THE DEVELOPMENT of NEUROLOGY in BELFAST by H
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
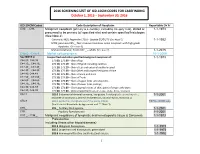
2016 SCREENING LIST of ICD-10CM CODES for CASEFINDING October 1, 2015 – September 30, 2016
2016 SCREENING LIST OF ICD-10CM CODES FOR CASEFINDING October 1, 2015 – September 30, 2016 ICD-10-CM Codes Code Description of Neoplasm Reportable Dx Yr C00._- C96._ Malignant neoplasm (primary & secondary; excluding category C44), stated or 1-1-1973 presumed to be primary (of specified site) and certain specified histologies (See Note 2) Carcinoid, NOS; Appendix C18.0 - Update 01/01/15 (See Note 5) 1-1-1992 MCN; pancreas C25._; Non-invasive mucinous cystic neoplasm with high grade dysplasia. (See note 6) Mature teratoma; Testis C62._ – adults (See note 7) 1-1-2015 C4a.0_-C4a.9_ Merkel cell carcinoma 10-1-2009 See NOTE 4 Unspecified and other specified malignant neoplasm of : 1-1-1973 C44.00.-C44.09 173.00, 173.09 – Skin of Lip C44.10_, C44.19_ 173.10, 173.19 – Skin of Eyelid including canthus C44.20_, C44.29_ 173. 20, 173.29 – Skin of Ear and external auditory canal C44.30_, C44.39_ 173.30, 173.39 – Skin Other and unspecified parts of face C44.40, C44.49 173. 40, 173.49 – Skin of Scalp and neck C44.50_, C44.59_ 173.50, 173.59 – Skin of Trunk C44.60_, C44.69_ 173. 60, 173.69 – Skin of Upper limb and shoulder, C44.70_, C44.79_ 173.70, 173.79 – Skin of Lower limb and hip; C44.80, C44.89 173.80, 173.89 – Overlapping lesions of skin, point of origin unknown; C44.90, C44.99 173.90, 173.99 - Sites unspecified (excludes Labia, Vulva, Penis, Scrotum) C54.1 182.0 Endometrial stromal sarcoma, low grade; Endolymphatic stromal myosis ; 1-1-2001 Endometrial stromatosis, Stromal endometriosis, Stromal myosis, NOS (C54.1) C56.9 183.0 Borderline malignancies -

Scientific and Medical Aspects of Apheresis: Issues and Evidence 3 ● Scientific and Medical Aspects of Apheresis: Issues and Evidence
3 Scientific and Medical Aspects of Apheresis: Issues and Evidence 3 ● Scientific and Medical Aspects of Apheresis: Issues and Evidence Various types of apheresis procedures have paucity of high-quality research, conclusions been performed on a clinical basis for many years, about the safety, efficacy, and effectiveness of but the number of patients and types of diseases apheresis are necessarily limited, although some treated have risen significantly in the last 5 years. tentative conclusions and directions for treatment This increase is partially due to increased under- can be discerned. standing of the disease and partially due to engi- The present chapter analyzes the methodolog- neering advances in equipment technologies. By ical problems in conducting apheresis research and almost any standard, treatment by apheresis is still examines available evidence of the safety, ef- in relatively early stages of development—there ficacy, and effectiveness of apheresis. Following are no ideal protocols based on a thorough un- a discussion of methodological issues, several derstanding of reasons for its efficacy. Never- major reviews of apheresis research will be sum- theless, there is an increasing flow of clinical data, marized and evaluated. This chapter will further sometimes describing dramatic patient improve- include the findings of a primary literature review ment, supporting the view that apheresis is a and assessment of apheresis in the treatment of rapidly emerging technology with significant three diseases—namely, hemolytic uremic syn- promise (117). Such evidence of treatment effec- drome, acquired Factor-VIII inhibitor, and Guil- tiveness’ is even today, however, often based on lain-Barré syndrome— where preliminary reports unsystematically collected data. -
LIST of OCCUPATIONAL DISEASES (Revised 2010)
LIST OF OCCUPATIONAL DISEASES (revised 2010) Identification and recognition of occupational diseases: Criteria for incorporating diseases in the ILO list of occupational diseases Occupational Safety and Health Series, No. 74 List of occupational diseases (revised 2010) Identification and recognition of occupational diseases: Criteria for incorporating diseases in the ILO list of occupational diseases INTERNATIONAL LABOUR OFFICE • GENEVA Copyright © International Labour Organization 2010 First published 2010 Publications of the International Labour Office enjoy copyright under Protocol 2 of the Universal Copyright Convention. Nevertheless, short excerpts from them may be reproduced without authorization, on condition that the source is indicated. For rights of reproduction or translation, application should be made to ILO Publications (Rights and Permissions), International Labour Office, CH-1211 Geneva 22, Switzerland, or by email: pubdroit@ ilo.org. The International Labour Office welcomes such applications. Libraries, institutions and other users registered with reproduction rights organizations may make copies in accordance with the licences issued to them for this purpose. Visit www.ifrro.org to find the reproduction rights organization in your country. ILO List of occupational diseases (revised 2010). Identification and recognition of occupational diseases: Criteria for incorporating diseases in the ILO list of occupational diseases Geneva, International Labour Office, 2010 (Occupational Safety and Health Series, No. 74) occupational disease / definition. 13.04.3 ISBN 978-92-2-123795-2 ISSN 0078-3129 Also available in French: Liste des maladies professionnelles (révisée en 2010): Identification et reconnaissance des maladies professionnelles: critères pour incorporer des maladies dans la liste des maladies professionnelles de l’OIT (ISBN 978-92-2-223795-1, ISSN 0250-412x), Geneva, 2010, and in Spanish: Lista de enfermedades profesionales (revisada en 2010). -

ICD-10 International Statistical Classification of Diseases and Related Health Problems
ICD-10 International Statistical Classification of Diseases and Related Health Problems 10th Revision Volume 2 Instruction manual 2010 Edition WHO Library Cataloguing-in-Publication Data International statistical classification of diseases and related health problems. - 10th revision, edition 2010. 3 v. Contents: v. 1. Tabular list – v. 2. Instruction manual – v. 3. Alphabetical index. 1.Diseases - classification. 2.Classification. 3.Manuals. I.World Health Organization. II.ICD-10. ISBN 978 92 4 154834 2 (NLM classification: WB 15) © World Health Organization 2011 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press through the WHO web site (http://www.who.int/about/licensing/copyright_form). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

FAQ REGARDING DISEASE REPORTING in MONTANA | Rev
Disease Reporting in Montana: Frequently Asked Questions Title 50 Section 1-202 of the Montana Code Annotated (MCA) outlines the general powers and duties of the Montana Department of Public Health & Human Services (DPHHS). The three primary duties that serve as the foundation for disease reporting in Montana state that DPHHS shall: • Study conditions affecting the citizens of the state by making use of birth, death, and sickness records; • Make investigations, disseminate information, and make recommendations for control of diseases and improvement of public health to persons, groups, or the public; and • Adopt and enforce rules regarding the reporting and control of communicable diseases. In order to meet these obligations, DPHHS works closely with local health jurisdictions to collect and analyze disease reports. Although anyone may report a case of communicable disease, such reports are submitted primarily by health care providers and laboratories. The Administrative Rules of Montana (ARM), Title 37, Chapter 114, Communicable Disease Control, outline the rules for communicable disease control, including disease reporting. Communicable disease surveillance is defined as the ongoing collection, analysis, interpretation, and dissemination of disease data. Accurate and timely disease reporting is the foundation of an effective surveillance program, which is key to applying effective public health interventions to mitigate the impact of disease. What diseases are reportable? A list of reportable diseases is maintained in ARM 37.114.203. The list continues to evolve and is consistent with the Council of State and Territorial Epidemiologists (CSTE) list of Nationally Notifiable Diseases maintained by the Centers for Disease Control and Prevention (CDC). In addition to the named conditions on the list, any occurrence of a case/cases of communicable disease in the 20th edition of the Control of Communicable Diseases Manual with a frequency in excess of normal expectancy or any unusual incident of unexplained illness or death in a human or animal should be reported. -

Blood and Immunity
Chapter Ten BLOOD AND IMMUNITY Chapter Contents 10 Pretest Clinical Aspects of Immunity Blood Chapter Review Immunity Case Studies Word Parts Pertaining to Blood and Immunity Crossword Puzzle Clinical Aspects of Blood Objectives After study of this chapter you should be able to: 1. Describe the composition of the blood plasma. 7. Identify and use roots pertaining to blood 2. Describe and give the functions of the three types of chemistry. blood cells. 8. List and describe the major disorders of the blood. 3. Label pictures of the blood cells. 9. List and describe the major disorders of the 4. Explain the basis of blood types. immune system. 5. Define immunity and list the possible sources of 10. Describe the major tests used to study blood. immunity. 11. Interpret abbreviations used in blood studies. 6. Identify and use roots and suffixes pertaining to the 12. Analyse several case studies involving the blood. blood and immunity. Pretest 1. The scientific name for red blood cells 5. Substances produced by immune cells that is . counteract microorganisms and other foreign 2. The scientific name for white blood cells materials are called . is . 6. A deficiency of hemoglobin results in the disorder 3. Platelets, or thrombocytes, are involved in called . 7. A neoplasm involving overgrowth of white blood 4. The white blood cells active in adaptive immunity cells is called . are the . 225 226 ♦ PART THREE / Body Systems Other 1% Proteins 8% Plasma 55% Water 91% Whole blood Leukocytes and platelets Formed 0.9% elements 45% Erythrocytes 10 99.1% Figure 10-1 Composition of whole blood. -
History of the Statistical Classification of Diseases and Causes of Death
Copyright information All material appearing in this report is in the public domain and may be reproduced or copied without permission; citation as to source, however, is appreciated. Suggested citation Moriyama IM, Loy RM, Robb-Smith AHT. History of the statistical classification of diseases and causes of death. Rosenberg HM, Hoyert DL, eds. Hyattsville, MD: National Center for Health Statistics. 2011. Library of Congress Cataloging-in-Publication Data Moriyama, Iwao M. (Iwao Milton), 1909-2006, author. History of the statistical classification of diseases and causes of death / by Iwao M. Moriyama, Ph.D., Ruth M. Loy, MBE, A.H.T. Robb-Smith, M.D. ; edited and updated by Harry M. Rosenberg, Ph.D., Donna L. Hoyert, Ph.D. p. ; cm. -- (DHHS publication ; no. (PHS) 2011-1125) “March 2011.” Includes bibliographical references. ISBN-13: 978-0-8406-0644-0 ISBN-10: 0-8406-0644-3 1. International statistical classification of diseases and related health problems. 10th revision. 2. International statistical classification of diseases and related health problems. 11th revision. 3. Nosology--History. 4. Death- -Causes--Classification--History. I. Loy, Ruth M., author. II. Robb-Smith, A. H. T. (Alastair Hamish Tearloch), author. III. Rosenberg, Harry M. (Harry Michael), editor. IV. Hoyert, Donna L., editor. V. National Center for Health Statistics (U.S.) VI. Title. VII. Series: DHHS publication ; no. (PHS) 2011- 1125. [DNLM: 1. International classification of diseases. 2. Disease-- classification. 3. International Classification of Diseases--history. 4. Cause of Death. 5. History, 20th Century. WB 15] RB115.M72 2011 616.07’8012--dc22 2010044437 For sale by the U.S. -

Neglected Diseases
Neglected Diseases What is a neglected disease? Why do we call these diseases neglected? How many people are affected by neglected diseases? What are some examples of neglected diseases? What can be done to prevent neglected diseases? How can neglected diseases be treated? Where can people get more information about neglected diseases? What is a neglected disease? Neglected diseases are conditions that inflict severe health burdens on the world’s poorest people. Many of these conditions are infectious diseases that are most prevalent in tropical climates, particularly in areas with unsafe drinking water, poor sanitation, substandard housing and little or no access to health care. Why do we call these diseases neglected? Diseases are said to be neglected if they are often overlooked by drug developers or by others instrumental in drug access, such as government officials, public health programs and the news media. Typically, private pharmaceutical companies cannot recover the cost of developing and producing treatments for these diseases. Another reason neglected diseases are not considered high priorities for prevention or treatment is because they usually do not affect people who live in the United States and other developed nations. Neglected diseases also lack visibility because they usually do not cause dramatic outbreaks that kill large numbers of people. Rather, such diseases usually exact their toll over a longer period of time, leading to crippling deformities, severe disabilities and/or relatively slow deaths. How many people are affected by neglected diseases? The World Health Organization (WHO) estimates that more than 1 billion people -- one- sixth of the world’s population -- suffer from one or more neglected diseases. -
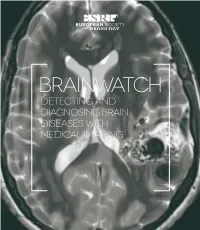
Detecting and Diagnosing Brain Diseases with Medical Imaging Table of Contents 3 Brainwatch Table of Contents
BRAINWATCH DETECTING AND diaGNOSING braiN diSEASES with MEdicaL IMAGING tabLE OF CONTENTS 3 brainwatch tabLE OF CONTENTS INTRODUCTIOn: What IS A NEUROradiOLOGIST? .................. 4 1 Imaging brain tumours: The neuroradiologist as the central chair on the brain tumour board .............................................................................9 2 Advanced imaging techniques in the diagnosis of dementia: from structure to function and back again ....................................................................................................................................17 3 Magnetic resonance imaging in the diagnosis of multiple sclerosis ...............................................................................................23 4 Magnetic resonance imaging in the diagnosis and treatment of Parkinson’s disease ......................................31 5 Radiotherapy of brain malignancies ...........................................39 6 Neuroimaging research ..................................................................................... 47 7 The patient’s view on brain imaging: European Federation of Neurological Associations .......................57 8 The Patient’s view on brain imaging: Austrian Self-Help Association ...........................................................................................65 9 Authors ..........................................................................................................................................71 photocredits ............................................................................................................................. -

The Spectrum of Autoimmune Diseases
Sarah Ballantyne, PhD 1717 The Spectrum of Autoimmune Diseases The following is a list of diseases that are either confirmed autoimmune diseases or for which there is very strong scientific evidence for autoimmune origins: Acute brachial neuropathy (also Atrophic polychondritis (also known Besnier-Boeck disease (also known A known as acute brachial radiculitis, as systemic chondromalacia and as sarcoidosis) neuralgic amyotrophy, brachial relapsing polychondritis) Bickerstaff’s encephalitis neuritis, brachial plexus neuropathy, Autoimmune angioedema Bladder pain syndrome (also known brachial plexitis, and Parsonage- Autoimmune aplastic anemia (also as interstitial cystitis) Turner syndrome) known as aplastic anemia) Brachial neuritis (also known as Acute disseminated Autoimmune cardiomyopathy brachial plexus neuropathy, brachial encephalomyelitis (ADEM) Autoimmune dysautonomia plexitis, Parsonage-Turner syndrome, Acute necrotizing hemorrhagic acute brachial neuropathy, acute Autoimmune hemolytic anemia leukoencephalitis brachial radiculitis, and neuralgic Acute parapsoriasis (also known as Autoimmune hepatitis amyotrophy) acute guttate parapsoriasis, acute Autoimmune hyperlipidemia Bullous pemphigoid pityriasis lichenoides, parapsoriasis Autoimmune immunodeficiency Castleman’s disease (also varioliformis, Mucha-Habermann C known as giant lymph node disease, and parapsoriasis or Autoimmune inner ear disease hyperplasia, lymphoid hamartoma, pityriasis lichenoides et varioliformis (AIED) and angiofollicular lymph node acuta) Autoimmune myocarditis -

Prevalence and Incidence of Rare Diseases
Number 2 | January 2019 Prevalence and incidence of rare diseases: Bibliographic data Diseases listed by decreasing prevalence, incidence or number of published cases www.orpha.net www.orphadata.org prevalence or incidence. Methodology When a range of data sources is available, the most recent data source that meets a certain number of quality criteria Orphanet carries out a systematic survey of literature in is favoured (registries, meta-analyses, population-based order to estimate the prevalence and incidence of rare studies, large cohorts studies). diseases. This study aims to collect new data regarding point prevalence, birth prevalence and incidence, and to For congenital diseases, the prevalence is estimated, so update already published data according to new scientific that: studies or other available data. Prevalence = birth prevalence x (patient life expectancy/general population life expectancy). This data is presented in the following reports published biannually: When only incidence data is documented, the prevalence • Prevalence, incidence or number of published cases is estimated when possible, so that : listed by diseases (in alphabetical order) ; • Diseases listed by decreasing prevalence, incidence or Prevalence = incidence x disease mean duration. number of published cases ; When neither prevalence nor incidence data is available, Data collection which is the case for very rare diseases, the number of cases or families documented in the medical literature is A number of different sources are used : provided. Limitations of the study Registries (RARECARE, EUROCAT, etc) ; The prevalence and incidence data presented in this report National/international health institutes and agencies are only estimations and cannot be considered to be (Institut National de Veille Sanitaire (French Institute absolutely correct. -
Commission Implementing Decision (Eu) 2018
6.7.2018 EN Official Journal of the European Union L 170/1 II (Non-legislative acts) DECISIONS COMMISSION IMPLEMENTING DECISION (EU) 2018/945 of 22 June 2018 on the communicable diseases and related special health issues to be covered by epidemiological surveillance as well as relevant case definitions (Text with EEA relevance) THE EUROPEAN COMMISSION, Having regard to the Treaty on the Functioning of the European Union, Having regard to Decision No 1082/2013/EU of the European Parliament and of the Council of 22 October 2013 on serious cross-border threats to health and repealing Decision No 2119/98/EC (1), and in particular Article 6(5)(a) and (b) thereof, Whereas: (1) Pursuant to Decision No 2119/98/EC of the European Parliament and of the Council (2), Commission Decision 2000/96/EC (3) established a list of communicable diseases and special health issues to be covered by epidemiological surveillance in the Community network. (2) Commission Decision 2002/253/EC (4) laid down case definitions for reporting communicable diseases listed in Decision 2000/96/EC to the Community network. (3) The Annex to Decision No 1082/2013/EU sets out the criteria for selecting the communicable diseases and related special health issues to be covered by epidemiological surveillance within the network. (4) The list of diseases and related special health issues established by Decision 2000/96/EC should be updated to reflect changes in disease incidence and prevalence, the needs of the European Union and its Member States, as well as to ensure compliance with the criteria provided in the Annex to Decision No 1082/2013/EU.