Chapter 17 Dyspnea Sabina Braithwaite and Debra Perina
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diagnosing Pulmonary Embolism M Riedel
309 Postgrad Med J: first published as 10.1136/pgmj.2003.007955 on 10 June 2004. Downloaded from REVIEW Diagnosing pulmonary embolism M Riedel ............................................................................................................................... Postgrad Med J 2004;80:309–319. doi: 10.1136/pgmj.2003.007955 Objective testing for pulmonary embolism is necessary, embolism have a low long term risk of subse- quent VTE.2 5–7 because clinical assessment alone is unreliable and the consequences of misdiagnosis are serious. No single test RISK FACTORS AND RISK has ideal properties (100% sensitivity and specificity, no STRATIFICATION risk, low cost). Pulmonary angiography is regarded as the The factors predisposing to VTE broadly fit Virchow’s triad of venous stasis, injury to the final arbiter but is ill suited for diagnosing a disease vein wall, and enhanced coagulability of the present in only a third of patients in whom it is suspected. blood (box 1). The identification of risk factors Some tests are good for confirmation and some for aids clinical diagnosis of VTE and guides decisions about repeat testing in borderline exclusion of embolism; others are able to do both but are cases. Primary ‘‘thrombophilic’’ abnormalities often non-diagnostic. For optimal efficiency, choice of the need to interact with acquired risk factors before initial test should be guided by clinical assessment of the thrombosis occurs; they are usually discovered after the thromboembolic event. Therefore, the likelihood of embolism and by patient characteristics that risk of VTE is best assessed by recognising the may influence test accuracy. Standardised clinical presence of known ‘‘clinical’’ risk factors. estimates can be used to give a pre-test probability to However, investigations for thrombophilic dis- orders at follow up should be considered in those assess, after appropriate objective testing, the post-test without another apparent explanation. -

Noninvasive Positive Pressure Ventilation in the Home
Technology Assessment Program Noninvasive Positive Pressure Ventilation in the Home Final Technology Assessment Project ID: PULT0717 2/4/2020 Technology Assessment Program Project ID: PULT0717 Noninvasive Positive Pressure Ventilation in the Home (with addendum) Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov Contract No: HHSA290201500013I_HHSA29032004T Prepared by: Mayo Clinic Evidence-based Practice Center Rochester, MN Investigators: Michael Wilson, M.D. Zhen Wang, Ph.D. Claudia C. Dobler, M.D., Ph.D Allison S. Morrow, B.A. Bradley Beuschel, B.S.P.H. Mouaz Alsawas, M.D., M.Sc. Raed Benkhadra, M.D. Mohamed Seisa, M.D. Aniket Mittal, M.D. Manuel Sanchez, M.D. Lubna Daraz, Ph.D Steven Holets, R.R.T. M. Hassan Murad, M.D., M.P.H. Key Messages Purpose of review To evaluate home noninvasive positive pressure ventilation (NIPPV) in adults with chronic respiratory failure in terms of initiation, continuation, effectiveness, adverse events, equipment parameters and required respiratory services. Devices evaluated were home mechanical ventilators (HMV), bi-level positive airway pressure (BPAP) devices, and continuous positive airway pressure (CPAP) devices. Key messages • In patients with COPD, home NIPPV as delivered by a BPAP device (compared to no device) was associated with lower mortality, intubations, hospital admissions, but no change in quality of life (low to moderate SOE). NIPPV as delivered by a HMV device (compared individually with BPAP, CPAP, or no device) was associated with fewer hospital admissions (low SOE). In patients with thoracic restrictive diseases, HMV (compared to no device) was associated with lower mortality (low SOE). -

Acute Chest Syndrome in Sickle Cell Disease Care Guideline
Acute Chest Syndrome in Sickle Cell Disease Care Guideline Inclusion Criteria: · Children with sickle cell disease Recommendations/ · New pulmonary infiltrate on CXR, involving at least one Considerations complete lung segment, excluding atelectasis Predictors: · Pain crisis involving chest, shoulders Assessment and back · Admit to 5S or PICU · Post anesthesia complication · NPO · Respiratory Infections · History and physical with focus on pulmonary exam · On narcotics · Vitals, accurate height and weight · Asthma exacerbation · Strict I/O; Daily Weight · O2 saturation · Baseline Hgb level may run low < · Diagnostics: 9gm/dl CBC with retic, CMP with LDH, STAT type and screen, Hgb electrophoresis · If suspected pulmonary embolism, · Consider VBG for significant respiratory distress obtain CT angiogram of chest · CXR 2 view · Blood culture if fever >38, elevated WBC · May need more than 1 exchange · VRP if URI symptoms transfusion if clinical findings not improving Interventions · After recovery from acute crisis, pt · Stat Hematology consult (if not admitted to Hematology service) should be started on hydroxyurea if · Pulmonary consult not already taking; optimize dose · Notify apheresis team as soon as possible during working hours if anticipated procedure · History of more than 1 acute chest · Consult PICU for possible apheresis catheter placement crisis, consider chronic transfusion · Oxygen to keep O2 sat >=94% protocols to keep HgbS < 25% · Maintenance IV fluids · Antibiotics: ceftriaxone and azithromycin · If recurrent crises, consider -

The Effects of Inhaled Albuterol in Transient Tachypnea of the Newborn Myo-Jing Kim,1 Jae-Ho Yoo,1 Jin-A Jung,1 Shin-Yun Byun2*
Original Article Allergy Asthma Immunol Res. 2014 March;6(2):126-130. http://dx.doi.org/10.4168/aair.2014.6.2.126 pISSN 2092-7355 • eISSN 2092-7363 The Effects of Inhaled Albuterol in Transient Tachypnea of the Newborn Myo-Jing Kim,1 Jae-Ho Yoo,1 Jin-A Jung,1 Shin-Yun Byun2* 1Department of Pediatrics, Dong-A University, College of Medicine, Busan, Korea 2Department of Pediatrics, Pusan National University School of Medicine, Yangsan, Korea This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. Purpose: Transient tachypnea of the newborn (TTN) is a disorder caused by the delayed clearance of fetal alveolar fluid.ß -adrenergic agonists such as albuterol (salbutamol) are known to catalyze lung fluid absorption. This study examined whether inhalational salbutamol therapy could improve clinical symptoms in TTN. Additional endpoints included the diagnostic and therapeutic efficacy of salbutamol as well as its overall safety. Methods: From January 2010 through December 2010, we conducted a prospective study of 40 newborns hospitalized with TTN in the neonatal intensive care unit. Patients were given either inhalational salbutamol (28 patients) or placebo (12 patients), and clinical indices were compared. Results: The dura- tion of tachypnea was shorter in patients receiving inhalational salbutamol therapy, although this difference was not statistically significant. The dura- tion of supplemental oxygen therapy and the duration of empiric antibiotic treatment were significantly shorter in the salbutamol-treated group. -

Acute Chest Syndrome
CLINICAL PATHWAY PEDIATRIC ACUTE CHEST SYNDROME (ACS) Patients with sickle cell disease presenting with 1) a new pulmonary infiltrate on chest radiography AND 2) evidence of lower airway disease (e.g. cough, shortness of breath, retractions, rales, etc.) TABLE OF CONTENTS Algorithm- N/A Target Population Background | Definitions Initial Evaluation-N/A Clinical Management Diagnostic Tests Fluids | Nutrition Respiratory Therapy Table 1. Pediatric Asthma Score Treatment Table 2. Antimicrobial Medication Table 3. Pain Medication Table 4. Respiratory Medication Discharge Criteria Related Children’s Hospital Colorado Documents References Clinical Improvement Team TARGET POPULATION Inclusion Criteria • Patients with sickle cell disease (SS, SC, Sβ0 thalassemia, Sβ+ thalassemia) • Patients of all ages • Patients treated year round Exclusion Criteria • Patients without infiltrate on chest radiograph (e.g. asthma exacerbation) • Patients with severe pulmonary hypertension • Patients post bone marrow transplant • Well children with pneumonia Page 1 of 10 CLINICAL PATHWAY BACKGROUND | DEFINITIONS Acute chest syndrome (ACS) is the second most common reason for hospitalization in children with sickle cell disease and a leading cause of mortality. ACS is defined as a new pulmonary infiltrate on chest radiograph in the presence of evidence of lower respiratory tract disease (e.g. some combination of cough, shortness of breath, retractions, rales, etc.). In the majority of cases of ACS, an etiology is unable to be identified. The most common identified etiology of ACS is infection but it may also result from pulmonary vaso-occlusion, pulmonary infarction or fat embolism. The primary infectious agents implicated in ACS include: Chlamydia pneumoniae, Mycoplasma pneumoniae, Streptococcus pneumoniae, and viruses. Risk factors for ACS include vaso-occlusive pain crisis, anesthesia, and surgery. -

Changes Seen on Computed Tomography of the Chest In
Alves UD et al.Original / CT of the Article chest in sickle cell disease Changes seen on computed tomography of the chest in mildly symptomatic adult patients with sickle cell disease* Alterações na tomografia computadorizada do tórax em pacientes adultos oligossintomáticos com doença falciforme Ursula David Alves1, Agnaldo José Lopes2, Maria Christina Paixão Maioli3, Andrea Ribeiro Soares3, Pedro Lopes de Melo4, Roberto Mogami5 Alves UD, Lopes AJ, Maioli MCP, Soares AR, Melo PL, Mogami R. Changes seen on computed tomography of the chest in mildly symptomatic adult patients with sickle cell disease. Radiol Bras. 2016 Jul/Ago;49(4):214–219. Abstract Objective: To describe and quantify the main changes seen on computed tomography of the chest in mildly symptomatic adult patients with sickle cell disease, as well as to evaluate the radiologist accuracy in determining the type of hemoglobinopathy. Materials and Methods: A prospective study involving 44 adult patients with sickle cell disease who underwent inspiration and expiration computed tomography of the chest. The frequency of tomography findings and the extent of involvement are reported. We also calculated radiologist accuracy in determining the type of hemoglobinopathy by analyzing the pulmonary alterations and morphology of the spleen. Results: The changes found on computed tomography scans, in descending order of frequency, were as follows: fibrotic opacities (81.8%); mosaic attenuation (56.8%); architectural distortion (31.8%); cardiomegaly (25.0%); lobar volume reduction (18.2%); and increased caliber of peripheral pulmonary arteries (9.1%). For most of the findings, the involvement was considered mild, five or fewer lung segments being affected. The accuracy in determining the type of hemoglobinopathy (HbSS group versus not HbSS group) was 72.7%. -
Respiratory Insufficiency in Patients with ALS at Or Near the End of Life
Amyotrophic lateral sclerosis (ALS) is a devastating motor neuron disease causing progressive paralysis and eventual death, usually from respiratory failure. Treatment for ALS is focused primarily on optimal symptom manage- ment because there is no known cure. Respiratory symptoms that occur are related to the disease process and can be very distressing for patients and their loved ones. Recommendations on the management of respira- tory insufficiency are provided to help guide clinicians caring for patients with ALS. Hospice and Palliative Care Feature The Management of Andrea L. Torres, APN, CNP Respiratory Insufficiency in Patients With ALS at or Near the End of Life 186 Home Healthcare Nurse www.homehealthcarenurseonline.com Copyright © 2012 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited. Introduction 2007). By the time most patients are definitively Amyotrophic lateral sclerosis (ALS) is a devastat- diagnosed, they are often already in an advanced ing motor neuron disease characterized by pro- stage of the disease (Wood-Allum & Shaw, 2010). gressive muscle weakness eventually leading to Life expectancy is typically 3-5 years from the paralysis and death. The onset typically occurs onset of symptoms (Elman et al., 2007). in late middle age, with men slightly more af- fected than women (Wood-Allum & Shaw, 2010). Palliative Care Approaches for ALS Patients The majority of cases of ALS have no known Due to the progressive nature of ALS, early pal- cause; about 10% of ALS cases are linked to a fa- liative care is an essential component in the milial trait (Ferguson & Elman, 2007). Treatment treatment plan, and should begin as soon as the is primarily focused on optimal symptom man- diagnosis of ALS is confirmed (Elman et al., 2007). -
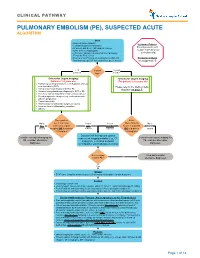
Pulmonary Embolism (Pe), Suspected Acute Algorithm
CLINICAL PATHWAY PULMONARY EMBOLISM (PE), SUSPECTED ACUTE ALGORITHM Start · Room air pulse oximetry Inclusion Criteria: · Consider supplemental oxygen · IV access and STAT CBC and DIC screen Patient presents with · Urine β-HCG, if appropriate suspected Pulmonary · CXR (PA + lateral), EKG and call the Cardiology Embolism (PE) Fellow for Echo review · Review criteria* for urgent imaging for possible PE Exclusion Criteria based on age-specific risk factors (see green boxes) No suspected PE < 18 Patient 18 years years old age? or older *Criteria for Urgent Imaging: *Criteria for Urgent Imaging: Patients < 18 years old For patients ≥ 18 years old · Painful leg swelling or known recent diagnosis of deep vein thrombosis (DVT) Please refer to the Wells Criteria · Family or personal history of DVT or PE Algorithm on page 7. · Known clotting disorder predisposing to DVT or PE · Recent or current indwelling central venous catheter · Elevated systemic estrogen (e.g., oral contraceptive pill use, pregnancy) · Recent immobility · Recent major or orthopedic surgery or trauma · Acute or chronic inflammatory condition · Obesity Does patient Is the No to meet 1 or more Yes to Yes to Wells Criteria No to ALL criteria for urgent ANY EITHER Score > 4 points BOTH criteria imaging OR is d-dimer criteria criterion OR is d-dimer criteria > 0.5ug/mL? > 0.5ug/mL? Discuss CXR findings and optimal Consider non-urgent imaging for subsequent imaging modality (e.g., CT Consider non-urgent imaging for PE, consider alternative angiogram, ventilation perfusion PE, consider -

Predictors of Impending Acute Chest Syndrome in Patients with Sickle Cell
www.nature.com/scientificreports OPEN Predictors of impending acute chest syndrome in patients with sickle cell anaemia Salam Alkindi1,2*, Ikhlas Al-Busaidi1, Bushra Al-Salami1, Samir Raniga3, Anil Pathare 1 & Samir K. Ballas4 Acute chest syndrome (ACS) is a major complication of sickle cell anaemia (SCA) and a leading cause for hospital admissions and death. We aimed to study the spectrum of clinical and laboratory features of ACS and to assess the predisposing factors and predictors of severity. A retrospective case-control cohort was studied by retrieving patient information from electronic medical records after ethical approval. One hundred adolescents and adults with SCA and hospital admissions for ACS were identifed through the discharge summaries, along with 20 additional patients presenting with VOC, but without ACS (controls). Among the patients with ACS, fever (>38.5 °C), reduced oxygen saturation (<95) and asplenia signifcantly difered when compared to those of controls (p < 0.05, chi-squared test). The degree of severity was refected in the use of non-invasive ventilation (NIV), simple and exchange transfusions, and the presence of bilateral pleural efusions and multi-lobar atelectasis/consolidation, which were signifcantly higher in the cases with ACS than in the controls. Lower haemoglobin (Hb) and high WBC counts were also signifcantly diferent between the two groups (p < 0.05, Student’s t test). Using logistic regression, our study further demonstrated that asplenia, fever, and reduced O2 saturation, along with low Hb and leukocytosis, were important predictors for the development of ACS. Sickle cell anaemia (SCA) is an autosomal recessive disorder characterized by a point mutation in codon 6 of the beta globin chain, where glutamic acid is replaced by valine, resulting in the formation of HbS with varied clinical 1 manifestations . -

CT Children's CLASP Guideline
CT Children’s CLASP Guideline Chest Pain INTRODUCTION . Chest pain is a frequent complaint in children and adolescents, which may lead to school absences and restriction of activities, often causing significant anxiety in the patient and family. The etiology of chest pain in children is not typically due to a serious organic cause without positive history and physical exam findings in the cardiac or respiratory systems. Good history taking skills and a thorough physical exam can point you in the direction of non-cardiac causes including GI, psychogenic, and other rare causes (see Appendix A). A study performed by the New England Congenital Cardiology Association (NECCA) identified 1016 ambulatory patients, ages 7 to 21 years, who were referred to a cardiologist for chest pain. Only two patients (< 0.2%) had chest pain due to an underlying cardiac condition, 1 with pericarditis and 1 with an anomalous coronary artery origin. Therefore, the vast majority of patients presenting to primary care setting with chest pain have a benign etiology and with careful screening, the patients at highest risk can be accurately identified and referred for evaluation by a Pediatric Cardiologist. INITIAL INITIAL EVALUATION: Focused on excluding rare, but serious abnormalities associated with sudden cardiac death EVALUATION or cardiac anomalies by obtaining the targeted clinical history and exam below (red flags): . Concerning Pain Characteristics, See Appendix B AND . Concerning Past Medical History, See Appendix B MANAGEMENT . Alarming Family History, See Appendix B . Physical exam: - Blood pressure abnormalities (obtain with manual cuff, in sitting position, right arm) - Non-innocent murmurs . Obtain ECG, unless confident pain is musculoskeletal in origin: - ECG’s can be obtained at CT Children’s main campus and satellites locations daily (Hartford, Danbury, Glastonbury, Shelton). -

Sickle Cell Pathway V2.1: Suspected Acute Chest Syndrome Table of Contents
Sickle Cell Pathway v2.1: Suspected Acute Chest Syndrome Table of Contents Inclusion Criteria · New, non-atelactatic, pulmonary infiltrate in patient with a Stop and sickle cell hemoglobinopathy Review Exclusion Criteria · O2 need related to opiate use with no infiltrate on CXR Sickle Cell Care Suspected Acute Chest Syndrome Appendix Summary of Version Changes Approval & Citation Evidence Ratings For questions concerning this pathway, contact: Last Updated: October 2020 [email protected] Next Expected Review: October 2025 If you are a patient with questions contact your medical provider, Medical Disclaimer © 2020 Seattle Children’s Hospital, all rights reserved Sickle Cell Pathway v2.1: Suspected Acute Chest Syndrome Inclusion Criteria · New, non-atelactatic, pulmonary infiltrate in patient with a Stop and sickle cell hemoglobinopathy Review Exclusion Criteria · O2 need related to opiate use with no infiltrate on CXR Evaluations for Acute Chest · Physical Exam · CXR · O2 sats · Consider viral studies · Blood & Urine Cx · CBC, diff, retic and type and cross Admit if not already admitted Standard Conservative Therapy · Aggressive pain management · Incentive spirometry q 1 hrs while awake, 10 breaths every hour from 0800 to 2200 and with vital signs while awake from 2200 to 0800, as well as with every "as needed" IV bolus of pain medication, and prior to chest x-rays · Oxygen to maintain O2 saturation >93% · Ceftriaxone q 24 hours IV (Ciprofloxacin and Clindamycin if allergic to Ceftriaxone) ! · Azithromycin or other -

A Case of Extreme Hypercapnia
119 Emerg Med J: first published as 10.1136/emj.2003.005009 on 20 January 2004. Downloaded from CASE REPORTS A case of extreme hypercapnia: implications for the prehospital and accident and emergency department management of acutely dyspnoeic patients L Urwin, R Murphy, C Robertson, A Pollok ............................................................................................................................... Emerg Med J 2004;21:119–120 64 year old woman was brought by ambulance to the useful non-invasive technique to aid the assessment of accident and emergency department. She had been peripheral oxygen saturation. In situations of poor perfusion, Areferred by her GP because of increasing dyspnoea, movement and abnormal haemoglobin, however, this tech- cyanosis, and lethargy over the previous four days. On arrival nique may not reliably reflect PaO2 values. More importantly, of the ambulance crew at her home she was noted to be and as shown in our case, there is no definite relation tachycardic and tachypnoeic (respiratory rate 36/min) with a between SaO2 values measured by pulse oximetry and PaCO2 GCS of 5 (E 3, M 1, V 1). She was given oxygen at 6 l/min via values although it has been shown that the more oxygenated a Duo mask, and transferred to hospital. The patient arrived at the accident and emergency department 18 minutes later. In transit, there had been a clinical deterioration. The GCS was now 3 and the respiratory rate 4/min. Oxygen saturation, as measured by a pulse oximeter was 99%. The patient was intubated and positive pressure ventilation started. Arterial blood gas measurements taken at the time of intubation were consistent with acute on chronic respiratory failure (fig 1).