Signs in Thoracic Imaging Geoffrey B
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

X-Ray Interpretation
Objectives Describe a systematic method for interpretation of chest and abdomen x-rays List findings to accurately identify common X-ray Interpretation pathology in chest & abdomen x-rays Describe a systematic method to approach the Denise Ramponi, DNP, FNP-C, ENP-BC, FAANP, FAEN important components in interpretation of upper & lower extremity x-rays Chest X-ray: Standard Views Lateral Film Postero-anterior (PA): (LAT) view can determine th On inspiration – diaphragm descends to 10 rib the anterior-posterior posteriorly structures along the axis of the body Normal LAT film Counting Ribs AP View - Portable http://www.lumen.luc.edu/lumen/MedEd/medicine/pulmonar/cxr/cxr_f.htm When the patient is unable to tolerate routine views with pts sitting or supine No participation from the patient Film is against the patient's back (supine) 1 Consolidation, Atelectasis, Chest radiograph Interstitial involvement Consolidation - any pathologic process that fills the alveoli with Left and right heart fluid, pus, blood, cells or other borders well defined substances Interstitial - involvement of the Both hemidiaphragms supporting tissue of the lung visible to midline parenchyma resulting in fine or coarse reticular opacities Right - higher Atelectasis - collapse of a part of Heart less than 50% of the lung due to a decrease in the amount of air resulting in volume diameter of the chest loss and increased density. Infiltrate, Consolidation vs. Congestive Heart Failure Atelectasis Fluid leaking into interstitium Kerley B 2 Kerley B lines Prominent interstitial markings Kerley lines Magnified CXR Cardiomyopathy & interstitial pulmonary edema Short 1-2 cm white lines at lung periphery horizontal to pleural surface Distended interlobular septa - secondary to interstitial edema. -

Diagnosing Pulmonary Embolism M Riedel
309 Postgrad Med J: first published as 10.1136/pgmj.2003.007955 on 10 June 2004. Downloaded from REVIEW Diagnosing pulmonary embolism M Riedel ............................................................................................................................... Postgrad Med J 2004;80:309–319. doi: 10.1136/pgmj.2003.007955 Objective testing for pulmonary embolism is necessary, embolism have a low long term risk of subse- quent VTE.2 5–7 because clinical assessment alone is unreliable and the consequences of misdiagnosis are serious. No single test RISK FACTORS AND RISK has ideal properties (100% sensitivity and specificity, no STRATIFICATION risk, low cost). Pulmonary angiography is regarded as the The factors predisposing to VTE broadly fit Virchow’s triad of venous stasis, injury to the final arbiter but is ill suited for diagnosing a disease vein wall, and enhanced coagulability of the present in only a third of patients in whom it is suspected. blood (box 1). The identification of risk factors Some tests are good for confirmation and some for aids clinical diagnosis of VTE and guides decisions about repeat testing in borderline exclusion of embolism; others are able to do both but are cases. Primary ‘‘thrombophilic’’ abnormalities often non-diagnostic. For optimal efficiency, choice of the need to interact with acquired risk factors before initial test should be guided by clinical assessment of the thrombosis occurs; they are usually discovered after the thromboembolic event. Therefore, the likelihood of embolism and by patient characteristics that risk of VTE is best assessed by recognising the may influence test accuracy. Standardised clinical presence of known ‘‘clinical’’ risk factors. estimates can be used to give a pre-test probability to However, investigations for thrombophilic dis- orders at follow up should be considered in those assess, after appropriate objective testing, the post-test without another apparent explanation. -

Chest and Abdominal Radiograph 101
Chest and Abdominal Radiograph 101 Ketsia Pierre MD, MSCI July 16, 2010 Objectives • Chest radiograph – Approach to interpreting chest films – Lines/tubes – Pneumothorax/pneumomediastinum/pneumopericar dium – Pleural effusion – Pulmonary edema • Abdominal radiograph – Tubes – Bowel gas pattern • Ileus • Bowel obstruction – Pneumoperitoneum First things first • Turn off stray lights, optimize room lighting • Patient Data – Correct patient – Patient history – Look at old films • Routine Technique: AP/PA, exposure, rotation, supine or erect Approach to Reading a Chest Film • Identify tubes and lines • Airway: trachea midline or deviated, caliber change, bronchial cut off • Cardiac silhouette: Normal/enlarged • Mediastinum • Lungs: volumes, abnormal opacity or lucency • Pulmonary vessels • Hila: masses, lymphadenopathy • Pleura: effusion, thickening, calcification • Bones/soft tissues (four corners) Anatomy of a PA Chest Film TUBES Endotracheal Tubes Ideal location for ETT Is 5 +/‐ 2 cm from carina ‐Normal ETT excursion with flexion and extension of neck 2 cm. ETT at carina Right mainstem Intubation ‐Right mainstem intubation with left basilar atelectasis. ETT too high Other tubes to consider DHT down right mainstem DHT down left mainstem NGT with tip at GE junction CENTRAL LINES Central Venous Line Ideal location for tip of central venous line is within superior vena cava. ‐ Risk of thrombosis decreased in central veins. ‐ Catheter position within atrium increases risk of perforation Acceptable central line positions • Zone A –distal SVC/superior atriocaval junction. • Zone B – proximal SVC • Zone C –left brachiocephalic vein. Right subclavian central venous catheter directed cephalad into IJ Where is this tip? Hemiazygous Or this one? Right vertebral artery Pulmonary Arterial Catheter Ideal location for tip of PA catheter within mediastinal shadow. -
Cardiothoracic Fellowship Program
Cardiothoracic Fellowship Program Table of Contents Program Contact ............................................................................................ 3 Other contact numbers .................................................................................. 4 Introduction ........................................................................................................... 5 Goals and Objectives of Fellowship: ..................................................................... 6 Rotation Schedule: ........................................................................................ 7 Core Curriculum .................................................................................................... 8 Fellow’s Responsibilities ..................................................................................... 22 Resources ........................................................................................................... 23 Facilities ....................................................................................................... 23 Educational Program .......................................................................................... 26 Duty Hours .......................................................................................................... 29 Evaluation ........................................................................................................... 30 Table of Appendices .................................................................................... 31 Appendix A -
Screening Chest X-Ray Interpretations and Radiographic Techniques IOM GUIDELINES FIRST EDITION Iii
FIRST EDITION 2015 Screening Chest X-Ray Interpretations and Radiographic Techniques IOM GUIDELINES Global Radiology Coordination and Teleradiology Centre Migration Health Division International Organization for Migration (Manila Administrative Centre) 24th floor Citibank Tower, Paseo De Roxas 8741, Makati city 1226 Metro Manila, Philippines Email: [email protected] • [email protected] Tel: +632 230 1674 The opinions expressed in the report are those of the authors and do not necessarily reflect the views of the International Organization for Migration (IOM). The designations employed and the presentation of material throughout the report do not imply the expression of any opinion whatsoever on the part of IOM concerning the legal status of any country, territory, city or area, or of its authorities, or concerning its frontiers or boundaries. IOM is committed to the principle that humane and orderly migration benefits migrants and society. As an intergovernmental organization, IOM acts with its partners in the international community to: assist in meeting the operational challenges of migration; advance understanding of migration issues; encourage social and economic development through migration; and uphold the human dignity and well-being of migrants. Author Sifrash Meseret GELAW, MD Radiologist, MPH; Global Radiology Coordinator IOM, Manila Administrative Centre, Manila, Philippines Major Contributor Anthony MACDERMOTT, MD former Global HAP Quality Coordinator, IOM, Regional Office for Asia and the Pacific, Bangkok, Thailand Additional -

Pediatrics-EOR-Outline.Pdf
DERMATOLOGY – 15% Acne Vulgaris Inflammatory skin condition assoc. with papules & pustules involving pilosebaceous units Pathophysiology: • 4 main factors – follicular hyperkeratinization with plugging of sebaceous ducts, increased sebum production, Propionibacterium acnes overgrowth within follicles, & inflammatory response • Hormonal activation of pilosebaceous glands which may cause cyclic flares that coincide with menstruation Clinical Manifestations: • In areas with increased sebaceous glands (face, back, chest, upper arms) • Stage I: Comedones: small, inflammatory bumps from clogged pores - Open comedones (blackheads): incomplete blockage - Closed comedones (whiteheads): complete blockage • Stage II: Inflammatory: papules or pustules surrounded by inflammation • Stage III: Nodular or cystic acne: heals with scarring Differential Diagnosis: • Differentiate from rosacea which has no comedones** • Perioral dermatitis based on perioral and periorbital location • CS-induced acne lacks comedones and pustules are in same stage of development Diagnosis: • Mild: comedones, small amounts of papules &/or pustules • Moderate: comedones, larger amounts of papules &/or pustules • Severe: nodular (>5mm) or cystic Management: • Mild: topical – azelaic acid, salicylic acid, benzoyl peroxide, retinoids, Tretinoin topical (Retin A) or topical antibiotics [Clindamycin or Erythromycin with Benzoyl peroxide] • Moderate: above + oral antibiotics [Minocycline 50mg PO qd or Doxycycline 100 mg PO qd], spironolactone • Severe (refractory nodular acne): oral -

The Supine Pneumothorax
Annals of the Royal College of Surgeons of England (1987) vol. 69 The supine pneumothorax DAVID A P COOKE FRCS Surgical Registrar, Department ofSurgery, St Thomas' Hospital JULIE C COOKE FRCR* Radiological Senior Registrar, Department ofDiagnostic Radiology, Brompton Hospital, London Key words: PNEUMOTHORAX; COMPUTI ED TOMOGRAPHY; TRAUMA Summary TABLE I Causes of a pneumothorax The consequences of an undiagnosed pneumothorax can be life- threatening, particularly in patients with trauma to the head or Broncho-pulmonay pathology Traumatic injuy and in those mechanical ventilation. Yet multiple requiring Asthma it is these patients, whose films will be assessed initially by the Bronchial adenoma surgeon, who are more likely to have a chest X-ray taken in the Bronchial carcinoma Penetrating trauma supine position. The features of supine pneumothoraces are de- Emphysema Blunt trauma scribed and discussed together with radiological techniques used to Fibrosing alveolitis Inhaled foreign body confirm the diagnosis, including computed tomography (CT) Idiopathic which may be ofparticular importance in patients with associated Marfan's syndrome fatrogenic cranial trauma. Pulmonary abscess Pulmonary dysplasia CVP line insertion Introduction Pulmonary infarct Jet ventilation Pulmonary metastases Liver biopsy In a seriously ill patient or the victim of multiple trauma Pulmonoalveolar proteinosis Lung biopsy the clinical symptoms and signs of a pneumothorax may Radiation pneumonitis Oesophageal instrumentation be overshadowed by other problems. Usually in these Sarcoid PEEP ventilation circumstances a chest X-ray will be taken at the bedside Staphylococcal septicaemia Pleural aspiration with the patient supine and the appearances of a Tuberculosis Pleural biopsy pneumothorax will be different from those seen when the Tuberose sclerosis patient is upright. -
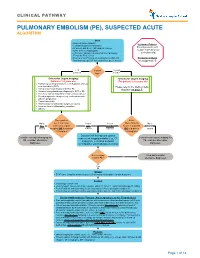
Pulmonary Embolism (Pe), Suspected Acute Algorithm
CLINICAL PATHWAY PULMONARY EMBOLISM (PE), SUSPECTED ACUTE ALGORITHM Start · Room air pulse oximetry Inclusion Criteria: · Consider supplemental oxygen · IV access and STAT CBC and DIC screen Patient presents with · Urine β-HCG, if appropriate suspected Pulmonary · CXR (PA + lateral), EKG and call the Cardiology Embolism (PE) Fellow for Echo review · Review criteria* for urgent imaging for possible PE Exclusion Criteria based on age-specific risk factors (see green boxes) No suspected PE < 18 Patient 18 years years old age? or older *Criteria for Urgent Imaging: *Criteria for Urgent Imaging: Patients < 18 years old For patients ≥ 18 years old · Painful leg swelling or known recent diagnosis of deep vein thrombosis (DVT) Please refer to the Wells Criteria · Family or personal history of DVT or PE Algorithm on page 7. · Known clotting disorder predisposing to DVT or PE · Recent or current indwelling central venous catheter · Elevated systemic estrogen (e.g., oral contraceptive pill use, pregnancy) · Recent immobility · Recent major or orthopedic surgery or trauma · Acute or chronic inflammatory condition · Obesity Does patient Is the No to meet 1 or more Yes to Yes to Wells Criteria No to ALL criteria for urgent ANY EITHER Score > 4 points BOTH criteria imaging OR is d-dimer criteria criterion OR is d-dimer criteria > 0.5ug/mL? > 0.5ug/mL? Discuss CXR findings and optimal Consider non-urgent imaging for subsequent imaging modality (e.g., CT Consider non-urgent imaging for PE, consider alternative angiogram, ventilation perfusion PE, consider -

CHEST RADIOLOGY: Goals and Objectives
Harlem Hospital Center Department of Radiology Residency Training Program CHEST RADIOLOGY: Goals and Objectives ROTATION 1 (Radiology Years 1): Resident responsibilities: • ED chest CTs • Inpatient and outpatient plain films including the portable intensive care unit radiographs • Consultations with referring clinicians MEDICAL KNOWLEDGE: • Residents must demonstrate knowledge about established and evolving biomedical, clinical, and cognitive sciences and the application of this knowledge to patient care. At the end of the rotation, the resident should be able to: • Identify normal radiographic and CT anatomy of the chest • Identify and describe common variants of normal, including aging changes. • Demonstrate a basic knowledge of radiographic interpretation of atelectasis, pulmonary infection, congestive heart failure, pleural effusion and common neoplastic diseases of the chest • Identify the common radiologic manifestation of thoracic trauma, including widened mediastinum, signs of aortic laceration, pulmonary contusion/laceration, esophageal and diaphragmatic rupture. • Know the expected postoperative appearance in patients s/p thoracic surgery and the expected location of the life support and monitoring devices on chest radiographs of critically ill patients (intensive care radiology); be able to recognize malpositioned devices. • Identify cardiac enlargement and know the radiographic appearance of the dilated right vs. left atria and right vs. left ventricles, and pulmonary vascular congestion • Recognize common life-threatening -

成人のstridorへの アプローチ 筑波大学総合診療グループ 細井崇弘 監修 筑波大学総合診療グループ 五十野博基 2017年3月9日
成人のstridorへの アプローチ 筑波大学総合診療グループ 細井崇弘 監修 筑波大学総合診療グループ 五十野博基 2017年3月9日 分野:呼吸器 テーマ:診断 症例78歳女性 主訴 呼吸困難 当院は医療過疎地にある100床程度の小規模病院。 【現病歴】高血圧、糖尿病で近医通院中。入院数日前から咳嗽がみら れていた。入院当日に近医を受診し、胸部レントゲン検査を受け肺炎 の疑いと診断され帰宅した。 20時近くまでは同居の娘が異常が無い事を確認。 24時頃に娘が帰宅すると、獣の鳴くような声が聞こえ、患者のもとに 駆け付けると呼吸苦を訴えており、救急車を要請し当院へ搬送された。 【既往歴】高血圧、糖尿病。喘息無し。 【喫煙歴】なし 入院時現症 来院時、自発開眼しているが、会話困難。 Vital sign:BP 145/90mmHg, HR 130/min, RR36/min,SpO2 86%, BT 38℃ 頸部 Stridorを聴取 BVMによる呼吸補助開始するも換気不良 上気道閉塞と判断し、7mmチューブで経口気管挿管 このとき喉頭蓋の浮腫(-) BGA(Vein):pH 7.08, PaO2 63Torr, PCO2 99.9 Torr 胸部所見では両側に軽度の coarse cracklesあり 腹部所見は異常なし 症例の経過 • インフルエンザA(+) • 呼吸器管理となり入院、ラピアクタ投与と鎮痛・鎮静 • CO2ナルコーシスは改善、耳鼻科と共に喉頭ファイバーで声門より 上部に狭窄病変が無い事を確認。 • 意識レベルも清明であり従命可能、自発呼吸も良好であり抜管 抜管後は発語もあり問題なかったが、10数分で呼吸困難を訴え、 SpO2が急激に低下したため再挿管。 再挿管時、声帯は確認できたがチューブが声帯を越えるのに非常に 難渋した。 Stridorは何が原因だったのか? 抜管による喉頭浮腫? では救急外来に来た際の最初のStridorは? Stridorが聞こえたが喉頭蓋炎ではなかったとき、 どのような鑑別疾患を上げ、 どのようにアプローチするのが良かったのか? Clinical Ques3on • 成人で気道狭窄が疑われる場合 ①鑑別診断は何か? ②初期診断のためのアプローチは? Stridorとは~身体診察~ • 強い楽音様の音で、明確な一定の音調(一般に400Hz前後)であり、 通過障害(閉塞)を示唆する。 ・Stridorは吸気時に限られる ・Stridorは常に頸部でより強く聴取されるが、wheezingは常に胸部で 聴取される。Am Rev Respir Dis.1983;143:890-892 ・気道の直径が8㎜以下になると労作時呼吸困難が出現し、 Crit Care Med 2004; 169: 1278-1297. ・気道の直系が5mm以下で安静時にも呼吸苦が出現する。 JAMA.1971;216:1984-1985 気道狭窄の分類 upper airway obstrucYon(UAO) Central airway obstrucYon(CAO) Lower airway obstrucYon(LAO) 口から(鼻腔含め)喉頭. 慢性的な閉塞性肺傷害、喘息や : :気管および主気管支 : CAOと同時に認められることも COPDなど。CAOやUAOとは典型 的には合併しない。 発症率などの疫学については、 (悪性腫瘍以外の例では) 成人での発生頻度が非常にまれであり、 詳しくは分かっていない。 Up to date: Clinical presentaon , diagnosYc evaluaon,and management of -

Deep Sulcus Sign Developed in Patient with Multiple Fibrous Bands Between the Parietal and Visceral Pleura
eISSN: 2508-8033 Brief Image in Trauma pISSN: 2508-5298 Deep Sulcus Sign Developed in Patient with Multiple Fibrous Bands between the Parietal and Visceral Pleura Chan Yong Park1, Kwang Hee Yeo1, Sung Jin Park1, Ho Hyun Kim1, Chan Kyu Lee1, Seon Hee Kim1, Hyun Min Cho1, Seok Ran Yeom2 1Department of Trauma Surgery, Pusan National University Hospital, Busan, Korea 2Department of Emergency Medicine, Pusan National University Hospital, Busan, Korea A deepening of the costophrenic angle occurs in cases with a deep sulcus sign. We report a case of deep sulcus sign in a 47-year-old man who fell from the fifth floor. Supine chest radiography showed a right-sided pneumothorax with deep sulcus sign. Chest computed tomography (CT) demonstrated a large pneumothorax with multiple fibrous bands between the parietal and visceral pleura of the upper lobe of the right lung. (Trauma Image Proced 2017(1):7-9) Key Words: Pneumothorax; X-Rays; Diagnosis; Tomography, X-Ray computed CASE A 47-year-old man presented to the emergency department after falling from a fifth floor height. His vital signs were systolic blood pressure 60 mmHg, pulse rate 111 beats/min, respiration rate 31 breaths/min, body temperature, 36.4℃, and oxygen saturation 96%. The injury severity score was 29, revised trauma score 5.15, trauma and injury severity score 74.8%. His arterial blood gas analysis was pH 7.35, pCO2 29 mmHg, pO2 75 mmHg, hemoglobin 16.7, SaO2 94%, lactic acid 11.8 mmol/L, and base excess -8.0. Supine chest radiography showed a right-sided pneumothorax with a deep sulcus Fig. -

Chapter 17 Dyspnea Sabina Braithwaite and Debra Perina
Chapter 17 Dyspnea Sabina Braithwaite and Debra Perina ■ PERSPECTIVE Pathophysiology Dyspnea is the term applied to the sensation of breathlessness The actual mechanisms responsible for dyspnea are unknown. and the patient’s reaction to that sensation. It is an uncomfort- Normal breathing is controlled both centrally by the respira- able awareness of breathing difficulties that in the extreme tory control center in the medulla oblongata, as well as periph- manifests as “air hunger.” Dyspnea is often ill defined by erally by chemoreceptors located near the carotid bodies, and patients, who may describe the feeling as shortness of breath, mechanoreceptors in the diaphragm and skeletal muscles.3 chest tightness, or difficulty breathing. Dyspnea results Any imbalance between these sites is perceived as dyspnea. from a variety of conditions, ranging from nonurgent to life- This imbalance generally results from ventilatory demand threatening. Neither the clinical severity nor the patient’s per- being greater than capacity.4 ception correlates well with the seriousness of underlying The perception and sensation of dyspnea are believed to pathology and may be affected by emotions, behavioral and occur by one or more of the following mechanisms: increased cultural influences, and external stimuli.1,2 work of breathing, such as the increased lung resistance or The following terms may be used in the assessment of the decreased compliance that occurs with asthma or chronic dyspneic patient: obstructive pulmonary disease (COPD), or increased respira- tory drive, such as results from severe hypoxemia, acidosis, or Tachypnea: A respiratory rate greater than normal. Normal rates centrally acting stimuli (toxins, central nervous system events).