For Peer Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Televisionization: Enactments of TV Experiences in Novels from 1970 to 2010 Claudia Weber
Claudia Weber Claudia Televisionization Enactments of TV Experiences in Novels from 1970 to 2010 Claudia Weber Televisionization Claudia Weber pursued her doctoral studies both at Stock- holm University, Sweden and Justus-Liebig-Universität Giessen, Germany. She is now employed at Technische Universität Darmstadt, Germany where she works in higher education didactics. ISBN 978-91-7447-979-9 Department of English Doctoral Thesis in English at Stockholm University, Sweden 2014 Televisionization: Enactments of TV Experiences in Novels from 1970 to 2010 Claudia Weber Televisionization Enactments of TV Experiences in Novels from 1970 to 2010 Claudia Weber © Claudia Weber, Stockholm University 2014 ISBN 978-91-7447-979-9 Printed in Sweden by Stockholm University Press, Stockholm 2014 Distributor: Department of English Abstract TV’s conquest of the American household in the period from the 1940s to the 1960s went hand in hand with critical discussions that revolved around the disastrous impact of television consumption on the viewer. To this day, watching television is connected with anxieties about the trivialization and banalization of society. At the same time, however, people appreciate it both as a source of information and entertainment. Television is therefore ‘both…and:’ entertainment and anxiety; distraction and allurement; compan- ionship and intrusion. When the role and position of television in culture is ambiguous, personal relations with, attitudes towards, and experiences of television are equally ambivalent, sometimes even contradictory, but the public and academic discourses on television tend to be partial. They focus on the negative impact of television consumption on the viewer, thereby neglecting whatever positive experiences one might associate with it. -

“La Lucha Libre Mexicana. Su Función Compensatoria En Relación Al Trauma Cultural”
Traducción del artículo “Mexican Wrestling. Its Compensatory Function in Relation to Cultural Trauma”, del Jung Journal: Culture & Psyche, vol. 4, núm. 4. Con la autorización de UCPress para reproducirse en una página web institucional. “La lucha libre mexicana. Su función compensatoria en relación al trauma cultural” VÍCTOR MANUEL LÓPEZ G. La lucha libre mexicana se deriva del catch-as-catch-can francés de los años 30, que combina la lucha grecorromana con el wrestling estadounidense. Originalmente relacionado con el pancracio1, esta forma de lucha ha trascendido fronteras. La lucha libre ha dado el salto de los cuadriláteros a las páginas de las revistas deportivas, la televisión, el cine y las fotonovelas, consagrando un subgénero cuyos protagonistas se han convertido en héroes icónicos, tal como lo demuestra el siguiente extracto tomado de una narración, transmitida por televisión mexicana en septiembre de 2008. Anunciador: la pelea será a dos de tres caídas sin límite de tiempo. En la esquina de los técnicos tenemos al Dr. Planeta, y en la de los rudos, al Sr. Calavera. ¡Y comienza la pelea! Calavera lanza una patada voladora a su oponente, quien se retuerce de dolor. Calavera inmoviliza a su rival contra el suelo y le mete el dedo en el ojo. Esta es una estratagema ilegal. Público: ¡Auch! ¡Tramposo! ¡Castíguenlo! ¡Llamen a la policía! (Chiflidos e insultos dirigidos al Sr. Calavera.) Anunciador: Planeta huye de la golpiza. Se para y corre hacia las cuerdas. Calavera lo persigue y lanza otro golpe ilegal contra Planeta, que lo evade. Frustra a Calavera usando un candado de cangrejo. -

'The Assault on Mount B' by Rod Fee 1/129
‘The Assault on Mount B’ by Rod Fee 1/129 Rod Fee ID:0826790 ‘The Assault on Mount B: understanding the role of story in self-delusion in our personal histories.’ A thesis submitted to Auckland University of Technology in fulfilment of the requirements for the degree of Doctor of Philosophy (PhD) 2015 Faculty: Applied Humanities School: Languages and Social Sciences Primary Supervisor: Dr Paul Mountfort Secondary Supervisor: Dr Maria O’Connor ‘The Assault on Mount B’ by Rod Fee 2/129 ATTESTATION OF AUTHORSHIP I hereby declare that this submission is my own work and that, to the best of my knowledge and belief, it contains no material previously published or written by another person (except where explicitly defined in the acknowledgements), nor material which to a substantial extent has been submitted for the award of any other degree or diploma of a university or other institution of higher learning. R H Fee ‘The Assault on Mount B’ by Rod Fee 3/129 ACKNOWLEDGEMENTS I acknowledge the assistance of: 1. My two supervisors Dr Paul Mountfort and Dr Maria O’Connor, and Associate Professor Mark Jackson mentor supervisor, all of AUT University ‘The Assault on Mount B’ by Rod Fee 4/129 INTELLECTUAL PROPERTY RIGHTS 1. All intellectual property including copyright, is retained by the candidate in the content of the candidate’s thesis. For the removal of doubt, publication by the candidate of this or any derivative work does not change the intellectual property rights of the candidate in relation to the thesis. 2. I confirm that my thesis does not contain plagiarised material or material for which the copyright or other intellectual property belongs to a third party. -

Arena Puebla
Octubre 2020 Spanish Reader ARENA PUEBLA Arena Puebla lugar de diversión y tradición. Septiembre es uno de los meses más importantes para los mexicanos, no solo por las fiestas patrias sino también por el “Día Nacional de la Lucha Libre y del Luchador Profesional Mexicano'' que se celebra cada 21 de septiembre. Por esa razón es necesario hablar de la emblemática Arena Puebla, el lugar sagrado para los luchadores, el lugar en donde se desarrollan espectáculos tan emocionantes para los mexicanos. La Arena Puebla se fundó el 18 de julio de 1953, está ubicada en la 13 oriente 402 en el popular barrio El Carmen y tiene un espacio para 3000 aficionados. Fue inaugurada por Salvador Lutteroth González conocido como el padre de la lucha libre mexicana y quien fue el fundador del Consejo Mundial de la Lucha Libre (CMLL). Además, este espacio funciona como escuela de lucha libre, con más de 20 años de experiencia. Este año celebró 67 años de su creación, pero debido a la pandemia los festejos tuvieron que ser postergados. 01 Spanish Institute of Puebla www.sipuebla.com Octubre 2020 En su inauguración, la lucha estelar tuvo a grandes figuras como Black Shadow, Tarzán López, y Enrique Yañez, enfrentando al Verdugo, el Cavernario Galindo y el famosísimo Santo “El Enmascarado de Plata”, quien en aquel momento era el campeón mundial Welter. Diferentes luchadores han engalanado las noches en el cuadrilátero, entre ellos están Blue Demon, El Huracán Ramírez, Arturo Casco “La Fiera”, El Perro Aguayo, Semi- narista, Califa, Danger, El Hércules Poblano, Gorila Osorio, Petronio Limón, El Jabato, Manuel Robles, Furia Chicana, Gardenia Davis, El Faraón, Enrique Vera, Príncipe Rojo, Tarahumara, Chico Madrid, Gavilán, Sombra Poblana, Murciélago, El Santo Poblano, El Perro Aguayo Jr. -

Learning from Delusions
OPINION Brian Martin nce or twice a year, I receive a call or Learning email from some- O one claiming to be under intensive tar- geted surveillance by the govern- from Delusions ment. They contact me because there’s a lot of material on my website about whistleblowing, and some about surveillance. I know governments carry out massive sur- veillance operations, for example collecting all sorts of electronic With others, the delusion is more ers, it just doesn’t make sense: there communications. However, these obvious, for example when they say is no obvious reason for them to be callers believe they have been spe- that a television program contains a an ongoing target of personalized cially selected as surveillance tar- message specifically designed and surveillance and harassment. gets, and sometimes for electronic inserted to affect their minds. or chemical bombardment too. My friend Steve Wright used The Truman Show Delusion One caller said he had written to work for the Omega Founda- With this background, I noticed a a political novel — unpublished — tion in Britain, which studies the book entitled Suspicious Minds. On and therefore the government was technology of repression, includ- the book jacket is the teaser “The monitoring his calls and following ing technologies for surveillance Truman Show delusion and other his every movement. He was very and electronic assault. He told me strange beliefs.” convincing. I suggested that he the Foundation would regularly The Truman Show is the name obtain evidence of the surveillance, hear from people who believed they of a film presenting the fictional but he always had some excuse, so were being electronically harassed. -
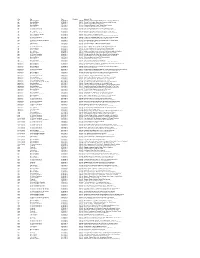
Key Pro Date Duration Segment Title Age Morning Edition 07/03/2013 0
Key Pro Date Duration Segment Title Age Morning Edition 07/03/2013 0:04:00 Doctors Recommend Baby Boomers Get Tested For Hepatitis C Age Morning Edition 07/05/2013 0:04:59 Seniors Flex Creative Muscles In Retirement Arts Colonies Age Tell Me More 07/08/2013 0:16:26 Winning Gold In Their Golden Years Age Morning Edition 07/11/2013 0:03:44 Chinatown 'Blessing Scams' Target Elderly Women Age Here & Now 07/18/2013 0:03:42 Cleveland Hosts National Senior Games Age All Things Considered 07/22/2013 0:07:20 Can Elderly Patients With Dementia Consent To Sex? Age All Things Considered 07/24/2013 0:05:37 Move Over Nursing Homes - There's Something Different Age Here & Now 07/25/2013 0:04:12 New Alzheimer's Research Could Lead To Treatments Age All Things Considered 07/26/2013 0:03:54 Age Hasn't Stopped This Man From Swimming And Winning Age Weekend Edition Sunday 07/28/2013 0:03:42 Athletic Glory At An Advanced Age Age Morning Edition 07/31/2013 0:03:55 Pickleball, Anyone? Senior Athletes Play New Games And Old Age All Things Considered 07/31/2013 0:04:45 For One Seniors Basketball Team, The Game Never Gets Old Age Here & Now 08/01/2013 0:16:27 Nursing Home Encourages Residents To Have Sex Age All Things Considered (Weekend) 08/03/2013 0:03:16 Worms' Bright Blue Death Could Shed Light On Human Aging Age Tell Me More 08/07/2013 0:01:35 Never Too Old To Take Gold Age Tell Me More 08/12/2013 0:19:38 Are We Ready For A Massive Aging Population? Age Morning Edition 08/20/2013 0:04:43 Older Farmers Seem To Be In No Hurry At All Age All Things Considered 08/23/2013 0:04:12 Summer Nights: Senior Softball In Huntington Beach, Calif. -

Representación De La Figura Del Luchador Profesional En Cuatro Cuentos Contemporáneos
COLEGIO DE HUMANIDADES Y CIENCIAS SOCIALES LICENCIATURA EN CREACIÓN LITERARIA Representación de la figura del luchador profesional en cuatro cuentos contemporáneos TRABAJO RECEPCIONAL QUE PARA OBTENER EL TÍTULO DE LICENCIADA EN CREACIÓN LITERARIA PRESENTA ANA LIDIA MARTÍNEZ ALBA Director del trabajo recepcional Dr. Gerardo Bustamante Bermúdez Ciudad de México, julio de 2017. SISTEMA BIBLIOTECARIO DE INFORMACIÓN Y DOCUMENTACIÓN UNIVERSIDAD AUTÓNOMA DE LA CIUDAD DE MÉXICO COORDINACIÓN ACADÉMICA RESTRICCIONES DE USO PARA LAS TESIS DIGITALES DERECHOS RESERVADOS© La presente obra y cada uno de sus elementos está protegido por la Ley Federal del Derecho de Autor; por la Ley de la Universidad Autónoma de la Ciudad de México, así como lo dispuesto por el Estatuto General Orgánico de la Universidad Autónoma de la Ciudad de México; del mismo modo por lo establecido en el Acuerdo por el cual se aprueba la Norma mediante la que se Modifican, Adicionan y Derogan Diversas Disposiciones del Estatuto Orgánico de la Universidad de la Ciudad de México, aprobado por el Consejo de Gobierno el 29 de enero de 2002, con el objeto de definir las atribuciones de las diferentes unidades que forman la estructura de la Universidad Autónoma de la Ciudad de México como organismo público autónomo y lo establecido en el Reglamento de Titulación de la Universidad Autónoma de la Ciudad de México. Por lo que el uso de su contenido, así como cada una de las partes que lo integran y que están bajo la tutela de la Ley Federal de Derecho de Autor, obliga a quien haga uso de la presente obra a considerar que solo lo realizará si es para fines educativos, académicos, de investigación o informativos y se compromete a citar esta fuente, así como a su autor ó autores. -

A CULTURAL HISTORY of MADNESS - Bloomsbury
A CULTURAL HISTORY OF MADNESS - Bloomsbury GENERAL EDITORS Jonathan Sadowsky, Case Western Reserve University, USA Chiara Thumiger, Kiel University, Germany AIMS & SCOPE Madness has strikingly ambiguous images in human history. All human societies seem to have a concept of madness, yet those concepts show extraordinary variance. Madness is widely seen, across time and cultures, as a medical problem, yet it often gestures towards other domains, including the religious, the moral, and the artistic. Madness impinges on the most personal and private sphere of human experience: how we understand the world, express ourselves about it, and share our mental, emotional and sensorial life with others. At the same time, madness is a public concern, often seeming to demand public response, at least by the immediate community, and often by the state. Madness is usually to some extent a disability, something that compromises functioning, yet is often also seen as a source of brilliance and inspiration. Madness is, virtually by definition, characterized by anomalous behavior, affect, and beliefs in any given context, and yet—partly because of this, and partly in spite of it— madness can be the most telling index of what a given society regards as normal or idealises as paradigm of functionality and health. In the ancient world, for example, reference to madness was used to qualify extraordinary characters, as in the famous case of the ‘melancholic’ as gifted individual, or of mania as associated to divine or poetic inspiration; unique experiences (religious, especially initiatory, but also creative and emotional); socio- political status (e.g., guilt deemed worthy of severe punishment, pollution); illness and bodily disturbance. -

Lucha Libre Mexicana. Máscaras a Través Del Tiempo
LUCHA LIBRE MEXICANA mascaras a traves del tiempo Por Julio Crespo Retoque fotografico Del hijo del Santo en uno de sus viajes a Japon, con el traje de batalla de los guerreros samurais. LUCHA LIBRE MEXICANA. MASCARAS A TRAVES DEL TIEMPO Por Julio Crespo La principal seña de identidad de la lucha libre en México es la máscara. Estos diseños que portan los luchadores son parte esencial en la creación de sus personajes, les confieren un sentido único, una intencionalidad, rodeando al luchador de un halo de misterio. Las máscaras son el bien más preciado que puede tener un luchador, y no hay mayor deshonra que perderla en una lucha de apuestas. LA HERENCIA DE LA MASCARA Con el paso de los años, las generaciones luchísticas mexicanas están defendiendo sus máscaras e incluso heredándolas, pasando éstas de padres a hijos (conocidas son las dinastías de los Villanos, los hermanos Dinamita, Santo el Enmascarado de Plata, Blue Demon, Tinieblas, Dos Caras). Las máscaras representan a un personaje y son defendidas por las nuevas generaciones incluso cuando los originales perdieron su incógnita, sus hijos o herederos retoman el personaje de nuevo enmascarado (como en los casos de Rey Misterio JR, Fishman JR, Dr Wagner JR, Rayo de Jalisco JR). También hay personajes que mantuvieron la incógnita durante toda su carrera y que sus juniors han perdido la máscara en lucha de apuestas, el ejemplo más reciente y más popular es Lizmark JR, quien perdió la máscara heredada de su padre en la función del 74º Aniversario de la lucha en México, organiza por el CMLL en 2007. -
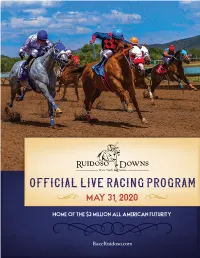
Official Live Racing Program May 31, 2020
OFFICIAL LIVE RACING PROGRAM MAY 31, 2020 HOME OF THE $3 MILLION ALL AMERICAN FUTURITY RaceRuidoso.com 2002 Sudderth Dr., Ruidoso NM 88345 RHONDA ROMACK-BURNS 575-937-3000 [email protected] OFFICE 575-257-3000 7TH DAY OF RACING • SUNDAY, MAY 31, 2020 • POST TIME 1:00PM weekend preview Friday - Mountain Top Futurity Trials (QH) This week’s racing card kicks off with 13 trial heats of 129 Quarter Horses vying for a spot in the Mountain Top Futurity. The top 10 qualifiers will run in the 350-yard, Grade II stakes race for 2-year- old New Mexico-bred horses that will be held on June 13th. Saturday - Ruidoso Maiden Stakes Trials Another great day of Quarter Horse trials is on tap with 45 Quarter Horses competing for a spot in the finals of the Ruidoso Maiden Stakes that will be run on June 14th. The top 10 qualifiers of 3, 4, and 5-year-olds will compete at 350 yards. Sunday - Dash For Speed Stakes The feature race of the day is the second running of the Dash For Speed Stakes for fillies and mares that are 3-years-old and up. Post time for the race is set for 4:55 PM and the horses will run 350 yards. The remainder of the program features a great mix of Quarter Horse and Thoroughbred racing. RACERUIDOSO.COM | 1 ruidoso downs SUNDAY, MAY 31, 2020 Ruidoso Downs Sunday, May 31, 2020 Horse Alphabetical Index 0$ 7 1 Ruidoso% * Downs 1 8 * ; ! 45/ " 0 / '' Sunday,2 May $= 31, ; , $ 2020 ;( % 0 $ $ * # + 8 %& , " %& 0 -& * * ! " 8 $ " * 2 % # Ruidoso -
![Luna Cšrnea 27[Final]](https://docslib.b-cdn.net/cover/3882/luna-c%C5%A1rnea-27-final-1633882.webp)
Luna Cšrnea 27[Final]
Black Shadow había perdido ya la lucha y el después se volvió explosivo. El Santo al fi- THE BLACK SHADOW PERDIÓ SU INCÓGNITA propio Santo quería quitarle la máscara. Blue nal le ganó el acto tirándole fuera del ring, Demon interviene. Hay un mare mágnum. azotándole contra los soportes de las Leopoldo Meraz La lucha del viernes pasado en la arena Coliseo cuerdas y le recibía con topes. El castigo registró entrada récord en los anales, pero para El Santo sólo fue “una lucha más” y para fue intenso. El árbitro Ruddy Blancarte The Black Shadow el derrumbe de la incógnita. El morbo del juego de máscaras que dos acabó contándole los tres segundos. tipos han hecho célebres –clásico Juan Pérez en la vida real– congregó a una clientela se- Blue Demon desesperado en el inter- dienta de fuertes emociones, esperando ver algo insólito y el vaticinio general se cumplió. medio, dio vida a su hermano y aunque El Santo fue un demonio en el final. No hubo nada raro. El Santo varias veces había ex- para la segunda caída El Santo dominó en puesto la máscara de plata y la había conservado porque es coloso en estos choques, y principio, “el gladiador de chicle” respon- aunque en esta vez The Black Shadow estuvo a la altura del titán, sus esfuerzos se estre- dió con golpes y le colocó un tirabuzón llaron ante el hombre de más experiencia. que aguantó El Santo estoicamente. Si- guió la pelea con dominio alterno, hubo ¿Fue ésta una lucha histórica? cambios de golpes, pero The Black Shadow Desde el punto de vista del gran número de es- se veía más entero, con más elasticidad, y pectadores, pasa la batalla como una de las en cambio, El Santo acusaba los efectos más interesantes. -

CNS Spectrums
CNS Spectrums http://journals.cambridge.org/CNS Additional services for CNS Spectrums: Email alerts: Click here Subscriptions: Click here Commercial reprints: Click here Terms of use : Click here The following abstracts were presented as posters at the 2015 NEI Psychopharmacology Congress CNS Spectrums / Volume 21 / Issue 01 / February 2016, pp 77 - 121 DOI: 10.1017/S1092852915000905, Published online: 22 February 2016 Link to this article: http://journals.cambridge.org/abstract_S1092852915000905 How to cite this article: (2016). The following abstracts were presented as posters at the 2015 NEI Psychopharmacology Congress. CNS Spectrums, 21, pp 77-121 doi:10.1017/S1092852915000905 Request Permissions : Click here Downloaded from http://journals.cambridge.org/CNS, IP address: 12.12.207.2 on 15 Mar 2016 CNS Spectrums (2016), 21,77–121. © Cambridge University Press 2016 doi:10.1017/S1092852915000905 ABSTRACTS The following abstracts were presented as posters at the 2015 NEI Psychopharmacology Congress Congratulations to the scientific poster winners of the 2015 NEI Psychopharmacology Congress! st 1 PLACE: Tardive Dyskinesia in the Era of Second Generation Antipsychotics: A Case Report and Literature Review (page 22) nd 2 PLACE: Comparing Deep Brain Stimulation (DBS) and ECT for Treatment Resistant Depression in Elderly Population (page 37) rd 3 PLACE: The Complex Multimodal Management of First-Psychotic Episode in Patients with Morphometric Alteration in Hippocampal Formation (page 30) Violent Video Games – Physiological and variability, emotion, sleep quality, violent video game, Psychological Impact on Children and desensitization, aggressiveness”. Adolescents: Literature Review RESULTS: Literature so far shows an association between Sree Latha Krishna Jadapalle, MD1 and Monifa daily exposure to violent video games and number of Seawell, MD1 depressive and anxiety symptoms among pre-adolescent youth.