1.4. Shear-Stress Sensing of Vascular Endothelial Cells
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
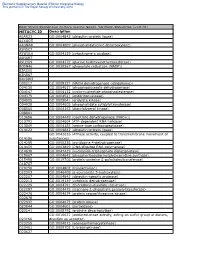
METACYC ID Description A0AR23 GO:0004842 (Ubiquitin-Protein Ligase
Electronic Supplementary Material (ESI) for Integrative Biology This journal is © The Royal Society of Chemistry 2012 Heat Stress Responsive Zostera marina Genes, Southern Population (α=0. -

Abstracts from the 10Th World Congress for Microcirculation
DOI:10.1111/micc.12246 Abstracts Abstracts from the 10th World Congress for Microcirculation September 25th – 27th, 2015 Kyoto, Japan PLENARY LECTURES vascular neutrophils that constantly patrol the lung and can detect and phagocytose bacteria attached to endothelium suggesting some communication inter-cellular communica- PL1 tion. Clearly much anti-microbial activity occurs in the Imaging the microcirculation in infections vasculature prior to dissemination of bacteria into tissues. P Kubes University of Calgary, Calgary, Canada PL2 Using spinning disk microscopy has allowed us to track pathogens and immune cells in the microcirculation. Mapping oxygen in the brain of awake resting Observing the liver microvasculature revealed numerous mice immune speed bumps that slowed, delayed and even S Charpak prevented bacteria from disseminating to other organs. For Laboratory of Neurophysiology and New Microscopies, Inserm U1128, example, when Borrelia burgdorferi enters the vasculature Paris Descartes University, Paris, France they are immediately caught by the liver vascular macro- The brain is extremely sensitive to hypoxia. Yet, the phage, the Kupffer cells and are engulfed and antigens are physiological values of oxygen concentration in the brain presented on CD1d to resident vascular immune cells remain elusive because high resolution measurements have including invariant Natural Killer T cells (iNKT cells). These only been performed during anesthesia, which affects two iNKT cells receive messages and rapidly make gamma main parameters modulating tissue oxygenation, i.e. interferon to help with immunity. Absence of these events neuronal activity and cerebral blood flow. Using the recent leads to massive dissemination of borrelia especially to joints. finding that measurements of capillary erythrocyte-associ- In the joints the iNKT cells live closely apposed but outside ated transients i.e. -

(10) Patent No.: US 8119385 B2
US008119385B2 (12) United States Patent (10) Patent No.: US 8,119,385 B2 Mathur et al. (45) Date of Patent: Feb. 21, 2012 (54) NUCLEICACIDS AND PROTEINS AND (52) U.S. Cl. ........................................ 435/212:530/350 METHODS FOR MAKING AND USING THEMI (58) Field of Classification Search ........................ None (75) Inventors: Eric J. Mathur, San Diego, CA (US); See application file for complete search history. Cathy Chang, San Diego, CA (US) (56) References Cited (73) Assignee: BP Corporation North America Inc., Houston, TX (US) OTHER PUBLICATIONS c Mount, Bioinformatics, Cold Spring Harbor Press, Cold Spring Har (*) Notice: Subject to any disclaimer, the term of this bor New York, 2001, pp. 382-393.* patent is extended or adjusted under 35 Spencer et al., “Whole-Genome Sequence Variation among Multiple U.S.C. 154(b) by 689 days. Isolates of Pseudomonas aeruginosa” J. Bacteriol. (2003) 185: 1316 1325. (21) Appl. No.: 11/817,403 Database Sequence GenBank Accession No. BZ569932 Dec. 17. 1-1. 2002. (22) PCT Fled: Mar. 3, 2006 Omiecinski et al., “Epoxide Hydrolase-Polymorphism and role in (86). PCT No.: PCT/US2OO6/OOT642 toxicology” Toxicol. Lett. (2000) 1.12: 365-370. S371 (c)(1), * cited by examiner (2), (4) Date: May 7, 2008 Primary Examiner — James Martinell (87) PCT Pub. No.: WO2006/096527 (74) Attorney, Agent, or Firm — Kalim S. Fuzail PCT Pub. Date: Sep. 14, 2006 (57) ABSTRACT (65) Prior Publication Data The invention provides polypeptides, including enzymes, structural proteins and binding proteins, polynucleotides US 201O/OO11456A1 Jan. 14, 2010 encoding these polypeptides, and methods of making and using these polynucleotides and polypeptides. -

Molekularbiologie Und Pharmakologie Neuer G-Protein-Gekoppelter Purin-Rezeptoren
Molekularbiologie und Pharmakologie neuer G-Protein-gekoppelter Purin-Rezeptoren Dissertation zur Erlangung des Doktorgrades (Dr. rer. nat.) der Mathematisch-Naturwissenschaftlichen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn vorgelegt von Melanie Knospe (geb. Hulbert) aus Bonn Bonn 2012 Angefertigt mit Genehmigung der Mathematisch-Naturwissenschaftlichen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn. 1. Gutachter: Prof. Dr. Christa E. Müller 2. Gutachter: Prof. Dr. Ivar von Kügelgen Tag der Promotion: 28.03.2012 Erscheinungsjahr: 2012 Diese Dissertation ist auf dem Hochschulserver der ULB Bonn (http://hss.ulb. uni-bonn.de/diss_online) elektronisch publiziert. Die vorliegende Arbeit wurde in der Zeit von Juni 2008 bis Dezember 2011 am Pharmazeutischen Institut der Rheinischen Friedrich-Wilhelms-Universität Bonn unter der Leitung von Frau Prof. Dr. Christa E. Müller durchgeführt. Mein besonderer Dank gebührt Frau Prof. Dr. Christa E. Müller für die Über- lassung des interessanten Themas, die fachliche Unterstützung, für die vielen wertvollen Anregungen und Diskussionen sowie die konstruktive Kritik beim Erstellen dieser Arbeit. Herrn Prof. Dr. Ivar von Kügelgen danke ich für die freundliche Übernahme des Koreferats. Für die Mitwirkung in meiner Prüfungskommission bedanke ich mich bei Herrn Prof. Dr. med. Klaus Mohr und Herrn Prof. Dr. Günther Mayer. Ich danke der NRW International Graduate Research School LIMES Chemical Biology für die finanzielle Unterstützung in Form eines Doktorandenstipendiums sowie -

Supplementary Informations SI2. Supplementary Table 1
Supplementary Informations SI2. Supplementary Table 1. M9, soil, and rhizosphere media composition. LB in Compound Name Exchange Reaction LB in soil LBin M9 rhizosphere H2O EX_cpd00001_e0 -15 -15 -10 O2 EX_cpd00007_e0 -15 -15 -10 Phosphate EX_cpd00009_e0 -15 -15 -10 CO2 EX_cpd00011_e0 -15 -15 0 Ammonia EX_cpd00013_e0 -7.5 -7.5 -10 L-glutamate EX_cpd00023_e0 0 -0.0283302 0 D-glucose EX_cpd00027_e0 -0.61972444 -0.04098397 0 Mn2 EX_cpd00030_e0 -15 -15 -10 Glycine EX_cpd00033_e0 -0.0068175 -0.00693094 0 Zn2 EX_cpd00034_e0 -15 -15 -10 L-alanine EX_cpd00035_e0 -0.02780553 -0.00823049 0 Succinate EX_cpd00036_e0 -0.0056245 -0.12240603 0 L-lysine EX_cpd00039_e0 0 -10 0 L-aspartate EX_cpd00041_e0 0 -0.03205557 0 Sulfate EX_cpd00048_e0 -15 -15 -10 L-arginine EX_cpd00051_e0 -0.0068175 -0.00948672 0 L-serine EX_cpd00054_e0 0 -0.01004986 0 Cu2+ EX_cpd00058_e0 -15 -15 -10 Ca2+ EX_cpd00063_e0 -15 -100 -10 L-ornithine EX_cpd00064_e0 -0.0068175 -0.00831712 0 H+ EX_cpd00067_e0 -15 -15 -10 L-tyrosine EX_cpd00069_e0 -0.0068175 -0.00233919 0 Sucrose EX_cpd00076_e0 0 -0.02049199 0 L-cysteine EX_cpd00084_e0 -0.0068175 0 0 Cl- EX_cpd00099_e0 -15 -15 -10 Glycerol EX_cpd00100_e0 0 0 -10 Biotin EX_cpd00104_e0 -15 -15 0 D-ribose EX_cpd00105_e0 -0.01862144 0 0 L-leucine EX_cpd00107_e0 -0.03596182 -0.00303228 0 D-galactose EX_cpd00108_e0 -0.25290619 -0.18317325 0 L-histidine EX_cpd00119_e0 -0.0068175 -0.00506825 0 L-proline EX_cpd00129_e0 -0.01102953 0 0 L-malate EX_cpd00130_e0 -0.03649016 -0.79413596 0 D-mannose EX_cpd00138_e0 -0.2540567 -0.05436649 0 Co2 EX_cpd00149_e0 -

Native Potatoes Apyrase Cat
Native Potatoes Apyrase Cat. No. NATE-0085 Lot. No. (See product label) Introduction Description Apyrase is found in all eukaryotes and some prokaryotes. Apyrase, from potato, has a crucial role in regulating growth and development. Apyrase is involved in the inactivation of synaptic ATP as a neurotransmitter following nerve stimulation and in the inhibition of ADP induced platelet aggregation to prevent thrombosis. Divalent metal ions are required for activity and best activity is observed with calcium ion at 5 mM. Applications At least two isoenzymes are found in different varieties of S. tuberosum:4,5 one with a high ATPase/ADPase ratio (∼10) and another with a low ratio (∼1). Reaction: ATP → ADP+Pi → AMP+2Pi.Apyrase is used to hydrolyze nucleoside triphosphates and diphosphates. For hydrolysis of organic di and triphosphates, the optimal pH is 6, and for inorganic substrates, the optimal pH is 5.1. Apyrase, from Creative Enzymes, has been used in inhibition studies of platelet-aggregation. Synonyms ATP-diphosphatase; adenosine diphosphatase; ADPase; ATP diphosphohydrolase; apyrase; EC 3.6.1.5; 9000-95-7 Product Information Source Potatoes Form lyophilized powder. Partially purified, lyophilized powder containing potassium succinate buffer salts. EC Number EC 3.6.1.5 CAS No. 9000-95-7 Activity > 200 units/mg protein; > 600 units/mg protein Buffer H2O: soluble 1.0 mg/mL Pathway Purine metabolism, organism-specific biosystem; Pyrimidine metabolism, organism-specific biosystem; Pyrimidine metabolism, conserved biosystem Unit Definition One unit will liberate 1.0 μmole of inorganic phosphate from ATP or ADP per min at pH 6.5 at 30°C. -

Generated by SRI International Pathway Tools Version 25.0, Authors S
Authors: Pallavi Subhraveti Ron Caspi Peter Midford Peter D Karp An online version of this diagram is available at BioCyc.org. Biosynthetic pathways are positioned in the left of the cytoplasm, degradative pathways on the right, and reactions not assigned to any pathway are in the far right of the cytoplasm. Transporters and membrane proteins are shown on the membrane. Ingrid Keseler Periplasmic (where appropriate) and extracellular reactions and proteins may also be shown. Pathways are colored according to their cellular function. Gcf_000190595Cyc: Cellulophaga lytica DSM 7489 Cellular Overview Connections between pathways are omitted for legibility. Anamika Kothari phosphate molybdate RS04350 RS08315 phosphate molybdate Macromolecule Modification tRNA-uridine 2-thiolation inosine 5'- Nucleoside and Nucleotide Degradation ditrans,octacis- a peptidoglycan with ditrans,octacis- a [bis(guanylyl an N-terminal- a [protein] and selenation (bacteria) phosphate guanosine ditrans,octacis- (4R)-4-hydroxy- an L-asparaginyl- an L-cysteinyl- Aminoacyl-tRNA Charging tRNA charging nucleotides undecaprenyldiphospho- (L-alanyl-γ-D-glutamyl- undecaprenyldiphospho- undecaprenyldiphospho- molybdopterin) cys L-methionyl-L- C-terminal glu degradation 2-oxoglutarate [tRNA Asn ] [tRNA Cys ] degradation III N-acetyl-(N-acetyl-β-D- L-lysyl-D-alanyl-D- N-acetyl-(N- N-acetyl-(N- cofactor cysteinyl-[protein] L-glutamate cys glucosaminyl)muramoyl- alanine) pentapeptide acetylglucosaminyl) acetylglucosaminyl) chaperone]- Phe IMP bifunctional phe a tRNA L-alanyl-γ-D-glutamyl-L- -

POLSKIE TOWARZYSTWO BIOCHEMICZNE Postępy Biochemii
POLSKIE TOWARZYSTWO BIOCHEMICZNE Postępy Biochemii http://rcin.org.pl WSKAZÓWKI DLA AUTORÓW Kwartalnik „Postępy Biochemii” publikuje artykuły monograficzne omawiające wąskie tematy, oraz artykuły przeglądowe referujące szersze zagadnienia z biochemii i nauk pokrewnych. Artykuły pierwszego typu winny w sposób syntetyczny omawiać wybrany temat na podstawie możliwie pełnego piśmiennictwa z kilku ostatnich lat, a artykuły drugiego typu na podstawie piśmiennictwa z ostatnich dwu lat. Objętość takich artykułów nie powinna przekraczać 25 stron maszynopisu (nie licząc ilustracji i piśmiennictwa). Kwartalnik publikuje także artykuły typu minireviews, do 10 stron maszynopisu, z dziedziny zainteresowań autora, opracowane na podstawie najnow szego piśmiennictwa, wystarczającego dla zilustrowania problemu. Ponadto kwartalnik publikuje krótkie noty, do 5 stron maszynopisu, informujące o nowych, interesujących osiągnięciach biochemii i nauk pokrewnych, oraz noty przybliżające historię badań w zakresie różnych dziedzin biochemii. Przekazanie artykułu do Redakcji jest równoznaczne z oświadczeniem, że nadesłana praca nie była i nie będzie publikowana w innym czasopiśmie, jeżeli zostanie ogłoszona w „Postępach Biochemii”. Autorzy artykułu odpowiadają za prawidłowość i ścisłość podanych informacji. Autorów obowiązuje korekta autorska. Koszty zmian tekstu w korekcie (poza poprawieniem błędów drukarskich) ponoszą autorzy. Artykuły honoruje się według obowiązujących stawek. Autorzy otrzymują bezpłatnie 25 odbitek swego artykułu; zamówienia na dodatkowe odbitki (płatne) należy zgłosić pisemnie odsyłając pracę po korekcie autorskiej. Redakcja prosi autorów o przestrzeganie następujących wskazówek: Forma maszynopisu: maszynopis pracy i wszelkie załączniki należy nadsyłać w dwu egzem plarzach. Maszynopis powinien być napisany jednostronnie, z podwójną interlinią, z marginesem ok. 4 cm po lewej i ok. 1 cm po prawej stronie; nie może zawierać więcej niż 60 znaków w jednym wierszu nie więcej niż 30 wierszy na stronie zgodnie z Normą Polską. -

Reconstruction and Analysis of Cattle Metabolic Networks in Normal and Acidosis Rumen Tissue
animals Article Reconstruction and Analysis of Cattle Metabolic Networks in Normal and Acidosis Rumen Tissue Maryam Gholizadeh 1, Jamal Fayazi 1,* , Yazdan Asgari 2, Hakimeh Zali 3 and Lars Kaderali 4 1 Department of Animal Science, Faculty of Animal Science and Food Technology, Agricultural Sciences and Natural Resources University of Khuzestan, Mollasani, Ahvaz 6341773637, Iran; [email protected] 2 Department of Medical Biotechnology, School of Advanced Technologies in Medicine, Tehran University of Medical Sciences, Tehran 1416753955, Iran; [email protected] 3 School of Advanced Technologies in Medicine, Shahid Beheshti University of Medical Sciences, Tehran 1416753955, Iran; [email protected] 4 Institute of Bioinformatics, University Medicine Greifswald, Felix-Hausdorff-Str. 8, 17475 Greifswald, Germany; [email protected] * Correspondence: [email protected]; Tel.: +98-91-6612-4162 Received: 5 January 2020; Accepted: 27 February 2020; Published: 11 March 2020 Simple Summary: Economics of feedlot beef production dictate that beef cattle must gain weight at their maximum potential rate; this involves getting them quickly onto a full feed of high fermentable diet which can induce the ruminal acidosis disease. The molecular host mechanisms that occur as a response to the acidosis, are mostly unknown. For answering this question, the rumen epithelial transcriptome in acidosis and control fattening steers were obtained. By RNA sequencing we found the different expression profiles of genes in normal and acidosis induced steers. Then we constructed two metabolic networks for normal and acidosis tissue based on gene expression profile. Our results suggest that rapid shifts to diets rich in fermentable carbohydrates cause an increased concentration of ruminal volatile fatty acids (VFA) and toxins and significant changes in transcriptome profiles and metabolites of rumen epithelial tissue, with negative effects on economic consequences of poor performance and animal health. -

(12) Patent Application Publication (10) Pub. No.: US 2012/0266329 A1 Mathur Et Al
US 2012026.6329A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2012/0266329 A1 Mathur et al. (43) Pub. Date: Oct. 18, 2012 (54) NUCLEICACIDS AND PROTEINS AND CI2N 9/10 (2006.01) METHODS FOR MAKING AND USING THEMI CI2N 9/24 (2006.01) CI2N 9/02 (2006.01) (75) Inventors: Eric J. Mathur, Carlsbad, CA CI2N 9/06 (2006.01) (US); Cathy Chang, San Marcos, CI2P 2L/02 (2006.01) CA (US) CI2O I/04 (2006.01) CI2N 9/96 (2006.01) (73) Assignee: BP Corporation North America CI2N 5/82 (2006.01) Inc., Houston, TX (US) CI2N 15/53 (2006.01) CI2N IS/54 (2006.01) CI2N 15/57 2006.O1 (22) Filed: Feb. 20, 2012 CI2N IS/60 308: Related U.S. Application Data EN f :08: (62) Division of application No. 1 1/817,403, filed on May AOIH 5/00 (2006.01) 7, 2008, now Pat. No. 8,119,385, filed as application AOIH 5/10 (2006.01) No. PCT/US2006/007642 on Mar. 3, 2006. C07K I4/00 (2006.01) CI2N IS/II (2006.01) (60) Provisional application No. 60/658,984, filed on Mar. AOIH I/06 (2006.01) 4, 2005. CI2N 15/63 (2006.01) Publication Classification (52) U.S. Cl. ................... 800/293; 435/320.1; 435/252.3: 435/325; 435/254.11: 435/254.2:435/348; (51) Int. Cl. 435/419; 435/195; 435/196; 435/198: 435/233; CI2N 15/52 (2006.01) 435/201:435/232; 435/208; 435/227; 435/193; CI2N 15/85 (2006.01) 435/200; 435/189: 435/191: 435/69.1; 435/34; CI2N 5/86 (2006.01) 435/188:536/23.2; 435/468; 800/298; 800/320; CI2N 15/867 (2006.01) 800/317.2: 800/317.4: 800/320.3: 800/306; CI2N 5/864 (2006.01) 800/312 800/320.2: 800/317.3; 800/322; CI2N 5/8 (2006.01) 800/320.1; 530/350, 536/23.1: 800/278; 800/294 CI2N I/2 (2006.01) CI2N 5/10 (2006.01) (57) ABSTRACT CI2N L/15 (2006.01) CI2N I/19 (2006.01) The invention provides polypeptides, including enzymes, CI2N 9/14 (2006.01) structural proteins and binding proteins, polynucleotides CI2N 9/16 (2006.01) encoding these polypeptides, and methods of making and CI2N 9/20 (2006.01) using these polynucleotides and polypeptides. -

All Enzymes in BRENDA™ the Comprehensive Enzyme Information System
All enzymes in BRENDA™ The Comprehensive Enzyme Information System http://www.brenda-enzymes.org/index.php4?page=information/all_enzymes.php4 1.1.1.1 alcohol dehydrogenase 1.1.1.B1 D-arabitol-phosphate dehydrogenase 1.1.1.2 alcohol dehydrogenase (NADP+) 1.1.1.B3 (S)-specific secondary alcohol dehydrogenase 1.1.1.3 homoserine dehydrogenase 1.1.1.B4 (R)-specific secondary alcohol dehydrogenase 1.1.1.4 (R,R)-butanediol dehydrogenase 1.1.1.5 acetoin dehydrogenase 1.1.1.B5 NADP-retinol dehydrogenase 1.1.1.6 glycerol dehydrogenase 1.1.1.7 propanediol-phosphate dehydrogenase 1.1.1.8 glycerol-3-phosphate dehydrogenase (NAD+) 1.1.1.9 D-xylulose reductase 1.1.1.10 L-xylulose reductase 1.1.1.11 D-arabinitol 4-dehydrogenase 1.1.1.12 L-arabinitol 4-dehydrogenase 1.1.1.13 L-arabinitol 2-dehydrogenase 1.1.1.14 L-iditol 2-dehydrogenase 1.1.1.15 D-iditol 2-dehydrogenase 1.1.1.16 galactitol 2-dehydrogenase 1.1.1.17 mannitol-1-phosphate 5-dehydrogenase 1.1.1.18 inositol 2-dehydrogenase 1.1.1.19 glucuronate reductase 1.1.1.20 glucuronolactone reductase 1.1.1.21 aldehyde reductase 1.1.1.22 UDP-glucose 6-dehydrogenase 1.1.1.23 histidinol dehydrogenase 1.1.1.24 quinate dehydrogenase 1.1.1.25 shikimate dehydrogenase 1.1.1.26 glyoxylate reductase 1.1.1.27 L-lactate dehydrogenase 1.1.1.28 D-lactate dehydrogenase 1.1.1.29 glycerate dehydrogenase 1.1.1.30 3-hydroxybutyrate dehydrogenase 1.1.1.31 3-hydroxyisobutyrate dehydrogenase 1.1.1.32 mevaldate reductase 1.1.1.33 mevaldate reductase (NADPH) 1.1.1.34 hydroxymethylglutaryl-CoA reductase (NADPH) 1.1.1.35 3-hydroxyacyl-CoA -

(12) Patent Application Publication (10) Pub. No.: US 2015/0240226A1 Mathur Et Al
US 20150240226A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0240226A1 Mathur et al. (43) Pub. Date: Aug. 27, 2015 (54) NUCLEICACIDS AND PROTEINS AND CI2N 9/16 (2006.01) METHODS FOR MAKING AND USING THEMI CI2N 9/02 (2006.01) CI2N 9/78 (2006.01) (71) Applicant: BP Corporation North America Inc., CI2N 9/12 (2006.01) Naperville, IL (US) CI2N 9/24 (2006.01) CI2O 1/02 (2006.01) (72) Inventors: Eric J. Mathur, San Diego, CA (US); CI2N 9/42 (2006.01) Cathy Chang, San Marcos, CA (US) (52) U.S. Cl. CPC. CI2N 9/88 (2013.01); C12O 1/02 (2013.01); (21) Appl. No.: 14/630,006 CI2O I/04 (2013.01): CI2N 9/80 (2013.01); CI2N 9/241.1 (2013.01); C12N 9/0065 (22) Filed: Feb. 24, 2015 (2013.01); C12N 9/2437 (2013.01); C12N 9/14 Related U.S. Application Data (2013.01); C12N 9/16 (2013.01); C12N 9/0061 (2013.01); C12N 9/78 (2013.01); C12N 9/0071 (62) Division of application No. 13/400,365, filed on Feb. (2013.01); C12N 9/1241 (2013.01): CI2N 20, 2012, now Pat. No. 8,962,800, which is a division 9/2482 (2013.01); C07K 2/00 (2013.01); C12Y of application No. 1 1/817,403, filed on May 7, 2008, 305/01004 (2013.01); C12Y 1 1 1/01016 now Pat. No. 8,119,385, filed as application No. PCT/ (2013.01); C12Y302/01004 (2013.01); C12Y US2006/007642 on Mar. 3, 2006.