Pediatrics Instructions: to Best Navigate the List, First Download This PDF File to Your Computer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tall Stature: a Difficult Diagnosis? Cristina Meazza1* , Chiara Gertosio2, Roberta Giacchero3, Sara Pagani1 and Mauro Bozzola1
Meazza et al. Italian Journal of Pediatrics (2017) 43:66 DOI 10.1186/s13052-017-0385-5 REVIEW Open Access Tall stature: a difficult diagnosis? Cristina Meazza1* , Chiara Gertosio2, Roberta Giacchero3, Sara Pagani1 and Mauro Bozzola1 Abstract Referral for an assessment of tall stature is less common than for short stature. Tall stature is defined as a height more than two standard deviations above the mean for age. The majority of subjects with tall stature show a familial tall stature or a constitutional advance of growth (CAG), which is a diagnosis of exclusion. After a careful physical evaluation, tall subjects may be divided into two groups: tall subjects with normal appearance and tall subjects with abnormal appearance. In the case of normal appearance, the paediatric endocrinologist will have to evaluate the growth rate. If it is normal for age and sex, the subject may be classified as having familial tall stature, CAG or obese subject, while if the growth rate is increased it is essential to evaluate pubertal status and thyroid status. Tall subjects with abnormal appearance and dysmorphisms can be classified into those with proportionate and disproportionate syndromes. A careful physical examination and an evaluation of growth pattern are required before starting further investigations. Physicians should always search for a pathological cause of tall stature, although the majority of children are healthy and they generally do not need treatment to cease growth progression. The most accepted and effective treatment for an excessive height prediction is inducing puberty early and leading to a complete fusion of the epiphyses and achievement of final height, using testosterone in males and oestrogens in females. -

Genetic Investigation of Patients with Tall Stature
2 182 E Vasco de Albuquerque Genetic investigation of tall 182:2 139–147 Clinical Study Albuquerque and others stature patients Genetic investigation of patients with tall stature Edoarda Vasco de Albuquerque Albuquerque1, Mariana Ferreira de Assis Funari2, Elisângela Pereira de Souza Quedas1, Rachel Sayuri Honjo Kawahira3, Raquel Soares Jallad4, Thaís Kataoka Homma1, Regina Matsunaga Martin2,5, Vinicius Nahime Brito2, Alexsandra Christianne Malaquias1,6, Antonio Marcondes Lerario1,7, Carla Rosenberg8, Ana Cristina Victorino Krepischi8, Chong Ae Kim3, Ivo Jorge Prado Arnhold2 and Alexander Augusto de Lima Jorge1 1Unidade de Endocrinologia Genética (LIM25), 2Unidade de Endocrinologia do Desenvolvimento, Laboratório de Hormônios e Genética Molecular (LIM42), Hospital das Clínicas da Faculdade de Medicina, Universidade de São Paulo (USP), São Paulo, Brasil, 3Unidade de Genética do Instituto da Criança, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo, Brasil, 4Unidade de Neuroendocrinologia, 5Unidade de Doenças Osteometabólicas, Hospital das Clínicas da Faculdade de Medicina, Universidade de São Paulo (USP), São Paulo, Brasil, 6Unidade de Endocrinologia Pediátrica, Correspondence Departamento de Pediatria, Irmandade da Santa Casa de Misericórdia de São Paulo, São Paulo, Brasil, 7Division of should be addressed Metabolism, Endocrinology and Diabetes, Department of Internal Medicine, University of Michigan, Ann Arbor, to A A L Jorge Michigan, USA, and 8Instituto de Biociências (IB), Universidade de São Paulo (USP), São Paulo, Brasil Email [email protected] Abstract Context: Patients with tall stature often remain undiagnosed after clinical investigation and few studies have genetically assessed this group, most of them without a systematic approach. Objective: To assess prospectively a group of individuals with tall stature, with and without syndromic features, and to establish a molecular diagnosis for their growth disorder. -
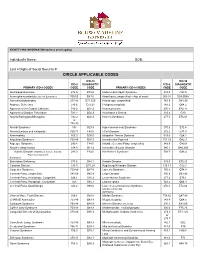
Circle Applicable Codes
IDENTIFYING INFORMATION (please print legibly) Individual’s Name: DOB: Last 4 Digits of Social Security #: CIRCLE APPLICABLE CODES ICD-10 ICD-10 ICD-9 DIAGNOSTIC ICD-9 DIAGNOSTIC PRIMARY ICD-9 CODES CODE CODE PRIMARY ICD-9 CODES CODE CODE Abetalipoproteinemia 272.5 E78.6 Hallervorden-Spatz Syndrome 333.0 G23.0 Acrocephalosyndactyly (Apert’s Syndrome) 755.55 Q87.0 Head Injury, unspecified – Age of onset: 959.01 S09.90XA Adrenaleukodystrophy 277.86 E71.529 Hemiplegia, unspecified 342.9 G81.90 Arginase Deficiency 270.6 E72.21 Holoprosencephaly 742.2 Q04.2 Agenesis of the Corpus Callosum 742.2 Q04.3 Homocystinuria 270.4 E72.11 Agenesis of Septum Pellucidum 742.2 Q04.3 Huntington’s Chorea 333.4 G10 Argyria/Pachygyria/Microgyria 742.2 Q04.3 Hurler’s Syndrome 277.5 E76.01 or 758.33 Aicardi Syndrome 333 G23.8 Hyperammonemia Syndrome 270.6 E72.4 Alcohol Embryo and Fetopathy 760.71 F84.5 I-Cell Disease 272.2 E77.0 Anencephaly 655.0 Q00.0 Idiopathic Torsion Dystonia 333.6 G24.1 Angelman Syndrome 759.89 Q93.5 Incontinentia Pigmenti 757.33 Q82.3 Asperger Syndrome 299.8 F84.5 Infantile Cerebral Palsy, unspecified 343.9 G80.9 Ataxia-Telangiectasia 334.8 G11.3 Intractable Seizure Disorder 345.1 G40.309 Autistic Disorder (Childhood Autism, Infantile 299.0 F84.0 Klinefelter’s Syndrome 758.7 Q98.4 Psychosis, Kanner’s Syndrome) Biotinidase Deficiency 277.6 D84.1 Krabbe Disease 333.0 E75.23 Canavan Disease 330.0 E75.29 Kugelberg-Welander Disease 335.11 G12.1 Carpenter Syndrome 759.89 Q87.0 Larsen’s Syndrome 755.8 Q74.8 Cerebral Palsy, unspecified 343.69 G80.9 -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

Level Estimates of Maternal Smoking and Nicotine Replacement Therapy During Pregnancy
Using primary care data to assess population- level estimates of maternal smoking and nicotine replacement therapy during pregnancy Nafeesa Nooruddin Dhalwani BSc MSc Thesis submitted to the University of Nottingham for the degree of Doctor of Philosophy November 2014 ABSTRACT Background: Smoking in pregnancy is the most significant preventable cause of poor health outcomes for women and their babies and, therefore, is a major public health concern. In the UK there is a wide range of interventions and support for pregnant women who want to quit. One of these is nicotine replacement therapy (NRT) which has been widely available for retail purchase and prescribing to pregnant women since 2005. However, measures of NRT prescribing in pregnant women are scarce. These measures are vital to assess its usefulness in smoking cessation during pregnancy at a population level. Furthermore, evidence of NRT safety in pregnancy for the mother and child’s health so far is nebulous, with existing studies being small or using retrospectively reported exposures. Aims and Objectives: The main aim of this work was to assess population- level estimates of maternal smoking and NRT prescribing in pregnancy and the safety of NRT for both the mother and the child in the UK. Currently, the only population-level data on UK maternal smoking are from repeated cross-sectional surveys or routinely collected maternity data during pregnancy or at delivery. These obtain information at one point in time, and there are no population-level data on NRT use available. As a novel approach, therefore, this thesis used the routinely collected primary care data that are currently available for approximately 6% of the UK population and provide longitudinal/prospectively recorded information throughout pregnancy. -
Macrocephaly Information Sheet 6-13-19
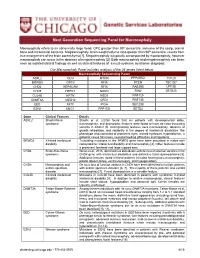
Next Generation Sequencing Panel for Macrocephaly Clinical Features: Macrocephaly refers to an abnormally large head, OFC greater than 98th percentile, inclusive of the scalp, cranial bone and intracranial contents. Megalencephaly, brain weight/volume ratio greater than 98th percentile, results from true enlargement of the brain parenchyma [1]. Megalencephaly is typically accompanied by macrocephaly, however macrocephaly can occur in the absence of megalencephaly [2]. Both macrocephaly and megalencephaly can been seen as isolated clinical findings as well as clinical features of a mutli-systemic syndromic diagnosis. Our Macrocephaly Panel includes analysis of the 36 genes listed below. Macrocephaly Sequencing Panel ASXL2 GLI3 MTOR PPP2R5D TCF20 BRWD3 GPC3 NFIA PTEN TBC1D7 CHD4 HEPACAM NFIX RAB39B UPF3B CHD8 HERC1 NONO RIN2 ZBTB20 CUL4B KPTN NSD1 RNF125 DNMT3A MED12 OFD1 RNF135 EED MITF PIGA SEC23B EZH2 MLC1 PPP1CB SETD2 Gene Clinical Features Details ASXL2 Shashi-Pena Shashi et al. (2016) found that six patients with developmental delay, syndrome macrocephaly, and dysmorphic features were found to have de novo truncating variants in ASXL2 [3]. Distinguishing features were macrocephaly, absence of growth retardation, and variability in the degree of intellectual disabilities The phenotype also consisted of prominent eyes, arched eyebrows, hypertelorism, a glabellar nevus flammeus, neonatal feeding difficulties and hypotonia. BRWD3 X-linked intellectual Truncating mutations in the BRWD3 gene have been described in males with disability nonsyndromic intellectual disability and macrocephaly [4]. Other features include a prominent forehead and large cupped ears. CHD4 Sifrim-Hitz-Weiss Weiss et al., 2016, identified five individuals with de novo missense variants in the syndrome CHD4 gene with intellectual disabilities and distinctive facial dysmorphisms [5]. -
Massachusetts Birth Defects 2002-2003
Massachusetts Birth Defects 2002-2003 Massachusetts Birth Defects Monitoring Program Bureau of Family Health and Nutrition Massachusetts Department of Public Health January 2008 Massachusetts Birth Defects 2002-2003 Deval L. Patrick, Governor Timothy P. Murray, Lieutenant Governor JudyAnn Bigby, MD, Secretary, Executive Office of Health and Human Services John Auerbach, Commissioner, Massachusetts Department of Public Health Sally Fogerty, Director, Bureau of Family Health and Nutrition Marlene Anderka, Director, Massachusetts Center for Birth Defects Research and Prevention Linda Casey, Administrative Director, Massachusetts Center for Birth Defects Research and Prevention Cathleen Higgins, Birth Defects Surveillance Coordinator Massachusetts Department of Public Health 617-624-5510 January 2008 Acknowledgements This report was prepared by the staff of the Massachusetts Center for Birth Defects Research and Prevention (MCBDRP) including: Marlene Anderka, Linda Baptiste, Elizabeth Bingay, Joe Burgio, Linda Casey, Xiangmei Gu, Cathleen Higgins, Angela Lin, Rebecca Lovering, and Na Wang. Data in this report have been collected through the efforts of the field staff of the MCBDRP including: Roberta Aucoin, Dorothy Cichonski, Daniel Sexton, Marie-Noel Westgate and Susan Winship. We would like to acknowledge the following individuals for their time and commitment to supporting our efforts in improving the MCBDRP. Lewis Holmes, MD, Massachusetts General Hospital Carol Louik, ScD, Slone Epidemiology Center, Boston University Allen Mitchell, -

Guidelines for Conducting Birth Defects Surveillance
NATIONAL BIRTH DEFECTS PREVENTION NETWORK HTTP://WWW.NBDPN.ORG Guidelines for Conducting Birth Defects Surveillance Edited By Lowell E. Sever, Ph.D. June 2004 Support for development, production, and distribution of these guidelines was provided by the Birth Defects State Research Partnerships Team, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention Copies of Guidelines for Conducting Birth Defects Surveillance can be viewed or downloaded from the NBDPN website at http://www.nbdpn.org/bdsurveillance.html. Comments and suggestions on this document are welcome. Submit comments to the Surveillance Guidelines and Standards Committee via e-mail at [email protected]. You may also contact a member of the NBDPN Executive Committee by accessing http://www.nbdpn.org and then selecting Network Officers and Committees. Suggested citation according to format of Uniform Requirements for Manuscripts ∗ Submitted to Biomedical Journals:∗ National Birth Defects Prevention Network (NBDPN). Guidelines for Conducting Birth Defects Surveillance. Sever, LE, ed. Atlanta, GA: National Birth Defects Prevention Network, Inc., June 2004. National Birth Defects Prevention Network, Inc. Web site: http://www.nbdpn.org E-mail: [email protected] ∗International Committee of Medical Journal Editors. Uniform requirements for manuscripts submitted to biomedical journals. Ann Intern Med 1988;108:258-265. We gratefully acknowledge the following individuals and organizations who contributed to developing, writing, editing, and producing this document. NBDPN SURVEILLANCE GUIDELINES AND STANDARDS COMMITTEE STEERING GROUP Carol Stanton, Committee Chair (CO) Larry Edmonds (CDC) F. John Meaney (AZ) Glenn Copeland (MI) Lisa Miller-Schalick (MA) Peter Langlois (TX) Leslie O’Leary (CDC) Cara Mai (CDC) EDITOR Lowell E. -

Diseases of the Digestive System (KOO-K93)
CHAPTER XI Diseases of the digestive system (KOO-K93) Diseases of oral cavity, salivary glands and jaws (KOO-K14) lijell Diseases of pulp and periapical tissues 1m Dentofacial anomalies [including malocclusion] Excludes: hemifacial atrophy or hypertrophy (Q67.4) K07 .0 Major anomalies of jaw size Hyperplasia, hypoplasia: • mandibular • maxillary Macrognathism (mandibular)(maxillary) Micrognathism (mandibular)( maxillary) Excludes: acromegaly (E22.0) Robin's syndrome (087.07) K07 .1 Anomalies of jaw-cranial base relationship Asymmetry of jaw Prognathism (mandibular)( maxillary) Retrognathism (mandibular)(maxillary) K07.2 Anomalies of dental arch relationship Cross bite (anterior)(posterior) Dis to-occlusion Mesio-occlusion Midline deviation of dental arch Openbite (anterior )(posterior) Overbite (excessive): • deep • horizontal • vertical Overjet Posterior lingual occlusion of mandibular teeth 289 ICO-N A K07.3 Anomalies of tooth position Crowding Diastema Displacement of tooth or teeth Rotation Spacing, abnormal Transposition Impacted or embedded teeth with abnormal position of such teeth or adjacent teeth K07.4 Malocclusion, unspecified K07.5 Dentofacial functional abnormalities Abnormal jaw closure Malocclusion due to: • abnormal swallowing • mouth breathing • tongue, lip or finger habits K07.6 Temporomandibular joint disorders Costen's complex or syndrome Derangement of temporomandibular joint Snapping jaw Temporomandibular joint-pain-dysfunction syndrome Excludes: current temporomandibular joint: • dislocation (S03.0) • strain (S03.4) K07.8 Other dentofacial anomalies K07.9 Dentofacial anomaly, unspecified 1m Stomatitis and related lesions K12.0 Recurrent oral aphthae Aphthous stomatitis (major)(minor) Bednar's aphthae Periadenitis mucosa necrotica recurrens Recurrent aphthous ulcer Stomatitis herpetiformis 290 DISEASES OF THE DIGESTIVE SYSTEM Diseases of oesophagus, stomach and duodenum (K20-K31) Ill Oesophagitis Abscess of oesophagus Oesophagitis: • NOS • chemical • peptic Use additional external cause code (Chapter XX), if desired, to identify cause. -

MECHANISMS in ENDOCRINOLOGY: Novel Genetic Causes of Short Stature
J M Wit and others Genetics of short stature 174:4 R145–R173 Review MECHANISMS IN ENDOCRINOLOGY Novel genetic causes of short stature 1 1 2 2 Jan M Wit , Wilma Oostdijk , Monique Losekoot , Hermine A van Duyvenvoorde , Correspondence Claudia A L Ruivenkamp2 and Sarina G Kant2 should be addressed to J M Wit Departments of 1Paediatrics and 2Clinical Genetics, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, Email The Netherlands [email protected] Abstract The fast technological development, particularly single nucleotide polymorphism array, array-comparative genomic hybridization, and whole exome sequencing, has led to the discovery of many novel genetic causes of growth failure. In this review we discuss a selection of these, according to a diagnostic classification centred on the epiphyseal growth plate. We successively discuss disorders in hormone signalling, paracrine factors, matrix molecules, intracellular pathways, and fundamental cellular processes, followed by chromosomal aberrations including copy number variants (CNVs) and imprinting disorders associated with short stature. Many novel causes of GH deficiency (GHD) as part of combined pituitary hormone deficiency have been uncovered. The most frequent genetic causes of isolated GHD are GH1 and GHRHR defects, but several novel causes have recently been found, such as GHSR, RNPC3, and IFT172 mutations. Besides well-defined causes of GH insensitivity (GHR, STAT5B, IGFALS, IGF1 defects), disorders of NFkB signalling, STAT3 and IGF2 have recently been discovered. Heterozygous IGF1R defects are a relatively frequent cause of prenatal and postnatal growth retardation. TRHA mutations cause a syndromic form of short stature with elevated T3/T4 ratio. Disorders of signalling of various paracrine factors (FGFs, BMPs, WNTs, PTHrP/IHH, and CNP/NPR2) or genetic defects affecting cartilage extracellular matrix usually cause disproportionate short stature. -

Supratentorial Brain Malformations
Supratentorial Brain Malformations Edward Yang, MD PhD Department of Radiology Boston Children’s Hospital 1 May 2015/ SPR 2015 Disclosures: Consultant, Corticometrics LLC Objectives 1) Review major steps in the morphogenesis of the supratentorial brain. 2) Categorize patterns of malformation that result from failure in these steps. 3) Discuss particular imaging features that assist in recognition of these malformations. 4) Reference some of the genetic bases for these malformations to be discussed in greater detail later in the session. Overview I. Schematic overview of brain development II. Abnormalities of hemispheric cleavage III. Commissural (Callosal) abnormalities IV. Migrational abnormalities - Gray matter heterotopia - Pachygyria/Lissencephaly - Focal cortical dysplasia - Transpial migration - Polymicrogyria V. Global abnormalities in size (proliferation) VI. Fetal Life and Myelination Considerations I. Schematic Overview of Brain Development Embryology Top Mid-sagittal Top Mid-sagittal Closed Neural Tube (4 weeks) Corpus Callosum Callosum Formation Genu ! Splenium Cerebral Hemisphere (11-20 weeks) Hemispheric Cleavage (4-6 weeks) Neuronal Migration Ventricular/Subventricular Zones Ventricle ! Cortex (8-24 weeks) Neuronal Precursor Generation (Proliferation) (6-16 weeks) Embryology From ten Donkelaar Clinical Neuroembryology 2010 4mo 6mo 8mo term II. Abnormalities of Hemispheric Cleavage Holoprosencephaly (HPE) Top Mid-sagittal Imaging features: Incomplete hemispheric separation + 1)1) No septum pellucidum in any HPEs Closed Neural -

R J M E ASE EPORT Romanian Journal of C R Morphology & Embryology
Rom J Morphol Embryol 2016, 57(4):1403–1408 R J M E ASE EPORT Romanian Journal of C R Morphology & Embryology http://www.rjme.ro/ Ovarian teratomas in a patient with Bardet–Biedl syndrome, a rare association IRINA TICA1), OANA-SORINA TICA2), ALINA DOINA NICOARĂ1), VLAD IUSTIN TICA3), ANDREI-ADRIAN TICA4) 1)Medical Department, Faculty of Medicine, “Ovidius” University, Constanta, Romania 2)Department of Mother and Child, Faculty of Medicine, University of Medicine and Pharmacy of Craiova, Romania 3)Department of Obstetrics and Gynecology, Faculty of Medicine, “Ovidius” University, Constanta, Romania 4)Research Center for Clinical and Experimental Medicine, University of Medicine and Pharmacy of Craiova, Romania Abstract Bardet–Biedl syndrome (BBS) represents a rare ciliopathy recessive autosomal inherited. The main clinical features are retinal dystrophy, postaxial polydactyly, obesity, different degrees of cognitive deficit, renal impairment, hypogonadism and genital malformations. The genetic explanation consists in BBS genes mutations, which encode modified proteins, altering the function of the immotile cilia. As a multitude of BBS genes mutations were described, the phenotypic aspect of these disorders varies according to that. We present the case of a 22 years old female patient, known with BBS since the age of 11 and which was diagnosed and operated for bilateral ovarian dermoid cysts, at the age of 21. We did not find a similar case in literature, regarding the association between the two disorders. We consider that our case points towards the importance of periodic imagistic evaluations [magnetic resonance imaging (MRI), computed tomography (CT) or ultrasound] of these patients, not only clinical and biological.