Pleural Effusion, Hypovascularity in Lung Zone (Westermark’S Sign) & Pyramid Shape Infiltrate with Peak Directed to Hilus (Hampton’S Hump)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

X-Ray Interpretation
Objectives Describe a systematic method for interpretation of chest and abdomen x-rays List findings to accurately identify common X-ray Interpretation pathology in chest & abdomen x-rays Describe a systematic method to approach the Denise Ramponi, DNP, FNP-C, ENP-BC, FAANP, FAEN important components in interpretation of upper & lower extremity x-rays Chest X-ray: Standard Views Lateral Film Postero-anterior (PA): (LAT) view can determine th On inspiration – diaphragm descends to 10 rib the anterior-posterior posteriorly structures along the axis of the body Normal LAT film Counting Ribs AP View - Portable http://www.lumen.luc.edu/lumen/MedEd/medicine/pulmonar/cxr/cxr_f.htm When the patient is unable to tolerate routine views with pts sitting or supine No participation from the patient Film is against the patient's back (supine) 1 Consolidation, Atelectasis, Chest radiograph Interstitial involvement Consolidation - any pathologic process that fills the alveoli with Left and right heart fluid, pus, blood, cells or other borders well defined substances Interstitial - involvement of the Both hemidiaphragms supporting tissue of the lung visible to midline parenchyma resulting in fine or coarse reticular opacities Right - higher Atelectasis - collapse of a part of Heart less than 50% of the lung due to a decrease in the amount of air resulting in volume diameter of the chest loss and increased density. Infiltrate, Consolidation vs. Congestive Heart Failure Atelectasis Fluid leaking into interstitium Kerley B 2 Kerley B lines Prominent interstitial markings Kerley lines Magnified CXR Cardiomyopathy & interstitial pulmonary edema Short 1-2 cm white lines at lung periphery horizontal to pleural surface Distended interlobular septa - secondary to interstitial edema. -

Diagnosing Pulmonary Embolism M Riedel
309 Postgrad Med J: first published as 10.1136/pgmj.2003.007955 on 10 June 2004. Downloaded from REVIEW Diagnosing pulmonary embolism M Riedel ............................................................................................................................... Postgrad Med J 2004;80:309–319. doi: 10.1136/pgmj.2003.007955 Objective testing for pulmonary embolism is necessary, embolism have a low long term risk of subse- quent VTE.2 5–7 because clinical assessment alone is unreliable and the consequences of misdiagnosis are serious. No single test RISK FACTORS AND RISK has ideal properties (100% sensitivity and specificity, no STRATIFICATION risk, low cost). Pulmonary angiography is regarded as the The factors predisposing to VTE broadly fit Virchow’s triad of venous stasis, injury to the final arbiter but is ill suited for diagnosing a disease vein wall, and enhanced coagulability of the present in only a third of patients in whom it is suspected. blood (box 1). The identification of risk factors Some tests are good for confirmation and some for aids clinical diagnosis of VTE and guides decisions about repeat testing in borderline exclusion of embolism; others are able to do both but are cases. Primary ‘‘thrombophilic’’ abnormalities often non-diagnostic. For optimal efficiency, choice of the need to interact with acquired risk factors before initial test should be guided by clinical assessment of the thrombosis occurs; they are usually discovered after the thromboembolic event. Therefore, the likelihood of embolism and by patient characteristics that risk of VTE is best assessed by recognising the may influence test accuracy. Standardised clinical presence of known ‘‘clinical’’ risk factors. estimates can be used to give a pre-test probability to However, investigations for thrombophilic dis- orders at follow up should be considered in those assess, after appropriate objective testing, the post-test without another apparent explanation. -
Cardiothoracic Fellowship Program
Cardiothoracic Fellowship Program Table of Contents Program Contact ............................................................................................ 3 Other contact numbers .................................................................................. 4 Introduction ........................................................................................................... 5 Goals and Objectives of Fellowship: ..................................................................... 6 Rotation Schedule: ........................................................................................ 7 Core Curriculum .................................................................................................... 8 Fellow’s Responsibilities ..................................................................................... 22 Resources ........................................................................................................... 23 Facilities ....................................................................................................... 23 Educational Program .......................................................................................... 26 Duty Hours .......................................................................................................... 29 Evaluation ........................................................................................................... 30 Table of Appendices .................................................................................... 31 Appendix A -

12. Shortness of Breath
12. Shortness of breath Shortness of breath (dyspnea) is described as an intense tightening in the chest, air hunger, difficulty breathing, breathlessness or a feeling of suffocation. It is a subjective symptom of many diseases. The causes of shortness of breath can be various, but most often pulmonary or cardiac. The main causes of pulmonary or cardiac dyspnea include heart congestion, pulmonary embolism, emphysema, atelectasis, pneumothorax and interstitial lung processes. The basic imaging method in the diagnosis of dyspnea that follows clinical examination is a chest X- ray. It is used to evaluate heart congestion, fluid effusions, atelectasis, pneumothorax, and a rough assessment of interstitial lung processes. Only if there is a clinical suspicion of pulmonary embolization, the CT angiography (with intravenous contrast), perfusion lung scintigraphy or echocardiography are imaging methods of choice. If interstitial lung disease or pulmonary emphysema are suspected or there is uncertain finding on chest X-ray, high-resolution CT (HRCT) of the chest is recommended. HRCT allows detailed assessment of pulmonary parenchyma. Non-contrast CT is usually sufficient to assess interstitial changes. Heart congestion Heart congestion is the result of insufficient cardiac output due to heart failure or fluid overload. The most common cause of heart congestion is left heart failure with increased pressure in pulmonary veins and capillaries. On chest X- ray can be distinguished 3 degrees of heart congestion. Note: Right-sided heart failure most often occurs in long-term left-sided heart failure or lung disease, which leads to high pulmonary artery resistance (various etiologies of pulmonary hypertension, e.g. advanced COPD). -

Interstitial Lung Disease
Interstitial Lung Disease Camille Washowich, MSN, ACNP, CCRN Center for Advanced Lung Disease Stanford University Medical Center Lung Physiology ILD Classification Interstitial Lung Disease Connective Tissue Diseases Primary (unclassified) Idiopathic Fibrotic Disorders Drug and Treatment Induced Connective Tissue Diseases Scleroderma Systemic Lupus Erythematous (SLE) Rheumatoid Arthritis Mixed Connective Tissue Disease Primary (unclassified) Sarcoidosis Stage I-IV Neurofibromatosis Tuberous Sclerosis AIDS ARDS Bone Marrow Transplantation Post infectious Occupational & Environmental Exposures: Inorganic & Organic Agriculture Workers and Animal Handlers Construction: wood/metal Auto repair Military Chemicals (plastic, paint, polyurethane) Organisms: fungus/molds/bacterium Idiopathic Fibrotic Disorders Pulmonary fibrosis Familial pulmonary fibrosis Autoimmune pulmonary fibrosis Respiratory bronchiolitis Nonspecific interstitial pneumonitis (NSIP) Drug Induced Antibiotics Anti-arrhythmics Anti-inflammatory Anti-convulsant Radiation/Chemotherapy Oxygen toxicity Narcotics ILD Epidemiology in the US 100K admissions/year Occupation DILD Sarcoidosis 11% 15% pulmonologist patients 5% DAH 8% 4% CTD Incidence: 5/100K 9% Men (31%) versus Women (26%) Other 11% IPF 45% of all ILD patients Pulmonary Fibrosis 52% Age/Gender/Race Specifications to Assist in Diagnosis 20-40yrs: Inherited Interstitial Lung diseases Familial idiopathic pulmonary fibrosis Collagen vascular disease- associated ILD LAM Pulmonary Langerhans’ cell granulomatosis Sarcoidosis 50yrs: -
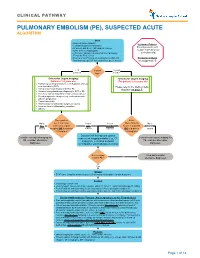
Pulmonary Embolism (Pe), Suspected Acute Algorithm
CLINICAL PATHWAY PULMONARY EMBOLISM (PE), SUSPECTED ACUTE ALGORITHM Start · Room air pulse oximetry Inclusion Criteria: · Consider supplemental oxygen · IV access and STAT CBC and DIC screen Patient presents with · Urine β-HCG, if appropriate suspected Pulmonary · CXR (PA + lateral), EKG and call the Cardiology Embolism (PE) Fellow for Echo review · Review criteria* for urgent imaging for possible PE Exclusion Criteria based on age-specific risk factors (see green boxes) No suspected PE < 18 Patient 18 years years old age? or older *Criteria for Urgent Imaging: *Criteria for Urgent Imaging: Patients < 18 years old For patients ≥ 18 years old · Painful leg swelling or known recent diagnosis of deep vein thrombosis (DVT) Please refer to the Wells Criteria · Family or personal history of DVT or PE Algorithm on page 7. · Known clotting disorder predisposing to DVT or PE · Recent or current indwelling central venous catheter · Elevated systemic estrogen (e.g., oral contraceptive pill use, pregnancy) · Recent immobility · Recent major or orthopedic surgery or trauma · Acute or chronic inflammatory condition · Obesity Does patient Is the No to meet 1 or more Yes to Yes to Wells Criteria No to ALL criteria for urgent ANY EITHER Score > 4 points BOTH criteria imaging OR is d-dimer criteria criterion OR is d-dimer criteria > 0.5ug/mL? > 0.5ug/mL? Discuss CXR findings and optimal Consider non-urgent imaging for subsequent imaging modality (e.g., CT Consider non-urgent imaging for PE, consider alternative angiogram, ventilation perfusion PE, consider -

CHEST RADIOLOGY: Goals and Objectives
Harlem Hospital Center Department of Radiology Residency Training Program CHEST RADIOLOGY: Goals and Objectives ROTATION 1 (Radiology Years 1): Resident responsibilities: • ED chest CTs • Inpatient and outpatient plain films including the portable intensive care unit radiographs • Consultations with referring clinicians MEDICAL KNOWLEDGE: • Residents must demonstrate knowledge about established and evolving biomedical, clinical, and cognitive sciences and the application of this knowledge to patient care. At the end of the rotation, the resident should be able to: • Identify normal radiographic and CT anatomy of the chest • Identify and describe common variants of normal, including aging changes. • Demonstrate a basic knowledge of radiographic interpretation of atelectasis, pulmonary infection, congestive heart failure, pleural effusion and common neoplastic diseases of the chest • Identify the common radiologic manifestation of thoracic trauma, including widened mediastinum, signs of aortic laceration, pulmonary contusion/laceration, esophageal and diaphragmatic rupture. • Know the expected postoperative appearance in patients s/p thoracic surgery and the expected location of the life support and monitoring devices on chest radiographs of critically ill patients (intensive care radiology); be able to recognize malpositioned devices. • Identify cardiac enlargement and know the radiographic appearance of the dilated right vs. left atria and right vs. left ventricles, and pulmonary vascular congestion • Recognize common life-threatening -

Chest Radiology: a Resident's Manual
Chest Radiology: A Resident's Manual Bearbeitet von Johannes Kirchner 1. Auflage 2011. Buch. 300 S. Hardcover ISBN 978 3 13 153871 0 Format (B x L): 23 x 31 cm Weitere Fachgebiete > Medizin > Sonstige Medizinische Fachgebiete > Radiologie, Bildgebende Verfahren Zu Inhaltsverzeichnis schnell und portofrei erhältlich bei Die Online-Fachbuchhandlung beck-shop.de ist spezialisiert auf Fachbücher, insbesondere Recht, Steuern und Wirtschaft. Im Sortiment finden Sie alle Medien (Bücher, Zeitschriften, CDs, eBooks, etc.) aller Verlage. Ergänzt wird das Programm durch Services wie Neuerscheinungsdienst oder Zusammenstellungen von Büchern zu Sonderpreisen. Der Shop führt mehr als 8 Millionen Produkte. 1 Heart Failure Acute left heart failure is most commonly caused by a hyperten- " Compare pulmonary vessels that are equidistant to a central sive crisis. Radiographic signs on the plain chest radiograph ob- point in the respective hilum. tained with the patient standing include: " Compare the diameter of a random easily identifiable superior " Redistribution of pulmonary perfusion lobe artery (often the anterior segmental artery is most easily " Presence of interstitial patterns (Kerley lines, peribronchial identifiable) with the diameter of the corresponding ipsilateral cuffing) bronchus (Fig. 1.62). " Alveolar densities with indistinct vascular structures (ad- vanced stage) As the pulmonary artery and corresponding ipsilateral bronchus " Pleural effusions are normally of precisely equal diameter, a larger arterial diameter is indicative of redistribution of perfusion (Fig. 1.63). The diagnos- All of these signs are essentially attributable to increased fluid tic criteria of caudal-to-cranial redistribution cannot be evaluated content in the abnormally heavy “wet” lung. The fluid accumula- on radiographs obtained in the supine patient. -

Chapter 17 Dyspnea Sabina Braithwaite and Debra Perina
Chapter 17 Dyspnea Sabina Braithwaite and Debra Perina ■ PERSPECTIVE Pathophysiology Dyspnea is the term applied to the sensation of breathlessness The actual mechanisms responsible for dyspnea are unknown. and the patient’s reaction to that sensation. It is an uncomfort- Normal breathing is controlled both centrally by the respira- able awareness of breathing difficulties that in the extreme tory control center in the medulla oblongata, as well as periph- manifests as “air hunger.” Dyspnea is often ill defined by erally by chemoreceptors located near the carotid bodies, and patients, who may describe the feeling as shortness of breath, mechanoreceptors in the diaphragm and skeletal muscles.3 chest tightness, or difficulty breathing. Dyspnea results Any imbalance between these sites is perceived as dyspnea. from a variety of conditions, ranging from nonurgent to life- This imbalance generally results from ventilatory demand threatening. Neither the clinical severity nor the patient’s per- being greater than capacity.4 ception correlates well with the seriousness of underlying The perception and sensation of dyspnea are believed to pathology and may be affected by emotions, behavioral and occur by one or more of the following mechanisms: increased cultural influences, and external stimuli.1,2 work of breathing, such as the increased lung resistance or The following terms may be used in the assessment of the decreased compliance that occurs with asthma or chronic dyspneic patient: obstructive pulmonary disease (COPD), or increased respira- tory drive, such as results from severe hypoxemia, acidosis, or Tachypnea: A respiratory rate greater than normal. Normal rates centrally acting stimuli (toxins, central nervous system events). -

Mayo Clinic Medical Manual This Page Intentionally Left Blank Mayo Clinic Medical Manual
Mayo Clinic Medical Manual This page intentionally left blank Mayo Clinic Medical Manual Editors Guilherme H. M. Oliveira, M.D. Gillian C. Nesbitt, M.D. Joseph G. Murphy, M.D. MAYO CLINIC SCIENTIFIC PRESS TAYLOR & FRANCIS GROUP ISBN 0849390877 The triple-shield Mayo logo and the words MAYO, MAYO CLINIC, and MAYO CLINIC SCIENTIFIC PRESS are marks of Mayo Foundation for Medical Education and Research. ©2006 by Mayo Foundation for Medical Education and Research. All rights reserved. This book is protected by copyright. No part of it may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means—electronic, mechanical, photocopying, record- ing, or otherwise—without the prior written consent of the copyright holder, except for brief quotations embodied in critical articles and reviews. Inquiries should be addressed to Scientific Publications, Plummer 10, Mayo Clinic, 200 First Street SW, Rochester, MN 55905. For order inquiries, contact Taylor & Francis Group, 6000 Broken Sound Parkway NW, Suite #300, Boca Raton, FL 33487. www.taylorandfrancis.com Catalog record is available from the Library of Congress. Care has been taken to confirm the accuracy of the information presented and to describe generally accepted practices. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this book and make no warranty, express or implied, with respect to the contents of the publication. This book should not be relied on apart from the advice of a qualified health care provider. The authors, editors, and publisher have exerted efforts to ensure that drug selection and dosage set forth in this text are in accordance with current recommendations and practice at the time of publication. -

Pneumonia (CAP)
肺實質化病變與肺塌陷 胸腔內科周百謙醫師 Dr. Pai-chien Chou MD PhD Department of Thoracic Medicine Taipei Medical University Hospital Chest X-ray • P-A view • Lateral view • Oblique view • Lordotic view • Expiratory film • Decubitus view • Overpenetrated grid film The Elements of a chest x-ray (CXR) • The Broncho-vascular markings in the lung • The borders of the heart • The contours of the mediastinum and pleural space • The ribs and spine Segmental anatomy Segmental Anatomy Cardiomediastinal outlines on Chest X-ray Density of image ◆ Gas ◆ Water ◆ Fat ◆ Metal and bone ◆ Thinking of pathogenesis Basic thinking of a lesion on Chest X-ray ◆ Size ◆ Location (Silhouette sign) – Anterior, posterior – Which lobe is involved ◆ Intrapulmonary (Air bronchogram sign) ◆ Extrapulmonary (Incomplete border sign) Infiltrate in the lungs • Fluid accumulates in lung, predominate in the alveolar (airspace) compartment or the interstitial compartment. interstitial compartment Lymphatic compartment Alveolar unit Vascular unit Air space opacification The opacification is caused by fluid or solid material within the airways that causes a difference in the relative attenuation of the lung: • transudate, e.g. pulmonary edema secondary to heart failure • pus, e.g. bacterial pneumonia • blood, e.g. pulmonary hemorrhage • cells, e.g. bronchoalveolar carcinoma • protein, e.g. alveolar proteinosis • fat, e.g. lipoid pneumonia • gastric contents, e.g. aspiration pneumonia • water, e.g. drowning When considering the likely causes of airspace opacification, it is useful to determine chronicity -

Signs in Chest Imaging
Diagn Interv Radiol 2011; 17:18–29 CHEST IMAGING © Turkish Society of Radiology 2011 PICTORIAL ESSAY Signs in chest imaging Oktay Algın, Gökhan Gökalp, Uğur Topal ABSTRACT adiological practice includes classification of illnesses with similar A radiological sign can sometimes resemble a particular object characteristics through recognizable signs. Knowledge of and abil- or pattern and is often highly suggestive of a group of similar pathologies. Awareness of such similarities can shorten the dif- R ity to recognize these signs can aid the physician in shortening ferential diagnosis list. Many such signs have been described the differential diagnosis list and deciding on the ultimate diagnosis for for X-ray and computed tomography (CT) images. In this ar- ticle, we present the most frequently encountered plain film a patient. In this report, 23 important and frequently seen radiological and CT signs in chest imaging. These signs include for plain signs are presented and described using chest X-rays, computed tomog- films the air bronchogram sign, silhouette sign, deep sulcus raphy (CT) images, illustrations and photographs. sign, Continuous diaphragm sign, air crescent (“meniscus”) sign, Golden S sign, cervicothoracic sign, Luftsichel sign, scim- itar sign, doughnut sign, Hampton hump sign, Westermark Plain films sign, and juxtaphrenic peak sign, and for CT the gloved finger Air bronchogram sign sign, CT halo sign, signet ring sign, comet tail sign, CT an- giogram sign, crazy paving pattern, tree-in-bud sign, feeding Bronchi, which are not normally seen, become visible as a result of vessel sign, split pleura sign, and reversed halo sign. opacification of the lung parenchyma.