem cells suggests a possible relation. placing GFP under the control of the nestin regulatory se- quences. During early anagen or growth phase of the hair Materials and Methods follicle, nestin-expressing cells, marked by GFP fluorescence in Nestin-GFP Transgenic Mice. Nestin is an intermediate filament nestin-GFP transgenic mice, appear in the permanent upper hair (IF) gene that is a marker for CNS progenitor cells and follicle immediately below the sebaceous glands in the follicle neuroepithelial stem cells (5). Enhanced GFP (EGFP) trans- bulge. This is where stem cells for the hair follicle outer-root genic mice carrying EGFP under the control of the nestin sheath are thought to be located. The relatively small, oval- second-intron enhancer are used for studying and visualizing shaped, nestin-expressing cells in the bulge area surround the the self-renewal and multipotency of CNS stem cells (5–7). hair shaft and are interconnected by short dendrites. The precise Here we report that hair follicle stem cells strongly express locations of the nestin-expressing cells in the hair follicle vary nestin as evidenced by nestin-regulated EGFP expression. -

CHAPTER 4 the Integumentary System
CHAPTER 4 The Integumentary System LEARNING OBJECTIVES Upon completion of this chapter, you should be able to: • Name the two layers of the skin. • Name the accessory structures of the integumentary system. • Build and pronounce medical terms of the integumentary system. • Name the disorders and treatments relating to the integumentary system. • Name the major classifi cations of pharmacologic agents used to treat skin disorders. • Analyze and defi ne the new terms introduced in this chapter. • Interpret abbreviations associated with the integumentary system. 53 54 PART TWO • BODY SYSTEMS Introduction The largest organ of the body is the skin. The skin covers the entire body—more than 20 square feet on average—and weighs about 24 pounds. It is part of the integumentary system, which also includes the accessory structures: hair, nails, and sebaceous (oil) and sudoriferous (sweat) glands. Integumentum is Latin for “covering” or “shelter.” The physician who specializes in the diag- nosis and treatment of skin disorders is called a dermatologist (dermat/o being one of the com- bining forms for skin). Coupling the root dermat/o with the previously learned suffi x -logy gives us the term dermatology , which is the term for the specialty practice that deals with the skin. Word Elements The major word elements that relate to the integumentary system consist of various anatomical components, accessory structures, colors of the skin, and abnormal conditions. The Word Ele- ments table lists many of the roots, their meanings, and examples associated -

Identification of Hair Shaft Progenitors That Create a Niche for Hair Pigmentation
Downloaded from genesdev.cshlp.org on September 27, 2021 - Published by Cold Spring Harbor Laboratory Press Identification of hair shaft progenitors that create a niche for hair pigmentation Chung-Ping Liao,1 Reid C. Booker,1 Sean J. Morrison,2,3,4,5,6 and Lu Q. Le1,4,5 1Department of Dermatology, 2Department of Pediatrics, 3Children’s Research Institute, 4Simmons Comprehensive Cancer Center, 5Hamon Center for Regenerative Science and Medicine, 6Howard Hughes Medical Institute, University of Texas Southwestern Medical Center, Dallas, Texas 75390, USA Hair differentiates from follicle stem cells through progenitor cells in the matrix. In contrast to stem cells in the bulge, the identities of the progenitors and the mechanisms by which they regulate hair shaft components are poorly understood. Hair is also pigmented by melanocytes in the follicle. However, the niche that regulates follicular melanocytes is not well characterized. Here, we report the identification of hair shaft progenitors in the matrix that are differentiated from follicular epithelial cells expressing transcription factor KROX20. Depletion of Krox20 lin- eage cells results in arrest of hair growth, confirming the critical role of KROX20+ cells as antecedents of structural cells found in hair. Expression of stem cell factor (SCF) by these cells is necessary for the maintenance of differen- tiated melanocytes and for hair pigmentation. Our findings reveal the identities of hair matrix progenitors that regulate hair growth and pigmentation, partly by creating an SCF-dependent niche for follicular melanocytes. [Keywords: stem cell factor (SCF); hair pigmentation; hair shaft progenitor cell; hair follicle stem cell; hair matrix; KROX20] Supplemental material is available for this article. -

Neural Control of Facial Sweat Gland Secretion in Horses
Iowa State University Capstones, Theses and Creative Components Dissertations Fall 2019 Neural control of facial sweat gland secretion in horses Lu Liu Follow this and additional works at: https://lib.dr.iastate.edu/creativecomponents Part of the Comparative and Evolutionary Physiology Commons, and the Systems and Integrative Physiology Commons Recommended Citation Liu, Lu, "Neural control of facial sweat gland secretion in horses" (2019). Creative Components. 455. https://lib.dr.iastate.edu/creativecomponents/455 This Creative Component is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Creative Components by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Neural control of facial sweat gland secretion in horses Lu Liu 2019.11.26 BMS 599 Creative Component Biomedical Sciences Department Iowa State University Abstract: For sweat glands, it has been shown that sympathetic neurons express a cholinergic/noradrenergic co-phenotype in their innervation in the trunk of mice.(Schütz et al. 2008). It is unknown if facial sweat glands are innervated the same way. Gustatory sweating is an abnormal sweating condition. People can sweat profusely when eating or drinking, or even thinking about eating or drinking. We hypothesize that the facial sweat glands are controlled differently and can be related to parasympathetic neurons from cranial nerves. Some samples from human donors have been tested, but few sweat glands can be targeted since the donors were older people. Thus, it was decided to use horse tissue for this project to obtain greater numbers of sweat glands on the face. -

Ch7 Basic Body Structure and Function Test&A
Chapter 7- Test Name: Basic Body Structure & Fuction Date: 1. Physiology is the study of A) what body parts look like and where they are located. B) the structure and function of the human body. C) how the various body parts work. D) how organisms are created. 2. The basic unit of life is A) a cell. B) a tissue. C) an organ. D) an organ system. 3. Which one of the following is like the cell's brain? A) The cytoplasm B) The cell nucleus C) The cell organelles D) The cell membrane 4. Which cell transports oxygen throughout the body? A) Red blood B) Epithelial C) Muscle D) Nerve 5. Which one of the following is considered connective tissue? A) Mucous membrane B) Blood C) Skin D) Glands 6. Which one of the following organs is included in the integumentary system? A) The fingernails B) The gallbladder C) The pancreas D) The ureters 7. What does epithelial tissue do? A) It connects tissues together. B) It produces movement. C) It conducts information. D) It protects the body. Page 1 8. Which statement correctly describes homeostasis? A) It causes problems by invading otherwise healthy tissues. B) It reduces the immune system's ability to fight off infection. C) It is a state of balance achieved by all of the organ systems working together. D) It occurs when the structure or function of an organ or organ system is abnormal. 9. The purpose of melanin is to A) keep the skin lubricated. B) aid in temperature regulation. C) give our skin, hair, and eyes color. -
The Integumentary System
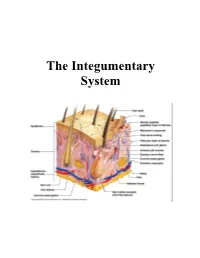
CHAPTER 5: THE INTEGUMENTARY SYSTEM Copyright © 2010 Pearson Education, Inc. OVERALL SKIN STRUCTURE 3 LAYERS Copyright © 2010 Pearson Education, Inc. Figure 5.1 Skin structure. Hair shaft Dermal papillae Epidermis Subpapillary vascular plexus Papillary layer Pore Appendages of skin Dermis Reticular • Eccrine sweat layer gland • Arrector pili muscle Hypodermis • Sebaceous (oil) gland (superficial fascia) • Hair follicle Nervous structures • Hair root • Sensory nerve fiber Cutaneous vascular • Pacinian corpuscle plexus • Hair follicle receptor Adipose tissue (root hair plexus) Copyright © 2010 Pearson Education, Inc. EPIDERMIS 4 (or 5) LAYERS Copyright © 2010 Pearson Education, Inc. Figure 5.2 The main structural features of the skin epidermis. Keratinocytes Stratum corneum Stratum granulosum Epidermal Stratum spinosum dendritic cell Tactile (Merkel) Stratum basale Dermis cell Sensory nerve ending (a) Dermis Desmosomes Melanocyte (b) Melanin granule Copyright © 2010 Pearson Education, Inc. DERMIS 2 LAYERS Copyright © 2010 Pearson Education, Inc. Figure 5.3 The two regions of the dermis. Dermis (b) Papillary layer of dermis, SEM (22,700x) (a) Light micrograph of thick skin identifying the extent of the dermis, (50x) (c) Reticular layer of dermis, SEM (38,500x) Copyright © 2010 Pearson Education, Inc. Figure 5.3a The two regions of the dermis. Dermis (a) Light micrograph of thick skin identifying the extent of the dermis, (50x) Copyright © 2010 Pearson Education, Inc. Q1: The type of gland which secretes its products onto a surface is an _______ gland. 1) Endocrine 2) Exocrine 3) Merocrine 4) Holocrine Copyright © 2010 Pearson Education, Inc. Q2: The embryonic tissue which gives rise to muscle and most connective tissue is… 1) Ectoderm 2) Endoderm 3) Mesoderm Copyright © 2010 Pearson Education, Inc. -
The Integumentary System
The Integumentary System THE INTEGUMENTARY SYSTEM Skin is the system of the body that makes an individual beautiful! Skin/fur coloration allows animals to be camouflaged. *The skin is the largest organ of the body. The skin and its derivatives (hair, nails, sweat and oil glands) make up the integumentary system. The total surface area of the skin is about 1.8 m² and its total weight is about 11 kg. The skin gives us our appearance and shape. Anatomy of the Skin • Skin is made up of two layers that cover a third fatty layer. The outer layer is called the epidermis; it is a tough protective layer. The second layer (located under the epidermis) is called the dermis; it contains nerve endings, sweat glands, oil glands, and hair follicles. Under these two skin layers is a fatty layer called the subcutaneous tissue, or hypodermis. 1 • The dermis is home to the oil glands. These are also called sebaceous glands, and they are always producing sebum. Sebum is your skin's own natural oil. It rises to the surface of your epidermis to keep your skin lubricated and protected. It also makes your skin waterproof. • Skin is alive! It's made of many thin sheets of flat, stacked cells. Older cells are constantly being pushed to the surface by new cells, which grow from below. When the old ones reach the top, they become wider and flatter as they get rubbed and worn by all your activity. And, sooner or later, they end up popping off like tiles blown from a roof in a strong wind.