Autoimmune Encephalitis in Critical Care: Optimizing Immunosuppression
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Café Au Lait Spots As a Marker of Neuropaediatric Diseases
Mini Review Open Access J Neurol Neurosurg Volume 3 Issue 5 - May 2017 DOI: 10.19080/OAJNN.2017.03.555622 Copyright © All rights are reserved by Francisco Carratalá-Marco Café Au Lait Spots as a Marker of Neuropaediatric Diseases Francisco Carratalá-Marco1*, Rosa María Ruiz-Miralles2, Patricia Andreo-Lillo1, Julia Dolores Miralles-Botella3, Lorena Pastor-Ferrándiz1 and Mercedes Juste-Ruiz2 1Neuropaediatric Unit, University Hospital of San Juan de Alicante, Spain 2Paediatric Department, University Hospital of San Juan de Alicante, Spain 3Dermatology Department, University Hospital of San Juan de Alicante, Spain Submission: March 22, 2017; Published: May 10, 2017 *Corresponding author: Francisco Carratalá-Marco, Neuropaediatric Unit, University Hospital of San Juan de Alicante, Spain, Tel: ; Email: Abstract Introduction: want to know in which The measure,Café au lait the spots presence (CALS) of isolated are shown CALS in representsthe normal a population risk factor forwithout neurological pathological disease. significance, although they could also be criteria for some neurologic syndromes. Unspecific association with general neurologic illnesses has been less frequently described. We Patients and methods: We set up an observational transversal study of cases, patients admitted for neuropaediatric reasons (NPP; n=49) excluding all the patients suffering from neurologic illnesses associated to CALS, and controls, a hospital simultaneously admitted pediatric population for non-neurologic causes (CP; n=101) since October 2012 to January 2013. The data were collected from the clinical reports at admission, and then analyzed by SPSS 22.0 statistical package, and the Stat Calc module of EpiInfo 7.0, following the ethics current rules of the institution for observational studies. -

Do the Lifetime Prevalence and Prognosis of Schizophrenia Differ Among World Regions? Cheryl Lynn Smith
Claremont Colleges Scholarship @ Claremont CMC Senior Theses CMC Student Scholarship 2018 Do the Lifetime Prevalence and Prognosis of Schizophrenia Differ Among World Regions? Cheryl Lynn Smith Recommended Citation Smith, Cheryl Lynn, "Do the Lifetime Prevalence and Prognosis of Schizophrenia Differ Among World Regions?" (2018). CMC Senior Theses. 1978. http://scholarship.claremont.edu/cmc_theses/1978 This Open Access Senior Thesis is brought to you by Scholarship@Claremont. It has been accepted for inclusion in this collection by an authorized administrator. For more information, please contact [email protected]. Do the Lifetime Prevalence and Prognosis of Schizophrenia Differ Among World Regions? A Thesis Presented by Cheryl Lynn Smith To the Keck Science Department Of Claremont McKenna, Pitzer, and Scripps Colleges In partial fulfillment of The degree of Bachelor of Arts Senior Thesis in Human Biology 04/23/2018 LIFETIME PREVALENCE AND PROGNOSIS OF SCHIZOPHRENIA 1 Table of Contents Abstract …………………………………………………………...……………………… 2 1. Introduction………………………………………………...…………...……………… 3 2. Background Information ……………………………...……………………………….. 5 2.1 Historical Background of Schizophrenia ……………………....…………… 5 2.2 Lifetime Prevalence of Schizophrenia …………………………...…..……… 12 2.3 Prognosis in People with Schizophrenia ……………....………...…..……… 13 3. Methods …………………………………………...……………………..……………. 17 4. Results ……………………………………………...…………………….…….…….... 18 5. Discussion ……………………………………………...……………………………… 24 6. Acknowledgements …………………………………………...………………………. -

Diseases/Symptoms Reported to Be Associated with Lyme Disease
Diseases/Symptoms Reported to be Associated with Lyme Disease Abdominal pseudo-eventration Abdominal wall weakness Acrodermatitis chronica atrophicans (ACA) Acute Acral Ischemia Acute conduction disorders Acute coronary syndrome Acute exogenous psychosis Acute febrile illness Acute hemiparesis Acute ischaemic pontine stroke Acute meningitis Acute myelo-meningo-radiculitis Acute myelitis Acute pediatric monoarticular arthritis Acute peripheral facial palsy Acute perimyocarditis Acute posterior multifocal placoid pigment epitheliopathy (APMPPE) Acute pyogenic arthritis Acute reversible diffuse conduction system disease Acute septic arthritis Acute severe encephalitis Acute transitory auriculoventricular block Acute transverse myelitis Acute urinary retention Acquired Immune Deficiency Syndrome (AIDS) Algodystrophy Allergic conditions Allergic conjunctivitis Alopecia Alzheimer’s Disease Amyotrophic lateral sclerosis (ALS - Lou Gehrig's Disease) Amyotrophy Anamnesis Anetoderma Anorexia nervosa Anterior optic neuropathy Antepartum fever Anxiety Arrhythmia Arthralgia Arthritis Asymmetrical hearing loss Ataxic sensory neuropathy Atraumatic spontaneous hemarthrosis Atrioventricular block Attention Deficit Disorder (ADD) Attention Deficit Hyperactivity Disorder (ADHD) Back pain without radiculitis Bannwarth’s Syndrome Behcet's disease Bell’s Palsy Benign cutaneous lymphocytoma Benign lymphocytic infiltration (Jessner-Kanof) Bilateral acute confluent disseminated choroiditis Bilateral carpal tunnel syndrome Bilateral facial nerve palsy Bilateral -

ICD-10-CM TABULAR LIST of DISEASES and INJURIES 2018 Addenda No Change Chapter 1 No Change Certain Infectious and Parasitic Diseases (A00-B99)
ICD-10-CM TABULAR LIST of DISEASES and INJURIES 2018 Addenda No Change Chapter 1 No Change Certain infectious and parasitic diseases (A00-B99) No Change Intestinal infectious diseases (A00-A09) No Change A04 Other bacterial intestinal infections No Change A04.7 Enterocolitis due to Clostridium difficile Add A04.71 Enterocolitis due to Clostridium difficile, recurrent Add A04.72 Enterocolitis due to Clostridium difficile, not specified as recurrent No Change A05 Other bacterial foodborne intoxications, not elsewhere classified No Change Excludes1: Revise from Clostridium difficile foodborne intoxication and infection (A04.7) Revise to Clostridium difficile foodborne intoxication and infection (A04.7-) No Change Helminthiases (B65-B83) No Change B81 Other intestinal helminthiases, not elsewhere classified No Change Excludes1: Revise from angiostrongyliasis due to Parastrongylus cantonensis (B83.2) Revise to angiostrongyliasis due to: Add Angiostrongylus cantonensis (B83.2) Add Parastrongylus cantonensis (B83.2) No Change B81.3 Intestinal angiostrongyliasis Revise from Angiostrongyliasis due to Parastrongylus costaricensis Revise to Angiostrongyliasis due to: Add Angiostrongylus costaricensis Add Parastrongylus costaricensis No Change Chapter 2 No Change Neoplasms (C00-D49) No Change Malignant neoplasms of ill-defined, other secondary and unspecified sites (C76-C80) No Change C79 Secondary malignant neoplasm of other and unspecified sites Delete Excludes2: lymph node metastases (C77.0) No Change C79.1 Secondary malignant neoplasm of bladder -

EFFECTIVE NEBRASKA DEPARTMENT of 01/01/2017 HEALTH and HUMAN SERVICES 173 NAC 1 I TITLE 173 COMMUNICABLE DISEASES CHAPTER 1
EFFECTIVE NEBRASKA DEPARTMENT OF 01/01/2017 HEALTH AND HUMAN SERVICES 173 NAC 1 TITLE 173 COMMUNICABLE DISEASES CHAPTER 1 REPORTING AND CONTROL OF COMMUNICABLE DISEASES TABLE OF CONTENTS SECTION SUBJECT PAGE 1-001 SCOPE AND AUTHORITY 1 1-002 DEFINITIONS 1 1-003 WHO MUST REPORT 2 1-003.01 Healthcare Providers (Physicians and Hospitals) 2 1-003.01A Reporting by PA’s and APRN’s 2 1-003.01B Reporting by Laboratories in lieu of Physicians 3 1-003.01C Reporting by Healthcare Facilities in lieu of Physicians for 3 Healthcare Associated Infections (HAIs) 1-003.02 Laboratories 3 1-003.02A Electronic Ordering of Laboratory Tests 3 1-004 REPORTABLE DISEASES, POISONINGS, AND ORGANISMS: 3 LISTS AND FREQUENCY OF REPORTS 1-004.01 Immediate Reports 4 1-004.01A List of Diseases, Poisonings, and Organisms 4 1-004.01B Clusters, Outbreaks, or Unusual Events, Including Possible 5 Bioterroristic Attacks 1-004.02 Reports Within Seven Days – List of Reportable Diseases, 5 Poisonings, and Organisms 1-004.03 Reporting of Antimicrobial Susceptibility 8 1-004.04 New or Emerging Diseases and Other Syndromes and Exposures – 8 Reporting and Submissions 1-004.04A Criteria 8 1-004.04B Surveillance Mechanism 8 1-004.05 Sexually Transmitted Diseases 9 1-004.06 Healthcare Associated Infections 9 1-005 METHODS OF REPORTING 9 1-005.01 Health Care Providers 9 1-005.01A Immediate Reports of Diseases, Poisonings, and Organisms 9 1-005.01B Immediate Reports of Clusters, Outbreaks, or Unusual Events, 9 Including Possible Bioterroristic Attacks i EFFECTIVE NEBRASKA DEPARTMENT OF -

Preventable Diseases Nick Wilson, Michael G Baker Abstract New Zealanders Can Now Reflect on and Celebrate 50 Years of Polio Elimination in This Country
THE NEW ZEALAND MEDICAL JOURNAL Journal of the New Zealand Medical Association Celebrating 50 years of polio elimination in New Zealand: but inadequate progress in eliminating other vaccine- preventable diseases Nick Wilson, Michael G Baker Abstract New Zealanders can now reflect on and celebrate 50 years of polio elimination in this country. This success was followed by eliminating two other infectious diseases, brucellosis and hydatids, and an imported potential disease vector, the southern saltmarsh mosquito. However, this country has made inadequate progress in eliminating several other vaccine-preventable diseases. These include measles, mumps, and rubella, which are priority candidates for elimination, and potentially Hib disease and rotavirus infection. To achieve such successes almost certainly requires that the country: (i) builds national leadership for elimination goals; (ii) develops detailed plans; (iii) continues recent successes in enhancing routine vaccination coverage; (iv) introduces rotavirus vaccine into the childhood immunisation schedule; and (v) strengthens surveillance and research (on such questions as the cost-effectiveness of new vaccines, measures to enhance uptake, and effective border controls to reduce the risk of disease importation). For 50 years now (since 1 April 1962), New Zealand has been free of transmission of wild-type polio virus infection. The end of this disease was particularly sudden with cases declining from 214 notifications in an outbreak in 1961 (with seven deaths) to only five cases in early 1962. 1 The end coincided with mass immunisation campaigns with the new Sabin (oral) vaccine in 1961 and 1962. The coverage in the vaccination campaign running from April to June 1962 was approximately 95% of the child population up to school leaving age. -
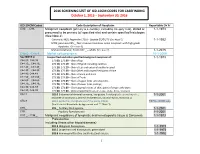
2016 SCREENING LIST of ICD-10CM CODES for CASEFINDING October 1, 2015 – September 30, 2016
2016 SCREENING LIST OF ICD-10CM CODES FOR CASEFINDING October 1, 2015 – September 30, 2016 ICD-10-CM Codes Code Description of Neoplasm Reportable Dx Yr C00._- C96._ Malignant neoplasm (primary & secondary; excluding category C44), stated or 1-1-1973 presumed to be primary (of specified site) and certain specified histologies (See Note 2) Carcinoid, NOS; Appendix C18.0 - Update 01/01/15 (See Note 5) 1-1-1992 MCN; pancreas C25._; Non-invasive mucinous cystic neoplasm with high grade dysplasia. (See note 6) Mature teratoma; Testis C62._ – adults (See note 7) 1-1-2015 C4a.0_-C4a.9_ Merkel cell carcinoma 10-1-2009 See NOTE 4 Unspecified and other specified malignant neoplasm of : 1-1-1973 C44.00.-C44.09 173.00, 173.09 – Skin of Lip C44.10_, C44.19_ 173.10, 173.19 – Skin of Eyelid including canthus C44.20_, C44.29_ 173. 20, 173.29 – Skin of Ear and external auditory canal C44.30_, C44.39_ 173.30, 173.39 – Skin Other and unspecified parts of face C44.40, C44.49 173. 40, 173.49 – Skin of Scalp and neck C44.50_, C44.59_ 173.50, 173.59 – Skin of Trunk C44.60_, C44.69_ 173. 60, 173.69 – Skin of Upper limb and shoulder, C44.70_, C44.79_ 173.70, 173.79 – Skin of Lower limb and hip; C44.80, C44.89 173.80, 173.89 – Overlapping lesions of skin, point of origin unknown; C44.90, C44.99 173.90, 173.99 - Sites unspecified (excludes Labia, Vulva, Penis, Scrotum) C54.1 182.0 Endometrial stromal sarcoma, low grade; Endolymphatic stromal myosis ; 1-1-2001 Endometrial stromatosis, Stromal endometriosis, Stromal myosis, NOS (C54.1) C56.9 183.0 Borderline malignancies -

Fusion of Multiple Heterogeneous Networks for Predicting Circrna
www.nature.com/scientificreports OPEN Fusion of multiple heterogeneous networks for predicting circRNA- disease associations Received: 22 January 2019 Lei Deng1, Wei Zhang1, Yechuan Shi1 & Yongjun Tang2 Accepted: 18 June 2019 Circular RNAs (circRNAs) are a newly identifed type of non-coding RNA (ncRNA) that plays crucial roles Published: xx xx xxxx in many cellular processes and human diseases, and are potential disease biomarkers and therapeutic targets in human diseases. However, experimentally verifed circRNA-disease associations are very rare. Hence, developing an accurate and efcient method to predict the association between circRNA and disease may be benefcial to disease prevention, diagnosis, and treatment. Here, we propose a computational method named KATZCPDA, which is based on the KATZ method and the integrations among circRNAs, proteins, and diseases to predict circRNA-disease associations. KATZCPDA not only verifes existing circRNA-disease associations but also predicts unknown associations. As demonstrated by leave-one-out and 10-fold cross-validation, KATZCPDA achieves AUC values of 0.959 and 0.958, respectively. The performance of KATZCPDA was substantially higher than those of previously developed network-based methods. To further demonstrate the efectiveness of KATZCPDA, we apply KATZCPDA to predict the associated circRNAs of Colorectal cancer, glioma, breast cancer, and Tuberculosis. The results illustrated that the predicted circRNA-disease associations could rank the top 10 of the experimentally verifed associations. Circular RNA (circRNA) is a class of non-coding RNA recently discovered. Unlike linear RNA, circRNA forms a continuous cycle of covalent closures and is highly represented in the eukaryotic transcriptome. Previous research has found thousands of prototype circRNAs in human, mouse and nematode cells1–4. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Connecticut Insurance Coverage for Specialized Formula; New York's “Hannah's Law”
OLR RESEARCH REPORT July 5, 2012 2012-R-0304 CONNECTICUT INSURANCE COVERAGE FOR SPECIALIZED FORMULA; NEW YORK'S “HANNAH'S LAW” By: Janet L. Kaminski Leduc, Senior Legislative Attorney You asked if Connecticut law requires health insurance policies to cover specialized formula used for treating eosinophilic disorder. You also asked for a description of New York’s “Hannah’s Law.” SUMMARY Connecticut insurance law does not explicitly require health insurance policies to cover specialized formulas for treating eosinophilic disorder. However, the law requires specified health insurance policies to cover medically necessary specialized formula for children up to age 12 for treating a disease or condition when the formula is administered under a physician’s direction. Thus, it appears that this would include coverage of specialized formulas for treating eosinophilic disorder. Anyone denied such coverage may appeal to their insurance carrier (internal appeal) or the Insurance Department (external appeal). The explanation of benefits from the carrier describes the appeal process. Anyone with concerns or questions about his or her insurance coverage may contact the Insurance Department’s Consumer Affairs Division at (800) 203-3447 or (860) 297-3900. More information about contacting the department is available at http://www.ct.gov/cid/cwp/view.asp?q=254352. Sandra Norman-Eady, Director Room 5300 Phone (860) 240-8400 Legislative Office Building FAX (860) 240-8881 Connecticut General Assembly Hartford, CT 06106-1591 http://www.cga.ct.gov/olr Office of Legislative Research [email protected] A bill (“Hannah’s Law”) in the New York Assembly would require health insurance policies to cover the cost of enteral formulas for treating eosinophilic esophagitis and related eosinophilic disorders. -

Eye Disease 1 Eye Disease
Eye disease 1 Eye disease Eye disease Classification and external resources [1] MeSH D005128 This is a partial list of human eye diseases and disorders. The World Health Organisation publishes a classification of known diseases and injuries called the International Statistical Classification of Diseases and Related Health Problems or ICD-10. This list uses that classification. H00-H59 Diseases of the eye and adnexa H00-H06 Disorders of eyelid, lacrimal system and orbit • (H00.0) Hordeolum ("stye" or "sty") — a bacterial infection of sebaceous glands of eyelashes • (H00.1) Chalazion — a cyst in the eyelid (usually upper eyelid) • (H01.0) Blepharitis — inflammation of eyelids and eyelashes; characterized by white flaky skin near the eyelashes • (H02.0) Entropion and trichiasis • (H02.1) Ectropion • (H02.2) Lagophthalmos • (H02.3) Blepharochalasis • (H02.4) Ptosis • (H02.6) Xanthelasma of eyelid • (H03.0*) Parasitic infestation of eyelid in diseases classified elsewhere • Dermatitis of eyelid due to Demodex species ( B88.0+ ) • Parasitic infestation of eyelid in: • leishmaniasis ( B55.-+ ) • loiasis ( B74.3+ ) • onchocerciasis ( B73+ ) • phthiriasis ( B85.3+ ) • (H03.1*) Involvement of eyelid in other infectious diseases classified elsewhere • Involvement of eyelid in: • herpesviral (herpes simplex) infection ( B00.5+ ) • leprosy ( A30.-+ ) • molluscum contagiosum ( B08.1+ ) • tuberculosis ( A18.4+ ) • yaws ( A66.-+ ) • zoster ( B02.3+ ) • (H03.8*) Involvement of eyelid in other diseases classified elsewhere • Involvement of eyelid in impetigo -

Scientific and Medical Aspects of Apheresis: Issues and Evidence 3 ● Scientific and Medical Aspects of Apheresis: Issues and Evidence
3 Scientific and Medical Aspects of Apheresis: Issues and Evidence 3 ● Scientific and Medical Aspects of Apheresis: Issues and Evidence Various types of apheresis procedures have paucity of high-quality research, conclusions been performed on a clinical basis for many years, about the safety, efficacy, and effectiveness of but the number of patients and types of diseases apheresis are necessarily limited, although some treated have risen significantly in the last 5 years. tentative conclusions and directions for treatment This increase is partially due to increased under- can be discerned. standing of the disease and partially due to engi- The present chapter analyzes the methodolog- neering advances in equipment technologies. By ical problems in conducting apheresis research and almost any standard, treatment by apheresis is still examines available evidence of the safety, ef- in relatively early stages of development—there ficacy, and effectiveness of apheresis. Following are no ideal protocols based on a thorough un- a discussion of methodological issues, several derstanding of reasons for its efficacy. Never- major reviews of apheresis research will be sum- theless, there is an increasing flow of clinical data, marized and evaluated. This chapter will further sometimes describing dramatic patient improve- include the findings of a primary literature review ment, supporting the view that apheresis is a and assessment of apheresis in the treatment of rapidly emerging technology with significant three diseases—namely, hemolytic uremic syn- promise (117). Such evidence of treatment effec- drome, acquired Factor-VIII inhibitor, and Guil- tiveness’ is even today, however, often based on lain-Barré syndrome— where preliminary reports unsystematically collected data.