Using Virtual Reality As a Therapeutic Modality for Children with Cerebral Palsy: a Review and Synthesis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
History of Value Creation
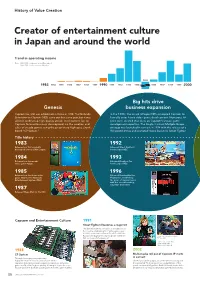
History of Value Creation Creator of entertainment culture in Japan and around the world Trend in operating income Note: 1983–1988: Fiscal years ended December 31 1989–2020: Fiscal years ended March 31 1995 1983 1984 1985 1986 1987 1988 1989 1990 1991 1992 1993 1994 1996 1997 1998 1999 2000 Big hits drive Genesis business expansion Capcom Co., Ltd. was established in Osaka in 1983. The Nintendo In the 1990s, the arrival of Super NES prompted Capcom to Entertainment System (NES) came out that same year, but it was formally enter home video game development. Numerous hit difficult to develop high-quality arcade-level content for, so titles were created that drew on Capcom’s arcade game Capcom focused business development on the creation and development expertise. The Single Content Multiple Usage sales of arcade games using the proprietary high-spec circuit strategy was launched in earnest in 1994 with the release of a board “CP System.” Hollywood movie and animated movie based on Street Fighter. Title history 1983 1992 Released our first originally Released Street Fighter II developed coin-op Little League. for the Super NES. 1984 1993 Released our first arcade Released Breath of Fire video game Vulgus. for the Super NES. 1985 1996 Released our first home video Released Resident Evil for game 1942 for the Nintendo PlayStation, establishing Entertainment System (NES). the genre of survival horror with this record-breaking, long-time best-seller. 1987 Released Mega Man for the NES. Capcom and Entertainment Culture 1991 Street Fighter II becomes a major hit The game became a sensation in arcades across the country, establishing the fighting game genre. -
3.2.2 Microsd-Muistikortti
RETROPIE-PROJEKTI Emulointiaseman konfigurointi ja käyttöönotto Eero Räsänen Opinnäytetyö Toukokuu 2015 Tietotekniikka Tietoliikennetekniikka ja tietoverkot TIIVISTELMÄ Tampereen ammattikorkeakoulu Tietotekniikan koulutusohjelma Tietoliikennetekniikka ja tietoverkot EERO RÄSÄNEN RetroPie-projekti Emulointiaseman konfigurointi ja käyttöönotto Opinnäytetyö 68 sivua, joista liitteitä 6 sivua Toukokuu 2015 Opinnäytetyön aiheena oli tutustua Raspberry Pi:lle tehtyyn RetroPie-projektiin, sekä sen konfigurointiin ja käyttöönottoon. Työssä esitellään itse RetroPie-projekti, sen toteuttamiseen tarvittavat ohjelmat ja laitteet, sekä kerrotaan "How to" -näkökulmasta projektin toteuttaminen. Projektia voidaan muokata haluamalla tavalla, mutta tähän on sisällytetty oma näkemykseni parhaasta mahdollisesta RetroPie-projektista ja sen sisällöstä. RetroPie-projekti mahdollistaa helpon tavan asentaa yli 30 erilaista emulaattoria Raspberry Pi:n sisälle. Projekti käyttää EmulationStationia graafisena front-endinä, ja RetroPie Setup -skriptiä back-endinä tarvittavien Rasbian-pakettien asentamiseen. Tämä on yksi suosituimmista Raspberry Pi:lle toteutetuista projekteista, jolla pääsee nauttimaan nostalgisesta retropelaamisesta. Opinnäytetyön ohjeet RetroPie-projektin toteuttamisesta sopivat hyvin tavalliselle Raspberry Pi -pohjasta kiinnostuneelle henkilölle, jolla ei ole juurikaan aikaisempaa Linux-osaamista. Työ sisältää välttämättömimmät konfiguraatiot, jotta RetroPie saadaan toimimaan tavallisen videopelikonsolin tavoin. Lisäksi työssä on lisäominaisuutena -

Company Profile President's Message
Doc.02 99.9.30 6:31 PM Page H2 1 COMPANY PROFILE PRESIDENT’S MESSAGE A leading company in the amusement have succeeded in producing one hit after advertising and incentive-based consumer industry, Capcom develops, publishes and another, and the release of Resident Evil in promotions such as our innovative Fighters Edge program. distributes a variety of software games for March 1996 established a new genre, both arcade machines and home video "Survival Horror", which is unrivaled by our With the new millennium on the horizon, the business consoles. We also operate amusement competitors. Popular all over the world, the world is on the brink of change. We are entering an age where consumers will have the power of choice. facilities at 47 locations in Japan. Since the outstanding Resident Evil series has Bidding farewell to mass consumption, we will see foundation of the company in May 1979, we contributed enormously to Capcom's growth. the development of an information-centered society have taken a leading role in the entertainment In addition to our existing overseas which contributes to a higher level of customer software industry and have continued to subsidiaries in the United States and Asia, we satisfaction as well as increased environmental awareness. And in the years to come, the world will respond to the demand and expectations of established Capcom Eurosoft in London, continue to change at a faster rate than ever. customers. In March 1991, we achieved the England in July 1998, as a main sales base for top position in the arcade game industry with the European home video game market. -

Graphical Process Unit a New Era
Nov 2014 (Volume 1 Issue 6) JETIR (ISSN-2349-5162) Graphical Process Unit A New Era Santosh Kumar, Shashi Bhushan Jha, Rupesh Kumar Singh Students Computer Science and Engineering Dronacharya College of Engineering, Greater Noida, India Abstract - Now in present days every computer is come with G.P.U (graphical process unit). The graphics processing unit (G.P.U) has become an essential part of today's mainstream computing systems. Over the past 6 years, there has been a marked increase in the performance and potentiality of G.P.U. The modern G.P.Us is not only a powerful graphics engine but also a deeply parallel programmable processor showing peak arithmetic and memory bandwidth that substantially outpaces its CPU counterpart. The G.P.U's speedy increase in both programmability and capability has spawned a research community that has successfully mapped a broad area of computationally demanding, mixed problems to the G.P.U. This effort in general-purpose computing on the G.P.Us, also known as G.P.U computing, has positioned the G.P.U as a compelling alternative to traditional microprocessors in high-performance computer systems of the future. We illustrate the history, hardware, and programming model for G.P.U computing, abstract the state of the art in tools and techniques, and present 4 G.P.U computing successes in games physics and computational physics that deliver order-of- magnitude performance gains over optimized CPU applications. Index Terms - G.P.U, History of G.P.U, Future of G.P.U, Problems in G.P.U, eG.P.U, Integrated graphics ________________________________________________________________________________________________________ I. -

“Análisis Y Configuración De API's Para Ejecución De Aplicaciones
ESCUELA SUPERIOR POLITECNICA DE CHIMBORAZO FACULTAD DE INFORMATICA Y ELECTRONICA ESCUELA DE INGENIERIA EN SISTEMAS “Análisis y Configuración de API’s para ejecución de Aplicaciones Microsoft Office en un entorno de Windows bajo Linux”. TESIS DE GRADO Previa la obtención del título de INGENIERO EN SISTEMAS INFORMATICOS Presentado por: SAMUEL CARRASCO LLERENA RIOBAMBA – ECUADOR 2008 - 2 - AGRADECIMIENTO Mi profundo y sincero agradecimiento a quienes han sido parte importante de mi vida académica: A Dios, Por su presencia en mi vida y por su guía en la realización de esta tesis. A mis padres, José y Teresita, Por su constante e incondicional apoyo, por sus fervientes oraciones en mi favor. A mis Asesores de Tesis, Ing. Danilo Pastor e Ing. Jorge Menéndez, Por su valioso e invaluable aporte al desarrollo de esta tesis. - 3 - Con amor incondicional, dedico esta tesis a las tres mujeres que con su existencia alegran mi corazón: AMBITAR TERESITA PRISCILA - 4 - FIRMAS DE RESPONSABILIDAD NOMBRE NOTA FIRMA Dr. Romeo Rodríguez DECANO FACULTAD INFORMATICA Y ELECTRONICA Ing. Iván Menes DIRECTOR ESCUELA DE INGENIERIA EN SISTEMAS Ing. Danilo Pástor DIRECT OR DE TESIS Ing. Jorge Menéndez V. MIEMBRO DE TESIS Tlgo. Carlos Rodríguez DIRECTOR CENTRO DE DOCUMENTACION Nota: - 5 - RESPONSABILIDAD DEL AUTOR Yo, Samuel Carrasco Llerena, soy responsable de las ideas, doctrinas y resultados expuestos en esta tesis; el Patrimonio intelectual de esta tesis de grado pertenece a la Escuela Superior Politécnica de Chimborazo. ____________________ Samuel Carrasco Ll. -

Universidad De Guadalajara
Universidad de Guadalajara Centro Universitario en Arte, Arquitectura y Diseño Doctorado Interinstitucional en Arte y Cultura Tema de Tesis: En contra de la momificación. Los videojuegos como artefactos de cultura visual contemporánea: la emulación y simulación a nivel circuito, a modo de tácticas de su preservación Tesis que para obtener el grado de Doctor en Arte y Cultura Presenta: Romano Ponce Díaz Director de Tesis: Dr. Jorge Arturo Chamorro Escalante Línea de Generación y Aplicación del Conocimiento: Artes Visuales. Guadalajara, Jalisco, febrero del 2019 1 En contra de la momificación. Los videojuegos como artefactos de cultura visual contemporánea: la emulación y simulación a nivel circuito, a modo de tácticas de su preservación. ©Derechos Reservados 2019 Romano Ponce Díaz [romano.ponce@ alumnos.udg.mx] 2 ÍNDICE DE ILUSTRACIONES. 8 ÍNDICE DE TABLAS. 8 1.1 PRESENTACIÓN 9 1.2 AGRADECIMIENTOS 11 1.3 RESUMEN 13 1.4 ABSTRACT 14 2 PRIMER NODO: EXPOSICIÓN. 16 2.1.1 CAPÍTULO 2. EL PROBLEMA PREFIGURADO: 19 2.2 OTRO EPÍLOGO A MANERA DE PRÓLOGO. 19 2.3 EL RELATO COMO PRESERVADOR DEL TESTIMONIO DE LA CULTURA. 20 2.4 LA MEMORIA PROSTÉTICA, SU RELACIÓN CON LOS OBJETOS, Y, LA NATURALEZA FINITA 27 2.4.1 CINEMATOGRAFÍA, EXPLOSIONES Y FILMES PERDIDOS 29 2.4.2 LOS VIDEOJUEGOS Y LAS FORMAS DE MIRAR AL MUNDO 33 2.4.3 VIDEOJUEGOS, IDEOLOGÍA, VISUALIDAD Y ARTE: 35 2.4.4 LA ESTRUCTURA DE LA OBSOLESCENCIA Y EL MALESTAR DE LA CULTURA 46 2.5 ANTES DE QUE CAIGA EN EL OLVIDO: UNA HIPÓTESIS 49 2.5.1 SOBRE LOS OBJETIVOS, ALCANCES, Y LA MORFOLOGÍA DEL TEXTO 51 3 CAPÍTULO 3. -
CAPCOM INTEGRATED REPORT 2019 Code Number: 9697
CAPCOM CO., LTD. INTEGRATED REPORT 2019 Captivating a Connected World CAPCOM INTEGRATED REPORT 2019 Code Number: 9697 Code Number: 9697 Advancing Our Global Brand Further Monster Hunter World: Iceborne Released in January 2018, Monster Hunter: World (MH:W, below), succeeded on two key elements of our growth strategy, namely globalization and shifting to digital. This propelled it to over 12.4 million units shipped worldwide, making it Capcom’s biggest hit ever. We aim to grow the fanbase even further by continuing to advance these two elements on Monster Hunter World: Iceborne (MHW:I, below), which is scheduled for release during the fiscal year ending March 2020. For details, see p. 35 of the Integrated Report 2018. Globalization Increasing global users by supporting 12 languages 1 and launching titles simultaneously worldwide The two key MH : W raised the Monster Hunter series to global Overseas Approximately 25% elements to brand status by increasing the overseas sales ratio to our success roughly 60%, compared to its historical 25%. We plan to solidify our global user base with MHW:I Overseas by releasing it simultaneously around the globe and Approximately offering the game in 12 languages. 75% 01 CAPCOM INTEGRATED REPORT 2019 Digital Shift 2 Taking our main sales and marketing channels online We expect the bulk of MHW:I sales to be digital. While we maximize revenue using the digital marketing data Trial version we have accumulated up to this point, we will analyze Feedback Capcom user purchasing trends to utilize in digital sales -

Promoting Growth Strategies and Governance Reforms Aimed at Enhancing Corporate Value
To Our Stakeholders (From the CEO & COO) Capcom’s Value Message from Growth Strategy Business Activity ESG Information Financial and Creation Activities Management Achievements Corporate Data Promoting Growth Strategies and Governance Reforms Aimed at Enhancing Corporate Value Creating Entertaining Games that Continue to Excite People Around the World –––– This is the cornerstone of Capcom’s business activities and the source of our corporate value. Through our business activities, we bring the Company economic benefits while providing society with new value. We believe the value of a corporation stems from shared value creation. As the game market expands globally, in addition to pursuing short-term profit, Capcom is promoting growth strategies from a medium- to long-term perspective in order to continue enhancing corporate value into the future. Going forward, we will transform our fundamental revenue model from a one-time sale “transactional model” to an ongoing “recurring revenue model,” while at the same time thoroughly executing our Single Content Multiple Usage strategy and constructing a portfolio to achieve stable earnings. We will also engage in governance reforms to control risks that increase proportionally with the acceleration of our growth strategies, thoroughly implement management visualization and systemization and create a structure enabling rational management decisions based on an institutional design with external directors at its core. Furthermore, we will make an effort to strengthen non-financial capital not reflected in quantitative data. In addition to enhancing Capcom’s highly original content, the source of our competitive edge, and the development structure that creates it, we will build positive relationships with business partners, regional communities, employees and a variety of stakeholders among other important “capital” comprising Capcom corporate value. -

The Effect of Screen Sizes on Gamers' Intrinsic Motivation
THE EFFECT OF SCREEN SIZES ON GAMERS’ INTRINSIC MOTIVATION WHEN PLAYING GAMES Noor Fardela Zainal Abidin A thesis submitted to Auckland University of Technology in fulfilment of the requirements for the Degree of Doctor of Philosophy (PhD) 2017 School of Engineering, Computer and Mathematical Sciences Primary Supervisor: Dr. Robert Wellington Secondary Supervisor: Professor Stephen MacDonell ABSTRACT This thesis reports on a study of the motivation of players of educational or constructive (E rated) games in relation to the screen size they used in game play. Educators have started to use games in the class room to encourage learning, and often they have been using small hand held consoles, but more work was needed on understanding the intrinsic motivation for engagement. Since engagement is what has prompted the uptake of educational gaming, this was deemed an important area to research. The growing popularity of video games has provoked scholars to look into various aspects of gaming. In this regard, one particular area of investigation is in relation to the intrinsic motivation among the gamers. Multiple screen sizes are found to influence players to play games from various viewpoints. For instance, from handheld consoles such as Nintendo Dual Screen (DS) and PlayStation Portable (PSP) as well as television based consoles like PlayStation 3, Xbox 360, and Nintendo Wii. Despite a significant number of studies on motivation that have looked into how games should be designed in order to motivate gamers, few studies have investigated the effects of screen sizes on them Therefore, this thesis investigates the effect of screen sizes on gamers’ intrinsic motivation when playing games. -

Table of Contents
Building Embedded Linux Systems Author : Karim Yaghmour Publisher : O'Reilly Date Published : April 2003 ISBN : 0-596-00222-X Table of Contents Dedication Preface Audience of This Book Scope and Background Information Organization of the Material Hardware Used in This Book Software Versions Book Web Site Typographical Conventions Contact Information Acknowledgments Chapter 1. Introduction Section 1.1. Definitions Section 1.2. Real Life and Embedded Linux Systems Section 1.3. Example Multicomponent System Section 1.4. Design and Implementation Methodology Chapter 2. Basic Concepts Section 2.1. Types of Hosts Section 2.2. Types of Host/Target Development Setups Section 2.3. Types of Host/Target Debug Setups Section 2.4. Generic Architecture of an Embedded Linux System Section 2.5. System Startup Section 2.6. Types of Boot Configurations Section 2.7. System Memory Layout Chapter 3. Hardware Support Section 3.1. Processor Architectures Section 3.2. Buses and Interfaces Section 3.3. I/O Section 3.4. Storage Section 3.5. General Purpose Networking Section 3.6. Industrial Grade Networking Section 3.7. System Monitoring Chapter 4. Development Tools Section 4.1. Using a Practical Project Workspace Section 4.2. GNU Cross-Platform Development Toolchain Section 4.3. C Library Alternatives Section 4.4. Java Section 4.5. Perl Section 4.6. Python Section 4.7. Ada Section 4.8. Other Programming Languages Section 4.9. Integrated Development Environments Section 4.10. Terminal Emulators Chapter 5. Kernel Considerations Section 5.1. Selecting a Kernel Section 5.2. Configuring the Kernel Section 5.3. Compiling the Kernel Section 5.4. -

Advanced Technology to Lead the Industry
CAPCOM CO., LTD. INTEGRATED REPORT INTEGRATED CAPCOM CO., LTD. 3-1-3 Uchihirano-machi, Chuo-ku, Osaka, 540-0037, Japan PHONE: 81-6-6920-3600 FAX: 81-6-6920-5100 http://www.capcom.co.jp/ ©CAPCOM CO., LTD. ALL RIGHTS RESERVED. 2016 Capcom Investor Relations Website http://www.capcom.co.jp/ir/english/ We have been focusing on IR activities by providing our shareholders and investors with timely and updated information through our website. CAPCOM INTEGRATED REPORT 2016 Smartphone Access If you have a smartphone that reads QR codes (two-dimensional bar codes), scan the image on the right for easy access to the site. Advanced Technology to Lead the Industry Cover Image The cover image shows Capcom’s development offices in Osaka. The building at lower right is R&D Building #2, boasting one of the newest development facilities in Japan, just completed in 2016. Code Number: 9697 At upper left is the R&D Building, completed in 1996. These two buildings will serve as a base as we The print of this catalog uses move forward with the strengthening environment-friendly vegetable oil ink. of our development structure. Code Number: 9697 billion $Global Game100 Market to Exceed 100 Billion Dollars in 2017 Global Game Market (Billions of dollars) Over100 100.6 103.2 94.2 85.8 68.8 2014 2015 2016 2017 2018 (Year) (forecast) (forecast) (forecast) Source: International Development Group Game Market Expanding More Rapidly than Anticipated The global game market continues to grow beyond previous market forecasts and is expected to exceed 100 billion dollars in 2017. -

The Use of Gamification Within Motion-Based Interventions for Children with Cerebral
The use of gamification within motion-based interventions for children with cerebral palsy - a systematic review - Cathrin Frentjen (s1358057) University of Twente Department of Positive Psychology and Technology Education program: Bachelor of Psychology 1st Supervisor: Dr. Elian de Kleine 2nd Supervisor: Dr. Saskia M. Kelders JUNE, 2015 Bachelorthesis June, 2015 Structure of this Bachelorthesis The thesis starts with a cover page, followed by an abstract. The abstract is written twice in English and in Dutch. I decided to write the entire thesis in English and appreciate the opportunity to get more confident in this foreign language. I´m a native German who´s studies abroad in the Netherlands, which opens up new horizons for me. The Netherlands are very advanced in the use of technology, especially at the University of Twente. This reinforces my decision to explore the topic of this thesis. After the abstract, a section of acknowledgement and a table of content comes up. The introduction (1) of this thesis outlines the problem of the disease cerebral palsy by giving a description of its etiology, it´s manifestation and pathology and current treatment methods. Besides, the introduction gives a theoretical overview of the research questions, which belong to gamification as possible treatment method. The next part is the method section (2). At this point the research methods and methodological process of the systematic literature search are highlighted. This section ends with a list of suited articles. Based on selected articles, the results emerge (3). In this section all findings from the assessment and evaluation of the articles are shown.