D40. Cerebrospinal Fluid.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Diagnosis of Subarachnoid Haemorrhage
Journal ofNeurology, Neurosurgery, and Psychiatry 1990;53:365-372 365 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.53.5.365 on 1 May 1990. Downloaded from OCCASIONAL REVIEW The diagnosis of subarachnoid haemorrhage M Vermeulen, J van Gijn Lumbar puncture (LP) has for a long time been of 55 patients with SAH who had LP, before the mainstay of diagnosis in patients who CT scanning and within 12 hours of the bleed. presented with symptoms or signs of subarach- Intracranial haematomas with brain shift was noid haemorrhage (SAH). At present, com- proven by operation or subsequent CT scan- puted tomography (CT) has replaced LP for ning in six of the seven patients, and it was this indication. In this review we shall outline suspected in the remaining patient who stop- the reasons for this change in diagnostic ped breathing at the end of the procedure.5 approach. In the first place, there are draw- Rebleeding may have occurred in some ofthese backs in starting with an LP. One of these is patients. that patients with SAH may harbour an We therefore agree with Hillman that it is intracerebral haematoma, even if they are fully advisable to perform a CT scan first in all conscious, and that withdrawal of cerebro- patients who present within 72 hours of a spinal fluid (CSF) may occasionally precipitate suspected SAH, even if this requires referral to brain shift and herniation. Another disadvan- another centre.4 tage of LP is the difficulty in distinguishing It could be argued that by first performing between a traumatic tap and true subarachnoid CT the diagnosis may be delayed and that this haemorrhage. -

Cerebrospinal Fluid in Critical Illness
Cerebrospinal Fluid in Critical Illness B. VENKATESH, P. SCOTT, M. ZIEGENFUSS Intensive Care Facility, Division of Anaesthesiology and Intensive Care, Royal Brisbane Hospital, Brisbane, QUEENSLAND ABSTRACT Objective: To detail the physiology, pathophysiology and recent advances in diagnostic analysis of cerebrospinal fluid (CSF) in critical illness, and briefly review the pharmacokinetics and pharmaco- dynamics of drugs in the CSF when administered by the intravenous and intrathecal route. Data Sources: A review of articles published in peer reviewed journals from 1966 to 1999 and identified through a MEDLINE search on the cerebrospinal fluid. Summary of review: The examination of the CSF has become an integral part of the assessment of the critically ill neurological or neurosurgical patient. Its greatest value lies in the evaluation of meningitis. Recent publications describe the availability of new laboratory tests on the CSF in addition to the conventional cell count, protein sugar and microbiology studies. Whilst these additional tests have improved our understanding of the pathophysiology of the critically ill neurological/neurosurgical patient, they have a limited role in providing diagnostic or prognostic information. The literature pertaining to the use of these tests is reviewed together with a description of the alterations in CSF in critical illness. The pharmacokinetics and pharmacodynamics of drugs in the CSF, when administered by the intravenous and the intrathecal route, are also reviewed. Conclusions: The diagnostic utility of CSF investigation in critical illness is currently limited to the diagnosis of an infectious process. Studies that have demonstrated some usefulness of CSF analysis in predicting outcome in critical illness have not been able to show their superiority to conventional clinical examination. -

CSF Xanthochromia
CSF Xanthochromia Pseudonyms – CSF bilirubin For investigation of suspected subarachnoid haemorrhage (SAH) in CT negative patients Xanthochromia is the yellow discoloration indicating the presence of bilirubin in CSF which appears as oxyhaemoglobin released from the breakdown of red blood cells following haemorrhage into the CSF is converted in vivo into bilirubin in a time‐dependent manner. A subarachnoid haemorrhage (SAH) is a spontaneous arterial bleeding into the subarachnoid space, usually from a cerebral aneurysm, and characterised by a severe sudden‐onset headache. The majority of positive cases are detected by computed tomography (CT) scanning but for those CT‐ negative patients presenting with a history suggestive of SAH the measurement of xanthochromia in CSF is advocated to detect those patients who actually have sustained a SAH and require treatment and to eliminate the possibility of SAH in the remainder without the need of confirmatory angiography. The CSF is collected by means of lumbar puncture (LP). For full interpretation of the result other CSF and blood tests must be collected at the same time – CSF protein and glucose; plasma glucose; and serum protein and bilirubin. General information CSF Xanthochromia sample collection kits are provided in the ACU (ORC) and AMU (Trafford) and also available from the Specimen Receptions at the laboratories at both sites. Concurrent samples should be requested for CSF protein and glucose, plasma glucose and serum LFTS (for protein and bilirubin) using the sample containers supplied. Collection container: CSF xanthochromia: White topped Universal container (In addition the following samples should be collected:‐ CSF glucose & protein: 1.2 mL fluoride‐EDTA glucose (Sarstedt yellow top) Serum protein & bilirubin: 4.9 mL SST (Sarstedt brown top) Plasma glucose: 2.7 mL fluoride‐EDTA glucose (Sarstedt yellow top) Type and volume of sample: 1 mL CSF requested, minimum 400 µL required for analysis Specimen transport/special precautions: A CSF Xanthochromia sample collection kit should be used. -
Thunderclap Headache and Subarachnoid Hemorrhage
Thunderclap Headache and Subarachnoid Hemorrhage W David Freeman, MD No conflicts of interest or disclosures Subarachnoid Hemorrhage Neurocrit Care. 2017 Sep;27(Suppl 1):116- 123. doi: 10.1007/s12028-017-0458-8. Objectives •Recognize the symptoms (thunderclap headache) and Subarachnoid signs of SAH Hemorrhage •Initiate workup for suspected SAH •Initial management of SAH patient Case • 39 year old woman presents with severe headache, uncertain time of onset, associated with nausea • PMH: long history of migraine headaches • Meds: • Reports taking ibuprofen prior to ED, with moderate improvement of headache • Taking warfarin for a pelvic DVT - year prior during pregnancy • Exam: sleepy, yet follows commands, left eye droop and dilated pupil, moving all extremities • BP 160/95 mmHg, RR 24/min, HR 98/min • Breathing shallow and rapid, airway protection uncertain Initial Checklist in Emergency Dept. ☐ Brain Imaging ☐ Labs: PT/PTT, CBC, electrolytes, BUN, Cr, troponin, toxicology screen ☐ 12 lead ECG ☐ Blood pressure goal established ☐ Consult neurosurgery ☐ Address hydrocephalus SAH Algorithm Neurocrit Care. 2017 Sep;27(Suppl 1):116- 123. doi: 10.1007/s12028-017-0458-8. SAH Symptoms and Signs CLASSIC NOT-SO-CLASSIC Abrupt onset of severe headache (HA), HA is not reported as abrupt (patient may i.e. thunderclap not remember event well) “Worst or first” headache of one’s life HA responds well to non-narcotic that is instantaneously maximal at onset analgesics (“thunderclap” after lightening strike) May have nausea, vomiting and neck pain HA -
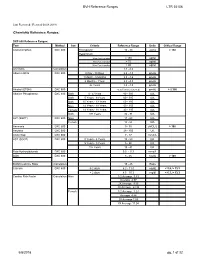
BVH Reference Ranges LTR 35106 Chemistry Reference Ranges
BVH Reference Ranges LTR 35106 Last Reviewed: (Revised 05.08.2018) Chemistry Reference Ranges: DXC 600 Reference Ranges: Test Method Sex Criteria Reference Range Units Critical Range Acetaminophen DXC 600 Therapeutic 10 - 30 ug/mL > 150 Hepatotoxic 4 hrs Post Ingestion > 150 ug/ml 8 hrs Post Ingestion > 75 ug/ml 12 hrs Post Ingestion > 40 ug/ml A/G Ratio Calculation 1.1 - 2.2 Albumin BCG DXC 600 0 Day - 30 Days 2.6 - 4.3 gm/dL 1 Month - 5 Months 2.8 - 4.6 gm/dL 6 Months - 1Year 2.8 - 4.8 gm/dL 2+ Years 3.2 - 4.9 gm/dL Alcohol (ETOH) DXC 600 <0.005 (none detected) gm/dL > 0.300 Alkaline Phosphatase DXC 600 Both 0 - 4 Years 80 - 350 IU/L Both 5 Years - 9 Years 60 - 385 IU/L Both 10 Years - 13 Years 60 - 485 IU/L Male 14 Years - 18 Years 50 - 350 IU/L Female 14 Years - 18 Years 40 - 195 IU/L Both 19+ Years 32 - 91 IU/L ALT (SGPT) DXC 600 Male 17 - 63 IU/L Female 14 - 54 IU/L Ammonia DXC 600 9 - 35 uMOL/L > 100 Amylase DXC 600 28 - 100 U/L Anion Gap DXC 600 7 - 17 mmol/L AST (SGOT) DXC 600 0 Years - 4 Years 10 - 60 IU/L 5 Years - 9 Years 5 - 50 IU/L 10+ Years 15 - 41 IU/L Beta Hydroxybutyrate DXC 600 0.0 - 0.3 mmol/L BUN DXC 600 8 - 26 mg/dL > 100 BUN/Creatinine Ratio Calculation 15 - 25 Ratio Calcium DXC 600 0-2 days 6.2 - 11.0 mg/dL < 5.8, > 13.3 > 2 days 8.5 - 10.3 mg/dl < 6.3, > 13.3 Cardiac Risk Factor Calculation Male 1/2 Average 3.43 Average 4.97 2X Average 9.55 3X Average 23.99 Female 1/2 Average 3.27 Average 4.44 2X Average 7.05 3X Average 11.04 5/8/2018 pg. -

Effect of Methemoglobin Formation on the MR Appearance of Subarachnoid Hemorrhage1
William G. Bradley, Jr., M.D., Ph.D. Effect of Methemoglobin Formation Paul G. Schmidt, Ph.D. on the MR Appearance of Subarachnoid Hemorrhage1 Subarachnoid hemorrhage has a much T HE EARLIEST reports of magnetic resonance (MR) images of in- higher intensity in magnetic resonance tracranial hemorrhage (1, 2) suggested a relatively intense ap- (MR) images with the passage of time. peanance of the hemorrhage relative to the surrounding brain. This Acute subarachnoid hemorrhage is diff i- was attributed to the short Ti relaxation time of the presumably cult to see; within 1 week its appearance paramagnetic, iron-containing hemoglobin. Figure 1 illustrates this has become intensified on Ti-weighted appearance in a patient imaged 1 week after rupture of an aneurysm images. Different concentrations of blood in an anterior communicating artery, with resulting intraparenchy- and lysed red blood cells in cerebrospinal mal hematoma and subarachnoid hemorrhage. The short Ti charac- fluid (CSF) were examined spectroscopi- ten of the injured area is enhanced relative to surrounding brain on cally but did not significantly alter Ti a Ti-weighted spin-echo image. and T2 relaxation of CSF acutely. Ultra- As experience was gained, subsequent reports (3, 4) indicated violet visible spectroscopy of bloody CSF that acute intracranial hemorrhage could be much more difficult to stored hypoxically for 3 days showed the detect on MR images. This was attributed by Sipponen et al. (3) to a presence of methemoglobin. The iron in lack of Ti shortening during the acute phase; however, they at- methemoglobin is paramagnetic; in com- tempted no explanation of this phenomenon. -

A Time-Updated, Parsimonious Model to Predict AKI in Hospitalized Children
CLINICAL RESEARCH www.jasn.org A Time-Updated, Parsimonious Model to Predict AKI in Hospitalized Children Ibrahim Sandokji ,1,2 Yu Yamamoto ,2 Aditya Biswas,2 Tanima Arora ,2 Ugochukwu Ugwuowo,2 Michael Simonov,2 Ishan Saran,2 Melissa Martin ,2 Jeffrey M. Testani,3 Sherry Mansour,2 Dennis G. Moledina ,2 Jason H. Greenberg ,1,2 and F. Perry Wilson 2 1Department of Pediatrics, Section of Nephrology, Yale University School of Medicine, New Haven, Connecticut 2Clinical and Translational Research Accelerator, Department of Medicine, Yale University School of Medicine, New Haven, Connecticut 3Section of Cardiovascular Medicine, Department of Internal Medicine, Yale University School of Medicine, New Haven, Connecticut ABSTRACT Background Timely prediction of AKI in children can allow for targeted interventions, but the wealth of data in the electronic health record poses unique modeling challenges. Methods We retrospectively reviewed the electronic medical records of all children younger than 18 years old who had at least two creatinine values measured during a hospital admission from January 2014 through January 2018. We divided the study population into derivation, and internal and external valida- tion cohorts, and used five feature selection techniques to select 10 of 720 potentially predictive variables from the electronic health records. Model performance was assessed by the area under the receiver operating characteristic curve in the validation cohorts. The primary outcome was development of AKI (per the Kidney Disease Improving Global Outcomes creatinine definition) within a moving 48-hour win- dow. Secondary outcomes included severe AKI (stage 2 or 3), inpatient mortality, and length of stay. Results Among 8473 encounters studied, AKI occurred in 516 (10.2%), 207 (9%), and 27 (2.5%) encounters in the derivation, and internal and external validation cohorts, respectively. -

Routine Cerebrospinal Fluid (CSF) Analysis
CHAPTER4 Routine cerebrospinal fluid (CSF) analysis a b a ) F. Deisenhammer, A. Bartos, R. Egg, Albumin CSF/serum ratio (Qalb should be pre- N. E. Gilhus,c G. Giovannoni,d S. Rauer,e ferred to total protein measurement and normal F. Sellebjergf upper limits should be related to patients’ age. Elevated Qalb is a non-specific finding but occurs mainly in bacterial, cryptococcal, and tubercu- Background A great variety of neurological diseases lous meningitis, leptomingeal metastases as well require investigation of the cerebrospinal fluid as acute and chronic demyelinating polyneu- (CSF) to prove the diagnosis or to rule out relevant ropathies. differential diagnoses. Pathological decrease of the CSF/serum glu- cose ratio or an increase in lactate concentration Objectives To evaluate the theoretical background indicates bacterial or fungal meningitis or lep- and provide guidelines for clinical use in rou- tomeningeal metastases. tine CSF analysis including total protein, albumin, Intrathecal immunoglobulin G synthesis is best immunoglobulins, glucose, lactate, cell count, demonstrated by isoelectric focusing followed by cytological staining, and investigation of infec- specific staining. tious CSF. Cellular morphology (cytological staining) should be evaluated whenever pleocytosis is found or Methods Systematic Medline search for the above leptomeningeal metastases or pathological bleed- mentioned variables. Review of appropriate publi- ing is suspected. Computed tomography-negative cations by one or more of the task force members. intrathecal bleeding should be investigated by Grading of evidence and recommendations was bilirubin detection. based on consensus by all task force members. Introduction CSF should be analysed immediately after collec- tion. If storage is needed 12 ml of CSF should The cerebrospinal fluid (CSF) is a dynamic, be partitioned into three to four sterile tubes. -

2017 LAB GUIDE TEST MENU March 2017Edition
2017 LAB GUIDE TEST MENU March 2017Edition Replaces: Sept 2015 Edition STAT TESTING MENU (2 Pages) 30 Minute In-Lab Turnaround Time (TAT) Unless Further Noted Below (In-Lab Time) MICROBIOLOGY 1. Spinal Fluid Culture set up and Gram Stain of sediment, India Ink prep 2. Gram Stain, other sites 3. Planting of cultures 4. Wet prep 5. Rapid Strep A Antigen Test (15 min. TAT) 6. Rapid Influenza A & B Antigen test 7. Rapid RSV Antigen test 8. Malaria Prep (60 min. TAT), Evening and Night shifts will only report “Parasites present or absent” 9. Screen, Gastric Urease, for Helicobacter Pylori (60 min. TAT) 10. Clostridium difficile DNA amplification (60 min. TAT) BLOOD BANK 1. Compatibility testing (leuko-reduced packed cells) 2. Type and Screen (60 min. TAT) 3. Cord Blood (2 hours) HEMATOLOGY 1. Complete Blood Count (CBC) SEE NOTE #1 2. Fibrinogen 3. Hemogram (ABC) 4. Monospot Test 5. Partial Thromboplastin Time (PTT) (60 min. TAT) 6. Prothrombin Time (PT) (60 min. TAT) 7. Fluid Cell Count (60 min. TAT) 8. Complete Urinalysis 9. D-dimer 10. Fluid pH CHEMISTRY 1. Arterial Blood Gases 2. Acetone 3. Ammonia 4. Amylase 5. Basic Metabolic Panel: Sodium, Potassium, Chloride, CO2, Creatinine, BUN, Glucose, and Calcium 6. Bilirubin (Total) 7. Blood Urea Nitrogen (BUN) 8. Calcium (Total and Ionized) 9. CPK (Total) (60 min. TAT for CPK total with MB fraction. CPKMB only run if CPK total > 113) UVM HEALTH NETWORK-CVPH 2 TEST MENU 10. Creatinine 11. CSF (Glucose and Protein) 12. Electrolytes: Sodium (Na), Potassium (K), Chloride (Cl), CO2 13. -

Effects of Hyperglycemia and Rapid Lowering of Plasma Glucose in Normal Rabbits
MILESTONES IN NEPHROLOGY J Am Soc Nephrol 11: 1776–1788, 2000 Mark A. Knepper, Feature Editor Studies on Mechanisms of Cerebral Edema in Diabetic Comas EFFECTS OF HYPERGLYCEMIA AND RAPID LOWERING OF PLASMA GLUCOSE IN NORMAL RABBITS ALLEN I. ARIEFF AND CHARLES R. KLEEMAN WITH THE TECHNICAL ASSISTANCE OF ALICE KEUSHKERIAN AND HELEN BAGDOYAN From the Departments of Medicine, Wadsworth Veterans Administration Center and Cedars-Sinai Medical Center, and the Cedars-Sinai Medical Research Institute, and University of California Los Angeles Medical Center, Los Angeles, California 90048 with comments by ALLEN I. ARIEFF AND RICHARD STERNS Reprinted from J. Clin. Invest. 52:571–583, 1973 A BSTRACT To investigate the pathophysiology of cerebral edema occurring during treatment of diabetic coma, the effects of hyperglycemia and rapid lowering of plasma glucose were AUTHOR COMMENTARY evaluated in normal rabbits. During 2 h of hyperglycemia (plasma glucose = 61 mM), both brain (cerebral cortex) and Allen I. Arieff muscle initially lost about 10% of water content. After 4 h of hyperglycemia, skeletal muscle water content remained low University of California, but that of brain was normal. Brain osmolality (Osm) (343 San Francisco mosmol/kg H2O) was similar to that of cerebrospinal fluid Sausalito, California (CSF) (340 mosmol/kg), but increases in the concentration of Na+, K+, Cl–, glucose, sorbitol, lactate, urea, myoinositol, and amino acids accounted for only about half of this increase. n 1936, Dillon, Riggs, and Dyer described a syndrome The unidentified solute was designated “idiogenic osmoles”. Iwhereby individuals who were being treated for diabetic When plasma glucose was rapidly lowered to normal with coma and apparently recovering suddenly deteriorated, with insulin, there was gross brain edema, increases in brain content worsening of coma, respiratory insufficiency, hypotension, of water, Na+, K+, Cl– and idiogenic osmoles, and a signifi tachycardia, high fever, and death (1). -

Tests…But Maybe You Transports Don’T 2
11/12/15 Some things you should When lab tests are useful know about laboratory 1. Managing patients during critical care tests…But maybe you transports don’t 2. While transporting patient to medical facilities for evaluation of laboratory Steve Faynor, CCEMT-P abnormalities HCA Chippenham Medical Center Richmond Ambulance Authority Objectives 1. Review some basic laboratory tests. Treat the patient, not the 2. Appreciate how patterns of laboratory test results can offer insight into etiology. laboratory values. 3. Learn how laboratory test calculations can add additional clinical information. 4. Review some limitations of laboratory tests. ELECTROLYTES & A case of “bad labs” RENAL FUNCTION TESTS 1 11/12/15 Hypernatremia & Renal Failure Hypernatremia • 89 year old white female • Hyperaldosteronism • Coming from nursing home due to • Cushing’s disease or syndrome abnormal labs • Diabetes insipidus (deficiency of ADH) • Sodium 172 mmol/L • Dehydration • Potassium 4.2 mmol/L • Chloride 137 mmol/L • Carbon dioxide 21 mmol/L • What are some causes of hypernatremia? • BP 122/66, SBP 99 later • BUN 212 mg N/dL • HR 64/min • Creatinine 6.10 mg/dL • RR 21/min • What do these values indicate? • SpCO2 98% on 4 L oxygen per min • Does this change your therapy? • Tongue dry, skin turgor poor • What is the cause of the hypernatremia in this patient? Treatment? Acute Renal Failure Use of the BUN/creatinine ratio • Intrinsic renal disease • In intrinsic causes of acute renal failure, the – Acute tubular necrosis: ischemia, toxins BUN/creatinine ratio is typically 10-15. – Acute glomerulonephritis • In pre-renal causes of acute renal failure, – CKD with missed dialysis the BUN/creatinine ratio is typically >20. -

Cerebrospinal Fluid and Hydrocephalus: Physiology, Diagnosis, and Treatment Andreas K
cancercontroljournal.org Vol. 24, No. 1, January 2017 H. LEE MOFFITT CANCER CENTER & RESEARCH INSTITUTE, AN NCI COMPREHENSIVE CANCER CENTER Cerebrospinal Fluid and Hydrocephalus: Physiology, Diagnosis, and Treatment Andreas K. Filis, MD, Kamran Aghayev, MD, and Frank D. Vrionis, MD, PhD Clinical Presentation, Diagnosis, and Radiological Findings of Neoplastic Meningitis Georgios Rigakos, MD, Chrysoula I. Liakou, MD, Naillid Felipe, et al Neoplastic Meningitis Due to Lung, Breast, and Melanoma Metastases Emilie Le Rhun, MD, Sophie Taillibert, MD, and Marc C. Chamberlain, MD Diagnosis and Management of Leukemic and Lymphomatous Meningitis Hemant Murthy, MD, Claudio Anasetti, MD, and Ernesto Ayala, MD Experimental Treatments for Leptomeningeal Metastases From Solid Malignancies Solmaz Sahebjam, MD, Peter A. Forsyth, MD, Keiran S. Smalley, PhD, et al Surgical Treatment for Leptomeningeal Disease Andrey A. Volkov, DO, Andreas K. Filis, MD, and Frank D. Vrionis, MD, PhD Cancer Control is included in Index Medicus/MEDLINE Editorial Board Members Editor: Conor C. Lynch, PhD Production Team: Assistant Member Lodovico Balducci, MD Veronica Nemeth Tumor Biology Senior Member Editorial Coordinator Program Leader, Senior Adult Oncology Program Kristen J. Otto, MD Sherri Damlo Moffitt Cancer Center Associate Member Managing Medical Editor Head and Neck and Endocrine Oncology Diane McEnaney Deputy Editor: Graphic Design Consultant Julio M. Pow-Sang, MD Michael A. Poch, MD Senior Member Assistant Member Associate Editor of Chair, Department of Genitourinary Oncology Genitourinary Oncology Educational Projects Director of Moffitt Robotics Program Jeffery S. Russell, MD, PhD John M. York, PharmD Moffitt Cancer Center Assistant Member Akita Biomedical Consulting Endocrine Tumor Oncology 1111 Bailey Drive Editor Emeritus: Elizabeth M.