Nail Anatomy and Physiology for the Clinician 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Development and Maintenance of Epidermal Stem Cells in Skin Adnexa
International Journal of Molecular Sciences Review Development and Maintenance of Epidermal Stem Cells in Skin Adnexa Jaroslav Mokry * and Rishikaysh Pisal Medical Faculty, Charles University, 500 03 Hradec Kralove, Czech Republic; [email protected] * Correspondence: [email protected] Received: 30 October 2020; Accepted: 18 December 2020; Published: 20 December 2020 Abstract: The skin surface is modified by numerous appendages. These structures arise from epithelial stem cells (SCs) through the induction of epidermal placodes as a result of local signalling interplay with mesenchymal cells based on the Wnt–(Dkk4)–Eda–Shh cascade. Slight modifications of the cascade, with the participation of antagonistic signalling, decide whether multipotent epidermal SCs develop in interfollicular epidermis, scales, hair/feather follicles, nails or skin glands. This review describes the roles of epidermal SCs in the development of skin adnexa and interfollicular epidermis, as well as their maintenance. Each skin structure arises from distinct pools of epidermal SCs that are harboured in specific but different niches that control SC behaviour. Such relationships explain differences in marker and gene expression patterns between particular SC subsets. The activity of well-compartmentalized epidermal SCs is orchestrated with that of other skin cells not only along the hair cycle but also in the course of skin regeneration following injury. This review highlights several membrane markers, cytoplasmic proteins and transcription factors associated with epidermal SCs. Keywords: stem cell; epidermal placode; skin adnexa; signalling; hair pigmentation; markers; keratins 1. Epidermal Stem Cells as Units of Development 1.1. Development of the Epidermis and Placode Formation The embryonic skin at very early stages of development is covered by a surface ectoderm that is a precursor to the epidermis and its multiple derivatives. -

Tbwhat You Need to Know About the Tuberculosis Skin Test
What You Need to Know About TB the Tuberculosis Skin Test “I was told I needed a TB skin test, so I went to the health clinic. It was quick and didn’t hurt. In two days, I went back to the clinic so the nurse could see the results. It’s important to go back in 2 or 3 days to get your results or you will have to get the test again.” A TB skin test will tell you if you have ever had TB germs in your body. • A harmless fluid is placed under your skin on the inside of your arm. A very small needle is used, so you will only feel a light pinch. • Make sure you don’t put a bandage or lotion on the test spot. Also—don’t scratch the spot. If the area itches, put an ice cube or cold cloth on it. It is okay for the test spot to get wet, but do not wipe or scrub the area. • Return to the clinic or doctor’s office in 2 to 3 days so your healthcare provider can look at the test spot on your arm. He or she will look at the test spot and measure any bump that appears there. Your healthcare provider will let you know if your test is negative or positive. Write the time and date you will need to return here: 2 Remember—only a healthcare provider can read your TB skin test results the right way. When your skin test is positive: • You have TB germs in your body. -

Touch and Temperature Senses
1 In press in Proceedings of the Association for Biology Laboratory Education (ABLE), 2004 Touch and Temperature Senses by Charlie Drewes Ecology, Evolution & Organismal Biology Iowa State University Ames, IA 50011 (515) 294-8061 [email protected] http://www.eeob.iastate.edu/faculty/DrewesC/htdocs/ Biographical: Charlie Drewes received a BA in biology from Augustana College (SD) and his MS and PhD in zoology from Michigan State University. Currently, he is a professor in Ecology, Evolution and Organismal Biology at Iowa State University. His research focus is on rapid escape reflexes and locomotion, especially in oligochaete worms. Charlie teaches courses in invertebrate biology, neurobiology and bioethics. During summers, he leads hands-on, residential workshops for high school biology teachers at Iowa Lakeside Lab. In 1998, he received the Distinguished Science Teaching Award from the Iowa Academy of Science and, in 2002, he received the Four-year College Biology Teaching Award from the National Association of Biology Teachers. Abstract: This investigation focuses on the sensory biology of human touch and temperature reception. Students investigate quantitative and qualitative aspects of touch-sensory functions in human skin. Values for two-point discrimination are compared to Weber’s original data. Also, novel materials and methods are introduced for investigating the functional organization of cold sensory reception in human skin, including: (a) estimation of sensory field size for single cold-sensory fibers, (b) demonstration of the discontinuous distribution of cold-sensory fibers in skin, and (c) estimation of the density of cold-sensitive fibers per unit area of skin. Tactile and thermoreceptor functions are related to underlying neuroanatomy of peripheral and central neural pathways. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

CHAPTER 4 the Integumentary System
CHAPTER 4 The Integumentary System LEARNING OBJECTIVES Upon completion of this chapter, you should be able to: • Name the two layers of the skin. • Name the accessory structures of the integumentary system. • Build and pronounce medical terms of the integumentary system. • Name the disorders and treatments relating to the integumentary system. • Name the major classifi cations of pharmacologic agents used to treat skin disorders. • Analyze and defi ne the new terms introduced in this chapter. • Interpret abbreviations associated with the integumentary system. 53 54 PART TWO • BODY SYSTEMS Introduction The largest organ of the body is the skin. The skin covers the entire body—more than 20 square feet on average—and weighs about 24 pounds. It is part of the integumentary system, which also includes the accessory structures: hair, nails, and sebaceous (oil) and sudoriferous (sweat) glands. Integumentum is Latin for “covering” or “shelter.” The physician who specializes in the diag- nosis and treatment of skin disorders is called a dermatologist (dermat/o being one of the com- bining forms for skin). Coupling the root dermat/o with the previously learned suffi x -logy gives us the term dermatology , which is the term for the specialty practice that deals with the skin. Word Elements The major word elements that relate to the integumentary system consist of various anatomical components, accessory structures, colors of the skin, and abnormal conditions. The Word Ele- ments table lists many of the roots, their meanings, and examples associated -

Pedicure: Nail Enhancements
All Hair Services Include Shampoo All Services Based on Student Availability Long Hair is Extra & Senior Price Available Hair Cuts: Color: (Does Not Include Cut & Style) Hair Cut (Hood dryer) $6.50 Retouch/Tint/PM Shine $14.50 With Blowdry $13.50 Additional Application $8.00 With Blowdry & Flat Iron $21.50 Color (All over color) $20.00 Foils Each $4.00 Hair Styles: Hair Length to Collar $38.00 Shampoo/Set $6.75 Hair Length to Shoulder $48.00 Spiral Rod Set $20.00 Hair Length past Shoulder $58.00 Shampoo/ Blowdry $9.00 Frosting with Cap $17.50 With Thermal Iron $13.00 Men’s Comb Highlight with Cut $15.00 With Flat Iron $15.00 With Press & Curl $18.00 Perms & Relaxers: (Includes Cut & Style) Wrap Only $6.50 Regular or Normal Hair $20.95 Wrap with Roller Set $10.50 Resistant or Tinted Hair $26.00 Fingerwaves with Style $17.50 Spiral or Piggyback $36.00 Twists $3.00 Relaxer $35.00 Straight Back $20.00 Curled $15.00 Other Hair Services: Spiral $20.00 Shampoo Only $2.00 French Braids with Blowdry $15.00 Line-up $3.00 Under 10 Braids $20.00 Deep Condition $5.00 Over 10 Braids $25.00 Keratin Treatment $15.00 Braid Removal $15.00 Updo or French Roll $20.00 Manicure: Spa Manicure $9.50 Waxing: French Manicure $8.00 Brow $6.00 Manicure $6.42 Lip $5.00 Chin $5.00 Pedicure: Full Face $15.00 Spa Pedicure $20.00 Half Leg $15.00 French Pedicure $17.00 Full Leg $30.00 Pedicure $15.00 Underarm $15.00 Half Arm $10.00 Nail Enhancements: Full Arm $15.00 Shellac (French $2) $15.00 Mid Back & Up $15.00 Overlay (Natural Nail) $12.00 Full Back $25.00 Acrylic Full Set $16.50 Bikini $25.00 Gel Full Set $18.00 Fill-in Gel & Acrylic $12.00 Massages: Nail Repair( Per Nail) $2.00 Relaxation $15.00 Soak Off $3.00 Deep Tissue $19.95 Nail Art (Per Nail) $1.00 Other Nail Services: Nails & Waxing Services Taxable Polish Change $4.00 Nails Clipped $5.00 Paraffin Dip Wax $5.00 . -
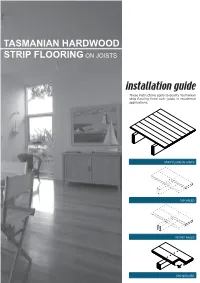
Tasmanian Hardwood Strip Flooring on Joists Guide for Installing
TASMANIAN HARDWOOD STRIP FLOORING ON JOISTS installation guide These instructions apply to quality Tasmanian strip flooring fixed over joists in residential applications. STRIP FLOOR ON JOISTS TOP NAILED SECRET NAILED END MATCHED TOOLS Simple tools are adequate in most applications. Necessary tools are: Tool Requirement Checklist Pencil, tape measure and square Hammer, punch and nail bag Stringline, spirit level and straight edge Hand saw and jig saw Safety glasses, dust mask and knee pads Spacers (about 100mm long and 2 mm thick) Rubber mallet, broom and vacuum cleaner Framing chisel For specialist applications, a drop saw, an air power staple gun, a power actuated fastener system and a cramping system may be useful. MATERIALS Use quality boards of the correct thickness. Grade descriptions for strip flooring are set out in the Australian Standard AS 2796 and are available at: www.tastimber.tas.gov.au. Boards at least 19 mm thick are needed to span 450 mm. Board width - Only secret nail boards up to 85 mm cover width. Secret nailed flooring is fixed through the tongue of specially profiled boards. Since they are only secured with one fastener per joist or batten, their width is limited to 85 mm cover. Board over 85 cover must be top nailed with two fasteners per joist. Use the correct nails for the job. The nail sizes required by Australian Standard 1684 are: Nail sizes for T & G flooring to joists* Nail sizes for T & G flooring to plywood substrate* Nailing Softwood Hardware & Strip flooring Rec. nailing (min.15mm substrate) joists cypress joists thicknes (mm) Hand 65 x 2.8 mm 50 x 2.8 mm 38 x 16 guage chisel point staples or driven bullet head bullet head 19 or 20 38 x 2.2 mm nails at 300mm spacing 32 x 16 guage chisel point staples or Machine 12,19 or 20 driven 65 x 2.5 mm 50 x 2.5 mm 30 x 2.2 mm nails at 200mm spacing *Alternative fasteners can be used for substrates types not listed subject to manufacturers’ recommendation. -

Regional Handwashing Policy
SOUTHERN CALIFORNIA GRADUATE MEDICAL EDUCATION POLICY AND PROCEDURE POLICY INFECTION PREVENTION AND CONTROL POLICIES EFFECTIVE DATE: SECTION: AND PROCEDURES 7/1/2014 TITLE: Hand Health & Hygiene Page: 1 of 8 BACKGROUND Studies have shown that handwashing causes a reduction in the carriage of potential pathogens on the hands. Microorganisms proliferate on the hands within the moist environment of gloves. Handwashing results in the reduction of patient morbidity and mortality from health care associated infections. The Centers for Disease Control and Prevention states that handwashing is the single most important procedure for preventing health-care associated infections. Artificial nails are more likely than natural nails to harbor pathogens that can lead to health care associated infections. There are four types of hand washing (see body of policy for detailed instructions): TYPE PURPOSE METHOD Routine Handwashing To remove soil and transient Wash hands with soap and microorganisms. water for at least 15 seconds. Hand antisepsis To remove soil and remove or Wash hands with antimicrobial destroy transient soap and water for at least 15 microorganisms. seconds. Hand rub/degerming To destroy transient and Rub alcohol-based hand resident microorganisms on degermer into hands vigorously UNSOILED hands. until dry. Surgical hand scrub To remove or destroy transient Wash hands and forearms with microorganisms and reduce antimicrobial soap and water resident flora. with brush to achieve friction. Or alcohol-based preparation rubbed vigorously -
The Integumentary System
CHAPTER 5: THE INTEGUMENTARY SYSTEM Copyright © 2010 Pearson Education, Inc. OVERALL SKIN STRUCTURE 3 LAYERS Copyright © 2010 Pearson Education, Inc. Figure 5.1 Skin structure. Hair shaft Dermal papillae Epidermis Subpapillary vascular plexus Papillary layer Pore Appendages of skin Dermis Reticular • Eccrine sweat layer gland • Arrector pili muscle Hypodermis • Sebaceous (oil) gland (superficial fascia) • Hair follicle Nervous structures • Hair root • Sensory nerve fiber Cutaneous vascular • Pacinian corpuscle plexus • Hair follicle receptor Adipose tissue (root hair plexus) Copyright © 2010 Pearson Education, Inc. EPIDERMIS 4 (or 5) LAYERS Copyright © 2010 Pearson Education, Inc. Figure 5.2 The main structural features of the skin epidermis. Keratinocytes Stratum corneum Stratum granulosum Epidermal Stratum spinosum dendritic cell Tactile (Merkel) Stratum basale Dermis cell Sensory nerve ending (a) Dermis Desmosomes Melanocyte (b) Melanin granule Copyright © 2010 Pearson Education, Inc. DERMIS 2 LAYERS Copyright © 2010 Pearson Education, Inc. Figure 5.3 The two regions of the dermis. Dermis (b) Papillary layer of dermis, SEM (22,700x) (a) Light micrograph of thick skin identifying the extent of the dermis, (50x) (c) Reticular layer of dermis, SEM (38,500x) Copyright © 2010 Pearson Education, Inc. Figure 5.3a The two regions of the dermis. Dermis (a) Light micrograph of thick skin identifying the extent of the dermis, (50x) Copyright © 2010 Pearson Education, Inc. Q1: The type of gland which secretes its products onto a surface is an _______ gland. 1) Endocrine 2) Exocrine 3) Merocrine 4) Holocrine Copyright © 2010 Pearson Education, Inc. Q2: The embryonic tissue which gives rise to muscle and most connective tissue is… 1) Ectoderm 2) Endoderm 3) Mesoderm Copyright © 2010 Pearson Education, Inc. -

Sweat Glands • Oil Glands • Mammary Glands
Chapter 4 The Integumentary System Lecture Presentation by Steven Bassett Southeast Community College © 2015 Pearson Education, Inc. Introduction • The integumentary system is composed of: • Skin • Hair • Nails • Sweat glands • Oil glands • Mammary glands © 2015 Pearson Education, Inc. Introduction • The skin is the most visible organ of the body • Clinicians can tell a lot about the overall health of the body by examining the skin • Skin helps protect from the environment • Skin helps to regulate body temperature © 2015 Pearson Education, Inc. Integumentary Structure and Function • Cutaneous Membrane • Epidermis • Dermis • Accessory Structures • Hair follicles • Exocrine glands • Nails © 2015 Pearson Education, Inc. Figure 4.1 Functional Organization of the Integumentary System Integumentary System FUNCTIONS • Physical protection from • Synthesis and storage • Coordination of immune • Sensory information • Excretion environmental hazards of lipid reserves response to pathogens • Synthesis of vitamin D3 • Thermoregulation and cancers in skin Cutaneous Membrane Accessory Structures Epidermis Dermis Hair Follicles Exocrine Glands Nails • Protects dermis from Papillary Layer Reticular Layer • Produce hairs that • Assist in • Protect and trauma, chemicals protect skull thermoregulation support tips • Nourishes and • Restricts spread of • Controls skin permeability, • Produce hairs that • Excrete wastes of fingers and supports pathogens prevents water loss provide delicate • Lubricate toes epidermis penetrating epidermis • Prevents entry of -
Nails Develop from Thickened Areas of Epidermis at the Tips of Each Digit Called Nail Fields
Nail Biology: The Nail Apparatus Nail plate Proximal nail fold Nail matrix Nail bed Hyponychium Nail Biology: The Nail Apparatus Lies immediately above the periosteum of the distal phalanx The shape of the distal phalanx determines the shape and transverse curvature of the nail The intimate anatomic relationship between nail and bone accounts for the bone alterations in nail disorders and vice versa Nail Apparatus: Embryology Nail field develops during week 9 from the epidermis of the dorsal tip of the digit Proximal border of the nail field extends downward and proximally into the dermis to create the nail matrix primordium By week 15, the nail matrix is fully developed and starts to produce the nail plate Nails develop from thickened areas of epidermis at the tips of each digit called nail fields. Later these nail fields migrate onto the dorsal surface surrounded laterally and proximally by folds of epidermis called nail folds. Nail Func7on Protect the distal phalanx Enhance tactile discrimination Enhance ability to grasp small objects Scratching and grooming Natural weapon Aesthetic enhancement Pedal biomechanics The Nail Plate Fully keratinized structure produced throughout life Results from maturation and keratinization of the nail matrix epithelium Attachments: Lateral: lateral nail folds Proximal: proximal nail fold (covers 1/3 of the plate) Inferior: nail bed Distal: separates from underlying tissue at the hyponychium The Nail Plate Rectangular and curved in 2 axes Transverse and horizontal Smooth, although -

There Are 25 Questions, Each Worth 3 Points and a Short Essay Worth 25 Points. DO YOUR OWN WORK !! Use Your Time Wisely 1. T
Mr. Holder Integumentary System – Unit 5 December 3, 2015 ARC TEST 1.0 DO NOT MARK OR WRITE ON THIS QUIZ !! There are 25 questions, each worth 3 points and a short essay worth 25 points. DO YOUR OWN WORK !! Use Your Time Wisely 1. The Integumentary System is divided into how many layers? a) 2 b) 3 c) 4 d) 6 2. What are the two major groups of membranes covering the human body? a) Epithelial & Mucus b) Cutaneous & Mucus c) Epithelial & Connective Tissue d) None of these 3. Which internal membrane provides protection for your joints? a) Serous b) Synovial c) Cutaneous d) Mucus 4. These membranes line internal cavities exposed to air & excrete a gooey substance. a) Serous b) Synovial c) Cutaneous d) Mucus 5. The Integumentary System protects the human body from … a) Friction b) Hot & Cold Temperature c) Bacteria d) All of These 6. Which stratum of the epidermis is full of keratin, cornified to prevent water loss? a) Basale b) Granulosum c) Corneum d) None of These 7. Which body system extends into the dermis to provide information to your brain? a) Cardiovascular b) Immune c) Integumentary d) Nervous 8. Subcutaneous tissue includes adipose tissue or fat. It is also known as the … a) Dermis b) Papillary Layer c) Hypodermis d) Reticular Layer 9. The dermis is divided into two layers. Which of these is the thickest? a) Papillary b) Reticular c) Basale d) Hypodermis 10. Which stratum of the epidermis is responsible for new cell production? a) Corneum b) Basale c) Granulosum d) Spinosum Page 1 Mr.