Massachusetts Birth Defects 2002-2003
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Educational Paper Ciliopathies
Eur J Pediatr (2012) 171:1285–1300 DOI 10.1007/s00431-011-1553-z REVIEW Educational paper Ciliopathies Carsten Bergmann Received: 11 June 2011 /Accepted: 3 August 2011 /Published online: 7 September 2011 # The Author(s) 2011. This article is published with open access at Springerlink.com Abstract Cilia are antenna-like organelles found on the (NPHP) . Ivemark syndrome . Meckel syndrome (MKS) . surface of most cells. They transduce molecular signals Joubert syndrome (JBTS) . Bardet–Biedl syndrome (BBS) . and facilitate interactions between cells and their Alstrom syndrome . Short-rib polydactyly syndromes . environment. Ciliary dysfunction has been shown to Jeune syndrome (ATD) . Ellis-van Crefeld syndrome (EVC) . underlie a broad range of overlapping, clinically and Sensenbrenner syndrome . Primary ciliary dyskinesia genetically heterogeneous phenotypes, collectively (Kartagener syndrome) . von Hippel-Lindau (VHL) . termed ciliopathies. Literally, all organs can be affected. Tuberous sclerosis (TSC) . Oligogenic inheritance . Modifier. Frequent cilia-related manifestations are (poly)cystic Mutational load kidney disease, retinal degeneration, situs inversus, cardiac defects, polydactyly, other skeletal abnormalities, and defects of the central and peripheral nervous Introduction system, occurring either isolated or as part of syn- dromes. Characterization of ciliopathies and the decisive Defective cellular organelles such as mitochondria, perox- role of primary cilia in signal transduction and cell isomes, and lysosomes are well-known -

Genetic and Flow Anomalies in Congenital Heart Disease
Published online: 2021-05-10 AIMS Genetics, 3(3): 157-166. DOI: 10.3934/genet.2016.3.157 Received: 01 July 2016 Accepted: 16 August 2016 Published: 23 August 2016 http://www.aimspress.com/journal/Genetics Review Genetic and flow anomalies in congenital heart disease Sandra Rugonyi* Department of Biomedical Engineering, Oregon Health & Science University, 3303 SW Bond Ave. M/C CH13B, Portland, OR 97239, USA * Correspondence: Email: [email protected]; Tel: +1-503-418-9310; Fax: +1-503-418-9311. Abstract: Congenital heart defects are the most common malformations in humans, affecting approximately 1% of newborn babies. While genetic causes of congenital heart disease have been studied, only less than 20% of human cases are clearly linked to genetic anomalies. The cause for the majority of the cases remains unknown. Heart formation is a finely orchestrated developmental process and slight disruptions of it can lead to severe malformations. Dysregulation of developmental processes leading to heart malformations are caused by genetic anomalies but also environmental factors including blood flow. Intra-cardiac blood flow dynamics plays a significant role regulating heart development and perturbations of blood flow lead to congenital heart defects in animal models. Defects that result from hemodynamic alterations recapitulate those observed in human babies, even those due to genetic anomalies and toxic teratogen exposure. Because important cardiac developmental events, such as valve formation and septation, occur under blood flow conditions while the heart is pumping, blood flow regulation of cardiac formation might be a critical factor determining cardiac phenotype. The contribution of flow to cardiac phenotype, however, is frequently ignored. -

The Role of Echocardiography in the Management of Adult Patients with Congenital Heart Disease Following Operative Treatment
779 Review Article The role of echocardiography in the management of adult patients with congenital heart disease following operative treatment Kálmán Havasi, Nóra Ambrus, Anita Kalapos, Tamás Forster, Attila Nemes 2nd Department of Medicine and Cardiology Centre, Medical Faculty, Albert Szent-Györgyi Clinical Centre, University of Szeged, Szeged, Hungary Contributions: (I) Conception and design: K Havasi; (II) Administrative support: N Ambrus, A Kalapos; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: K Havasi; (V) Data analysis and interpretation: K Havasi, N Ambrus, A Kalapos; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Attila Nemes, MD, PhD, DSc, FESC. 2nd Department of Medicine and Cardiology Centre, Medical Faculty, Albert Szent-Györgyi Clinical Centre, University of Szeged, H-6725 Szeged, Semmelweis street 8, Szeged, Hungary. Email: [email protected]. Abstract: Treatment of congenital heart diseases has significantly advanced over the last few decades. Due to the continuously increasing survival rate, there are more and more adult patients with congenital heart diseases and these patients present at the adult cardiologist from the paediatric cardiology care. The aim of the present review is to demonstrate the role of echocardiography in some significant congenital heart diseases. Keywords: Echocardiography; congenital heart disease; adult Submitted Jul 03, 2018. Accepted for publication Sep 07, 2018. doi: 10.21037/cdt.2018.09.11 View this article at: http://dx.doi.org/10.21037/cdt.2018.09.11 Introduction if the patient’s condition is evaluated by the proper imaging modality. Therefore, the treating physician should know the Treatment of congenital heart diseases has significantly benefits, disadvantages and clinical indications of the certain advanced during the last few decades. -

Approach to Brain Malformations
Approach to Brain Malformations A General Imaging Approach to Brain CSF spaces. This is the basis for development of the Dandy- Malformations Walker malformation; it requires abnormal development of the cerebellum itself and of the overlying leptomeninges. Whenever an infant or child is referred for imaging because of Looking at the midline image also gives an idea of the relative either seizures or delayed development, the possibility of a head size through assessment of the craniofacial ratio. In the brain malformation should be carefully investigated. If the normal neonate, the ratio of the cranial vault to the face on child appears dysmorphic in any way (low-set ears, abnormal midline images is 5:1 or 6:1. By 2 years, it should be 2.5:1, and facies, hypotelorism), the likelihood of an underlying brain by 10 years, it should be about 1.5:1. malformation is even higher, but a normal appearance is no guarantee of a normal brain. In all such cases, imaging should After looking at the midline, evaluate the brain from outside be geared toward showing a structural abnormality. The to inside. Start with the cerebral cortex. Is the thickness imaging sequences should maximize contrast between gray normal (2-3 mm)? If it is too thick, think of pachygyria or matter and white matter, have high spatial resolution, and be polymicrogyria. Is the cortical white matter junction smooth or acquired as volumetric data whenever possible so that images irregular? If it is irregular, think of polymicrogyria or Brain: Pathology-Based Diagnoses can be reformatted in any plane or as a surface rendering. -
Research Day 2021 Program
Western Michigan University ScholarWorks at WMU Research Day WMU Homer Stryker M.D. School of Medicine 2021 Research Day 2021 Program Western Michigan University Homer Stryker M.D. School of Medicine Follow this and additional works at: https://scholarworks.wmich.edu/medicine_research_day Part of the Life Sciences Commons, and the Medicine and Health Sciences Commons WMU ScholarWorks Citation Homer Stryker M.D. School of Medicine, Western Michigan University, "Research Day 2021 Program" (2021). Research Day. 298. https://scholarworks.wmich.edu/medicine_research_day/298 This Abstract is brought to you for free and open access by the WMU Homer Stryker M.D. School of Medicine at ScholarWorks at WMU. It has been accepted for inclusion in Research Day by an authorized administrator of ScholarWorks at WMU. For more information, please contact [email protected]. th 38 Annual Kalamazoo Community Medical and Health Sciences Virtual Research Day Wednesday, April 21, 2021 8:00 a.m. – 12:00 p.m. TABLE OF CONTENTS INTRODUCTION ........................................................................................................... 4 KEYNOTE SPEAKER.................................................................................................... 6 SCHEDULE ..................................................................................................................... 7 ORAL PRESENTATIONS ............................................................................................. 8 ORAL ABSTRACTS .................................................................................................... -
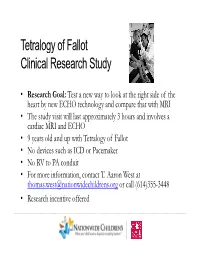
Tetralogy of Fallot Clinical Research Study
Tetralogy of Fallot Clinical Research Study • Research Goal: Test a new way to look at the right side of the heart by new ECHO technology and compare that with MRI • The stu dy v is it w ill last approx imate ly 3 h ours an d ilinvolves a cardiac MRI and ECHO • 9 years old and up with Tetralogy of Fallot • No devices such as ICD or Pacemaker • No RV to PA conduit • For more information, contact T. Aaron West at [email protected] or call (614)355-3448 • Research incentive offered ………………..…………………………………………………………………………………………………………………………………….. Tetralogy of Fallot Past, Present, Future Stephen R. Crumb, APN Coordinator, COACH Program Columbus Ohio Adult Congenital Heart ………………..…………………………………………………………………………………………………………………………………….. Disclosure: Go Buck(y)(s) ? Survival to 18 years of age with CHD 1980 – 90 1970 – 75 Year Born with CHD 1960 – 40 1940 – 20 0 10 20 30 40 50 60 70 80 90 100 ………………..…………………………………………………………………………………………………………………………………….. Pediatric to Adult Congenital Heart Disease Expanding Population of Adol escents and AdAdlults Increased Mid Term with CHD Survival Increased Early Lower Perioperative Survival Mortality Early Complete Improved Surgical Repair Techniques Advances in Fetal Diagnosis NICU Care Incidence of CHD ………………..…………………………………………………………………………………………………………………………………….. Ratio of Pediatric to Adult Patients with CHD Pediatric patients Adult patients 1965 1985 2005 ………………..…………………………………………………………………………………………………………………………………….. Normal Heart Tetralogy of Fallot ETIENNE-LOUIS ARTHUR FALLOT Mixing red and blue -
ARPKD): Kidney-Related and Non-Kidney-Related Phenotypes
Pediatr Nephrol (2014) 29:1915–1925 DOI 10.1007/s00467-013-2634-1 EDUCATIONAL REVIEW Clinical manifestations of autosomal recessive polycystic kidney disease (ARPKD): kidney-related and non-kidney-related phenotypes Rainer Büscher & Anja K. Büscher & Stefanie Weber & Julia Mohr & Bianca Hegen & Udo Vester & Peter F. Hoyer Received: 26 April 2013 /Revised: 5 September 2013 /Accepted: 6 September 2013 /Published online: 10 October 2013 # IPNA 2013 Abstract Autosomal recessive polycystic kidney disease disease. In this review we focus on common and uncommon (ARPKD), although less frequent than the dominant form, is kidney-related and non-kidney-related phenotypes. Clinical a common, inherited ciliopathy of childhood that is caused by management of ARPKD patients should include consideration mutations in the PKHD1-gene on chromosome 6. The charac- of potential problems related to these manifestations. teristic dilatation of the renal collecting ducts starts in utero and can present at any stage from infancy to adulthood. Renal Keywords ARPKD . Extrarenal manifestation . Children . insufficiency may already begin in utero and may lead to early Hepatic fibrosis . Portal hypertension . Caroli’ssyndrome abortion or oligohydramnios and lung hypoplasia in the new- born. However, there are also affected children who have no evidence of renal dysfunction in utero and who are born with Introduction normal renal function. Up to 30 % of patients die in the perinatal period, and those surviving the neonatal period reach Autosomal recessive polycystic kidney disease (ARPKD) be- end stage renal disease (ESRD) in infancy, early childhood or longs to the family of cilia-related disorders and is an important adolescence. In contrast, some affected patients have been inherited disease with distinct clinical features and genetics. -

World Journal of Pharmaceutical and Life Sciences
wjpls, 2017, Vol. 3, Issue 8, 66-68 Review Article ISSN 2454-2229 Farman . World Journal of Pharmaceutical World Journal and Lifeof Pharmaceutical Sciences and Life Sciences WJPLS www.wjpls.org SJIF Impact Factor: 4.223 ONE TOO MANY- POLYORCHIDISM A RARE CASE REPORT AND REVIEW OF LITERATURE Dr. Farman Ali* India. *Corresponding Author: Dr. Farman Ali India. Email ID: [email protected], Article Received on 12/08/2017 Article Revised on 03/09/2017 Article Accepted on 24/09/2017 ABSTRACT Polyorchidism is the incidence of more than two testicles in a male. It is a rare congenital anomaly involving the abnormal division of the genital ridge longitudinally or transversely, mainly occurring in the scrotum. Triorchidism(presence of 3 testes) is the most common occurrence of this condition. They mostly occur on the left side. There have been only 140-200 pathological cases that are published in world journal literature, out of which only a few cases have been reported in India. A rare case was reported of a 20 year old man with polyorchidism presenting with an inguinal hernia, describing the clinical features, it's surgical findings and a review of the literature. The most common sites are: Scrotal(66%), inguinal(25%), and abdominal(9%). This condition is mostly asymptomatic but may commonly present with features like maldescent(40%), hernia(30%), torsion(15%), hydrocoele(9%) and malignancy(6%). Spermatogenesis may be normal only in 50% of cases. If symptoms present, they may be scrotal pain, swelling and infertility. High accuracy of pre-operative ultrasound evaluation of scrotal mass differentiates this benign entity from ominous abnormalities and prevents unnecessary surgical exploration of sonographically normal, uncomplicated and orthotopic supernumerary testes. -

Targeted Exome Sequencing Provided Comprehensive Genetic Diagnosis of Congenital Anomalies of the Kidney and Urinary Tract
Journal of Clinical Medicine Article Targeted Exome Sequencing Provided Comprehensive Genetic Diagnosis of Congenital Anomalies of the Kidney and Urinary Tract 1,2, 3,4, 3 1,5 Yo Han Ahn y, Chung Lee y, Nayoung K. D. Kim , Eujin Park , Hee Gyung Kang 1,2,6,* , Il-Soo Ha 1,2,6, Woong-Yang Park 3,4,7 and Hae Il Cheong 1,2,6 1 Department of Pediatrics, Seoul National University College of Medicine, Seoul 03080, Korea; [email protected] (Y.H.A.); [email protected] (E.P.); [email protected] (I.-S.H.); [email protected] (H.I.C.) 2 Department of Pediatrics, Seoul National University Children’s Hospital, Seoul 03080, Korea 3 Samsung Genome Institute, Samsung Medical Center, Seoul 06351, Korea; [email protected] (C.L.); [email protected] (N.K.D.K.); [email protected] (W.-Y.P.) 4 Department of Health Sciences and Technology, Samsung Advanced Institute for Health Sciences and Technology, Sungkyunkwan University, Seoul 06351, Korea 5 Department of Pediatrics, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul 07441, Korea 6 Kidney Research Institute, Medical Research Center, Seoul National University College of Medicine, Seoul 03080, Korea 7 Department of Molecular Cell Biology, Sungkyunkwan University School of Medicine, Suwon 16419, Korea * Correspondence: [email protected] These authors equally contributed to this article. y Received: 31 January 2020; Accepted: 8 March 2020; Published: 10 March 2020 Abstract: Congenital anomalies of the kidney and urinary tract (CAKUT) are the most common cause of chronic kidney disease in children. -

Genetics of Congenital Hand Anomalies
G. C. Schwabe1 S. Mundlos2 Genetics of Congenital Hand Anomalies Die Genetik angeborener Handfehlbildungen Original Article Abstract Zusammenfassung Congenital limb malformations exhibit a wide spectrum of phe- Angeborene Handfehlbildungen sind durch ein breites Spektrum notypic manifestations and may occur as an isolated malforma- an phänotypischen Manifestationen gekennzeichnet. Sie treten tion and as part of a syndrome. They are individually rare, but als isolierte Malformation oder als Teil verschiedener Syndrome due to their overall frequency and severity they are of clinical auf. Die einzelnen Formen kongenitaler Handfehlbildungen sind relevance. In recent years, increasing knowledge of the molecu- selten, besitzen aber aufgrund ihrer Häufigkeit insgesamt und lar basis of embryonic development has significantly enhanced der hohen Belastung für Betroffene erhebliche klinische Rele- our understanding of congenital limb malformations. In addi- vanz. Die fortschreitende Erkenntnis über die molekularen Me- tion, genetic studies have revealed the molecular basis of an in- chanismen der Embryonalentwicklung haben in den letzten Jah- creasing number of conditions with primary or secondary limb ren wesentlich dazu beigetragen, die genetischen Ursachen kon- involvement. The molecular findings have led to a regrouping of genitaler Malformationen besser zu verstehen. Der hohe Grad an malformations in genetic terms. However, the establishment of phänotypischer Variabilität kongenitaler Handfehlbildungen er- precise genotype-phenotype correlations for limb malforma- schwert jedoch eine Etablierung präziser Genotyp-Phänotyp- tions is difficult due to the high degree of phenotypic variability. Korrelationen. In diesem Übersichtsartikel präsentieren wir das We present an overview of congenital limb malformations based Spektrum kongenitaler Malformationen, basierend auf einer ent- 85 on an anatomic and genetic concept reflecting recent molecular wicklungsbiologischen, anatomischen und genetischen Klassifi- and developmental insights. -

CONGENITAL ABNORMALITIES of the CENTRAL NERVOUS SYSTEM Christopher Verity, Helen Firth, Charles Ffrench-Constant *I3
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.74.suppl_1.i3 on 1 March 2003. Downloaded from CONGENITAL ABNORMALITIES OF THE CENTRAL NERVOUS SYSTEM Christopher Verity, Helen Firth, Charles ffrench-Constant *i3 J Neurol Neurosurg Psychiatry 2003;74(Suppl I):i3–i8 dvances in genetics and molecular biology have led to a better understanding of the control of central nervous system (CNS) development. It is possible to classify CNS abnormalities Aaccording to the developmental stages at which they occur, as is shown below. The careful assessment of patients with these abnormalities is important in order to provide an accurate prog- nosis and genetic counselling. c NORMAL DEVELOPMENT OF THE CNS Before we review the various abnormalities that can affect the CNS, a brief overview of the normal development of the CNS is appropriate. c Induction—After development of the three cell layers of the early embryo (ectoderm, mesoderm, and endoderm), the underlying mesoderm (the “inducer”) sends signals to a region of the ecto- derm (the “induced tissue”), instructing it to develop into neural tissue. c Neural tube formation—The neural ectoderm folds to form a tube, which runs for most of the length of the embryo. c Regionalisation and specification—Specification of different regions and individual cells within the neural tube occurs in both the rostral/caudal and dorsal/ventral axis. The three basic regions of copyright. the CNS (forebrain, midbrain, and hindbrain) develop at the rostral end of the tube, with the spinal cord more caudally. Within the developing spinal cord specification of the different popu- lations of neural precursors (neural crest, sensory neurones, interneurones, glial cells, and motor neurones) is observed in progressively more ventral locations. -

Guidelines for Conducting Birth Defects Surveillance
NATIONAL BIRTH DEFECTS PREVENTION NETWORK HTTP://WWW.NBDPN.ORG Guidelines for Conducting Birth Defects Surveillance Edited By Lowell E. Sever, Ph.D. June 2004 Support for development, production, and distribution of these guidelines was provided by the Birth Defects State Research Partnerships Team, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention Copies of Guidelines for Conducting Birth Defects Surveillance can be viewed or downloaded from the NBDPN website at http://www.nbdpn.org/bdsurveillance.html. Comments and suggestions on this document are welcome. Submit comments to the Surveillance Guidelines and Standards Committee via e-mail at [email protected]. You may also contact a member of the NBDPN Executive Committee by accessing http://www.nbdpn.org and then selecting Network Officers and Committees. Suggested citation according to format of Uniform Requirements for Manuscripts ∗ Submitted to Biomedical Journals:∗ National Birth Defects Prevention Network (NBDPN). Guidelines for Conducting Birth Defects Surveillance. Sever, LE, ed. Atlanta, GA: National Birth Defects Prevention Network, Inc., June 2004. National Birth Defects Prevention Network, Inc. Web site: http://www.nbdpn.org E-mail: [email protected] ∗International Committee of Medical Journal Editors. Uniform requirements for manuscripts submitted to biomedical journals. Ann Intern Med 1988;108:258-265. We gratefully acknowledge the following individuals and organizations who contributed to developing, writing, editing, and producing this document. NBDPN SURVEILLANCE GUIDELINES AND STANDARDS COMMITTEE STEERING GROUP Carol Stanton, Committee Chair (CO) Larry Edmonds (CDC) F. John Meaney (AZ) Glenn Copeland (MI) Lisa Miller-Schalick (MA) Peter Langlois (TX) Leslie O’Leary (CDC) Cara Mai (CDC) EDITOR Lowell E.