Investigating Regions of Shared Genetic Variation in Attention Deficit/Hyperactivity Disorder and Major Depressive Disorder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Defining Functional Interactions During Biogenesis of Epithelial Junctions
ARTICLE Received 11 Dec 2015 | Accepted 13 Oct 2016 | Published 6 Dec 2016 | Updated 5 Jan 2017 DOI: 10.1038/ncomms13542 OPEN Defining functional interactions during biogenesis of epithelial junctions J.C. Erasmus1,*, S. Bruche1,*,w, L. Pizarro1,2,*, N. Maimari1,3,*, T. Poggioli1,w, C. Tomlinson4,J.Lees5, I. Zalivina1,w, A. Wheeler1,w, A. Alberts6, A. Russo2 & V.M.M. Braga1 In spite of extensive recent progress, a comprehensive understanding of how actin cytoskeleton remodelling supports stable junctions remains to be established. Here we design a platform that integrates actin functions with optimized phenotypic clustering and identify new cytoskeletal proteins, their functional hierarchy and pathways that modulate E-cadherin adhesion. Depletion of EEF1A, an actin bundling protein, increases E-cadherin levels at junctions without a corresponding reinforcement of cell–cell contacts. This unexpected result reflects a more dynamic and mobile junctional actin in EEF1A-depleted cells. A partner for EEF1A in cadherin contact maintenance is the formin DIAPH2, which interacts with EEF1A. In contrast, depletion of either the endocytic regulator TRIP10 or the Rho GTPase activator VAV2 reduces E-cadherin levels at junctions. TRIP10 binds to and requires VAV2 function for its junctional localization. Overall, we present new conceptual insights on junction stabilization, which integrate known and novel pathways with impact for epithelial morphogenesis, homeostasis and diseases. 1 National Heart and Lung Institute, Faculty of Medicine, Imperial College London, London SW7 2AZ, UK. 2 Computing Department, Imperial College London, London SW7 2AZ, UK. 3 Bioengineering Department, Faculty of Engineering, Imperial College London, London SW7 2AZ, UK. 4 Department of Surgery & Cancer, Faculty of Medicine, Imperial College London, London SW7 2AZ, UK. -

Aneuploidy: Using Genetic Instability to Preserve a Haploid Genome?
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Science (Cancer Biology) Aneuploidy: Using genetic instability to preserve a haploid genome? Submitted by: Ramona Ramdath In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Science Examination Committee Signature/Date Major Advisor: David Allison, M.D., Ph.D. Academic James Trempe, Ph.D. Advisory Committee: David Giovanucci, Ph.D. Randall Ruch, Ph.D. Ronald Mellgren, Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: April 10, 2009 Aneuploidy: Using genetic instability to preserve a haploid genome? Ramona Ramdath University of Toledo, Health Science Campus 2009 Dedication I dedicate this dissertation to my grandfather who died of lung cancer two years ago, but who always instilled in us the value and importance of education. And to my mom and sister, both of whom have been pillars of support and stimulating conversations. To my sister, Rehanna, especially- I hope this inspires you to achieve all that you want to in life, academically and otherwise. ii Acknowledgements As we go through these academic journeys, there are so many along the way that make an impact not only on our work, but on our lives as well, and I would like to say a heartfelt thank you to all of those people: My Committee members- Dr. James Trempe, Dr. David Giovanucchi, Dr. Ronald Mellgren and Dr. Randall Ruch for their guidance, suggestions, support and confidence in me. My major advisor- Dr. David Allison, for his constructive criticism and positive reinforcement. -

WO 2019/068007 Al Figure 2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2019/068007 Al 04 April 2019 (04.04.2019) W 1P O PCT (51) International Patent Classification: (72) Inventors; and C12N 15/10 (2006.01) C07K 16/28 (2006.01) (71) Applicants: GROSS, Gideon [EVIL]; IE-1-5 Address C12N 5/10 (2006.0 1) C12Q 1/6809 (20 18.0 1) M.P. Korazim, 1292200 Moshav Almagor (IL). GIBSON, C07K 14/705 (2006.01) A61P 35/00 (2006.01) Will [US/US]; c/o ImmPACT-Bio Ltd., 2 Ilian Ramon St., C07K 14/725 (2006.01) P.O. Box 4044, 7403635 Ness Ziona (TL). DAHARY, Dvir [EilL]; c/o ImmPACT-Bio Ltd., 2 Ilian Ramon St., P.O. (21) International Application Number: Box 4044, 7403635 Ness Ziona (IL). BEIMAN, Merav PCT/US2018/053583 [EilL]; c/o ImmPACT-Bio Ltd., 2 Ilian Ramon St., P.O. (22) International Filing Date: Box 4044, 7403635 Ness Ziona (E.). 28 September 2018 (28.09.2018) (74) Agent: MACDOUGALL, Christina, A. et al; Morgan, (25) Filing Language: English Lewis & Bockius LLP, One Market, Spear Tower, SanFran- cisco, CA 94105 (US). (26) Publication Language: English (81) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of national protection available): AE, AG, AL, AM, 62/564,454 28 September 2017 (28.09.2017) US AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, 62/649,429 28 March 2018 (28.03.2018) US CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, (71) Applicant: IMMP ACT-BIO LTD. -
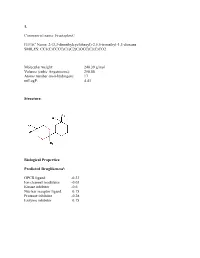
Sean Raspet – Molecules
1. Commercial name: Fructaplex© IUPAC Name: 2-(3,3-dimethylcyclohexyl)-2,5,5-trimethyl-1,3-dioxane SMILES: CC1(C)CCCC(C1)C2(C)OCC(C)(C)CO2 Molecular weight: 240.39 g/mol Volume (cubic Angstroems): 258.88 Atoms number (non-hydrogen): 17 miLogP: 4.43 Structure: Biological Properties: Predicted Druglikenessi: GPCR ligand -0.23 Ion channel modulator -0.03 Kinase inhibitor -0.6 Nuclear receptor ligand 0.15 Protease inhibitor -0.28 Enzyme inhibitor 0.15 Commercial name: Fructaplex© IUPAC Name: 2-(3,3-dimethylcyclohexyl)-2,5,5-trimethyl-1,3-dioxane SMILES: CC1(C)CCCC(C1)C2(C)OCC(C)(C)CO2 Predicted Olfactory Receptor Activityii: OR2L13 83.715% OR1G1 82.761% OR10J5 80.569% OR2W1 78.180% OR7A2 77.696% 2. Commercial name: Sylvoxime© IUPAC Name: N-[4-(1-ethoxyethenyl)-3,3,5,5tetramethylcyclohexylidene]hydroxylamine SMILES: CCOC(=C)C1C(C)(C)CC(CC1(C)C)=NO Molecular weight: 239.36 Volume (cubic Angstroems): 252.83 Atoms number (non-hydrogen): 17 miLogP: 4.33 Structure: Biological Properties: Predicted Druglikeness: GPCR ligand -0.6 Ion channel modulator -0.41 Kinase inhibitor -0.93 Nuclear receptor ligand -0.17 Protease inhibitor -0.39 Enzyme inhibitor 0.01 Commercial name: Sylvoxime© IUPAC Name: N-[4-(1-ethoxyethenyl)-3,3,5,5tetramethylcyclohexylidene]hydroxylamine SMILES: CCOC(=C)C1C(C)(C)CC(CC1(C)C)=NO Predicted Olfactory Receptor Activity: OR52D1 71.900% OR1G1 70.394% 0R52I2 70.392% OR52I1 70.390% OR2Y1 70.378% 3. Commercial name: Hyperflor© IUPAC Name: 2-benzyl-1,3-dioxan-5-one SMILES: O=C1COC(CC2=CC=CC=C2)OC1 Molecular weight: 192.21 g/mol Volume -

Ncomms-18-33880B
ORE Open Research Exeter TITLE Genome-wide association study identifies genetic loci for self-reported habitual sleep duration supported by accelerometer-derived estimates. AUTHORS Dashti, HS; Jones, SE; Wood, AR; et al. JOURNAL Nature Communications DEPOSITED IN ORE 15 March 2019 This version available at http://hdl.handle.net/10871/36477 COPYRIGHT AND REUSE Open Research Exeter makes this work available in accordance with publisher policies. A NOTE ON VERSIONS The version presented here may differ from the published version. If citing, you are advised to consult the published version for pagination, volume/issue and date of publication NCOMMS-18-33880B Dashti et al. a. Sleep Duration Heritability = 9.8 (0.1)% ) P ( 10 log - Chromosome 1 2 3 4 5 6 7 10 11 14 17 19 C1orf94 PAX8 PCCB BANK1 PAM SCAND3 FOXP2 LOC100131719 HSD17B12 LOC100128215 LOC644157 PIN1 GJB5 LOC100130100 PPP2R3A LCORL PPIP5K2 LOC646160 MAD1L1 GPR26 METT5D1 PRKD1 LOC644172 OLFM2 PDE4B VRK2 STAG1 LOC645174 GIN1 FAM83B CHCHD3 MLLT10 OR2BH1P NOVA1 PER1 DAB1 GALNT3 MSL2 PRKG2 C5ORF30 MEA1 DNAJC1 C11orf63 ADCK1 PFAS DPYD SCN1A BBX, CCSER1 SLC6A3 PPP2R5D 8 SKIDA1 DRD2 FRDAP SMAD5-AS5 20 TTC21B LOC285205 LOC100132531 SMAD5-AS2 PPP1R3B EGR2 PTPRJ RTN1 VAMP2 YWHAB PABPCP2 LOC100128160 LOC285577 SRF PABPC1L LOC100129150 ADO OR4X2 12 FNTB AURKB LOC100133235 FOXP1 FGFR4 CUL7 FGF8 OR4B1 GPX2 ARHGEF15 SLC8A1 IL20RB V27 SLC34A1 DNPH1 KSR2 9 NFKB2 OR4S1 MVK MAX RANGRF MBOAT2 NPM1P17 RGS14 CUL9 ZCCHC7 PITX3 OR4X1 CHURC1 BORCS6 MAP2 ERC2 LMAN2 MRPL2 KCTD10 MRPL41 PSD TRPC6 UBE3B RAB15 CTC1, -
Get High-Res Image
150 100 50 163 169 313 # mutations Non syn. Syn. E">)->(A/T: E">6A/C/T)->(A/T) flip A->6";): indel+null double_null # mutations/Mb 0 20 40 60 80 2% 6% 4% 5% 1% 3% 3% 5% 4% 1% 3% 2% 10% 8% 5% 2% 3% 5% 7% 2% 4% 1% 5% 2% 4% 4% 6% 4% 5% 2% 2% 5% 4% 3% 6% 3% 17% 2% 1% 1% 6% 3% 1% 4% 1% 2% 3% 8% 2% 2% 5% 3% 2% 1% 6% 5% 2% 2% 4% 3% 6% 3% 1% 3% 3% 5% 1% 4% 2% 0% 5% 3% 5% 4% 1% 3% 15% 4% 2% 10% 7% 7% 3% 10% 3% 6% 4% 3% 11% 4% 3% 6% 21% 3% 3% 4% 8% 2% 6% 5% 4% 8% 3% 3% 6% 1% 6% 3% 2% 5% 7% 5% 3% 3% 2% 10% 3% 17% 6% 6% 4% 6% 12% 9% 5% 6% 5% 4% 3% 2% 21% 5% 4% 4% 17% 5% 3% 4% 3% 4% 4% 7% 7% 6% 6% 6% 4% 6% 6% 6% 8% 6% 1% 2% 2% 2% 3% 4% 8% 13% 17% 30% 54% 15% 0 (0A$205243952TP (0A$297281792TP(0A$273246702TP (0A$299280252TP(0A$255282992TP (0A$2MP2A4T&2TP(0A$250259392TP (0A$205254252TP(0A$244267792TP (0A$255279132TP(0A$275251462TP (0A$2622A4712TP(0A$255275742TP (0A$205244322TP(0A$244281202TP (0A$2442A4792TP(0A$249244872TP (0A$2N-2A4'&2TP(0A$286282802TP (0A$278275352TP(0A$255215962TP (0A$235236152TP(0A$244261442TP (0A$2N-2A55!2TP(0A$278271662TP (0A$244267762TP(0A$244276712TP (0A$2-2281942TP(0A$267237742TP (0A$2N-2A4'P2TP(0A$255282032TP (0A$205244172TP(0A$255285082TP (0A$286283592TP(0A$286277132TP (0A$2MP2A4TE2TP(0A$280256082TP (0A$299280322TP(0A$255286152TP (0A$2622A46S2TP(0A$250259322TP (0A$2N-2A55*2TP(0A$278271612TP (0A$2952A4VP2TP(0A$249245072TP (0A$249244862TP(0A$291268492TP (0A$2622A46P2TP(0A$2622A4702TP (0A$205244222TP(0A$250250722TP (0A$2MP2A4TH2TP(0A$275270312TP (0A$299280332TP(0A$255280942TP (0A$295270392TP(0A$255283022TP (0A$249245052TP(0A$293280672TP -

Clinical, Molecular, and Immune Analysis of Dabrafenib-Trametinib
Supplementary Online Content Chen G, McQuade JL, Panka DJ, et al. Clinical, molecular and immune analysis of dabrafenib-trametinib combination treatment for metastatic melanoma that progressed during BRAF inhibitor monotherapy: a phase 2 clinical trial. JAMA Oncology. Published online April 28, 2016. doi:10.1001/jamaoncol.2016.0509. eMethods. eReferences. eTable 1. Clinical efficacy eTable 2. Adverse events eTable 3. Correlation of baseline patient characteristics with treatment outcomes eTable 4. Patient responses and baseline IHC results eFigure 1. Kaplan-Meier analysis of overall survival eFigure 2. Correlation between IHC and RNAseq results eFigure 3. pPRAS40 expression and PFS eFigure 4. Baseline and treatment-induced changes in immune infiltrates eFigure 5. PD-L1 expression eTable 5. Nonsynonymous mutations detected by WES in baseline tumors This supplementary material has been provided by the authors to give readers additional information about their work. © 2016 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/30/2021 eMethods Whole exome sequencing Whole exome capture libraries for both tumor and normal samples were constructed using 100ng genomic DNA input and following the protocol as described by Fisher et al.,3 with the following adapter modification: Illumina paired end adapters were replaced with palindromic forked adapters with unique 8 base index sequences embedded within the adapter. In-solution hybrid selection was performed using the Illumina Rapid Capture Exome enrichment kit with 38Mb target territory (29Mb baited). The targeted region includes 98.3% of the intervals in the Refseq exome database. Dual-indexed libraries were pooled into groups of up to 96 samples prior to hybridization. -

Unifying the Genomics-Based Classes of Cancer Fusion Gene Partners: Large Cancer Fusion Genes Are Evolutionarily Conserved
CANCER GENOMICS & PROTEOMICS 9: 389-396 (2012) Unifying the Genomics-based Classes of Cancer Fusion Gene Partners: Large Cancer Fusion Genes Are Evolutionarily Conserved LIBIA M. PAVA, DANIEL T. MORTON, REN CHEN and GEORGE BLANCK Department of Molecular Medicine, Morsani College of Medicine, University of South Florida, Tampa, FL, U.S.A. Abstract. Background: Genes that fuse to cause cancer have fusion of NPM and ALK in anaplastic large-cell lymphoma been studied to determine molecular bases for proliferation, to (3); ABL and BCR in chronic myelogenous leukemia (CML) develop diagnostic tools, and as targets for drugs. To facilitate (4, 5); and C-MYC and IgH in Burkitt’s lymphoma in (6), identification of additional, cancer fusion genes, following among many others. The detection and understanding of the observation of a chromosomal translocation, we have ABL-BCR fusion protein, which stimulates unregulated cell characterized the genomic features of the fusion gene partners. division and leads to leukemia, led to the development of Previous work indicated that cancer fusion gene partners, are Gleevec, a drug able to block the ATP-binding site of the either large or evolutionarily conserved in comparison to the tyrosine kinase domain of ABL-BCR, halting CML (7). This neighboring genes in the region of a chromosomal extraordinary success has led to the hope of designing drugs translocation. These results raised the question of whether targeted against other cancer fusion proteins. large cancer fusion gene partners were also evolutionarily There are about 50,000 unstudied translocations, raising conserved. Methods and Results: We developed two methods the question of whether that information can continue to be for quantifying evolutionary conservation values, allowing the used to facilitate the identification of fusion genes. -

A Multi-Cancer Gene Signature Associated with Stromal Activation
A multi-cancer gene signature associated with stromal activation Sandra Orsulic, PhD Professor of OB/GYN Women’s Cancer Program Samuel Oschin Comprehensive Cancer Institute I Cedars-Sinai Medical Center 1100011010 1001000101 0101001011 Stroma/ECM Prevents Tumor Invasion Stroma/ECM Promotes Tumor Invasion Tumor Growth and Stroma Remodeling Ki67-positive dividing cells cancer cells stroma Tumor Growth and Stroma Remodeling Ki67-positive dividing cells cancer • proliferative cells • targeted by chemotherapy • genetically unstable stroma Tumor Growth and Stroma Remodeling Ki67-positive dividing cells cancer • proliferating cells • targeted by chemotherapy • genetically unstable • slow proliferating • not targeted by chemotherapy stroma • genetically stable • enhanced remodeling predicts poor outcome Expression of COL11A1 in Intratumoral Stroma COL11A1 + Fat 0% Peritumoral ~1% stroma Tumor ~50% Intratumoral 100µm stroma COL11A1 Expression in Cancers and Corresponding Normal Tissues Smooth Muscle Actin Expression in Cancers and Corresponding Normal Tissues COL11A1 Expression in Cancers and Corresponding Normal Tissues BREAST COLORECTAL 1 2 1 2 3 1. Breast (61) 1. Colon (19) 2. Invasive ductal breast 2. Rectum (3) carcinoma (389) 3. Colon adenocarcinoma (101) Overexpression gene rank: 1 Overexpression gene rank: 3 (in top 1%) (in top 1%) p-value: 1.15E-73 p-value: 2.19E-44 t-test: 33.769 t-test: 27.871 fold change: 40.542 fold change: 32.796 Increase in COL11A1 Levels During Cancer Progression Breast Cancer Ductal Invasive Carcinoma Ductal In -

(12) Patent Application Publication (10) Pub. No.: US 2016/0264934 A1 GALLOURAKIS Et Al
US 20160264934A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2016/0264934 A1 GALLOURAKIS et al. (43) Pub. Date: Sep. 15, 2016 (54) METHODS FOR MODULATING AND Publication Classification ASSAYING MI6AIN STEM CELL POPULATIONS (51) Int. Cl. CI2N5/0735 (2006.01) (71) Applicants: THE GENERAL, HOSPITAL AOIN I/02 (2006.01) CORPORATION, Boston, MA (US); CI2O I/68 (2006.01) The Regents of the University of GOIN 33/573 (2006.01) California, Oakland, CA (US) CI2N 5/077 (2006.01) CI2N5/0793 (2006.01) (72) Inventors: Cosmas GIALLOURAKIS, Boston, (52) U.S. Cl. MA (US); Alan C. MULLEN, CPC ............ CI2N5/0606 (2013.01); CI2N5/0657 Brookline, MA (US); Yi XING, (2013.01); C12N5/0619 (2013.01); C12O Torrance, CA (US) I/6888 (2013.01); G0IN33/573 (2013.01); A0IN I/0226 (2013.01); C12N 2501/72 (73) Assignees: THE GENERAL, HOSPITAL (2013.01); C12N 2506/02 (2013.01); C12O CORPORATION, Boston, MA (US); 2600/158 (2013.01); C12Y 201/01062 The Regents of the University of (2013.01); C12Y 201/01 (2013.01) California, Oakland, CA (US) (57) ABSTRACT (21) Appl. No.: 15/067,780 The present invention generally relates to methods, assays and kits to maintain a human stem cell population in an (22) Filed: Mar 11, 2016 undifferentiated state by inhibiting the expression or function of METTL3 and/or METTL4, and mA fingerprint methods, assays, arrays and kits to assess the cell state of a human stem Related U.S. Application Data cell population by assessing mA levels (e.g. mA peak inten (60) Provisional application No. -

Prediction of Age at Onset in Parkinson's Disease Using Objective
www.nature.com/scientificreports OPEN Prediction of age at onset in Parkinson’s disease using objective specifc neuroimaging genetics based on a sparse canonical correlation analysis Ji Hye Won1,2, Mansu Kim1,2, Jinyoung Youn3,4* & Hyunjin Park2,5* The age at onset (AAO) is an important determinant in Parkinson’s disease (PD). Neuroimaging genetics is suitable for studying AAO in PD as it jointly analyzes imaging and genetics. We aimed to identify features associated with AAO in PD by applying the objective-specifc neuroimaging genetics approach and constructing an AAO prediction model. Our objective-specifc neuroimaging genetics extended the sparse canonical correlation analysis by an additional data type related to the target task to investigate possible associations of the imaging–genetic, genetic–target, and imaging– target pairs simultaneously. The identifed imaging, genetic, and combined features were used to construct analytical models to predict the AAO in a nested fve-fold cross-validation. We compared our approach with those from two feature selection approaches where only associations of imaging– target and genetic–target were explored. Using only imaging features, AAO prediction was accurate in all methods. Using only genetic features, the results from other methods were worse or unstable compared to our model. Using both imaging and genetic features, our proposed model predicted the AAO well (r = 0.5486). Our fndings could have signifcant impacts on the characterization of prodromal PD and contribute to diagnosing PD early because genetic features could be measured accurately from birth. Parkinson’s disease (PD) is the second most common neurodegenerative disorder and presents with various motor and non-motor symptoms1. -

The Hypothalamus As a Hub for SARS-Cov-2 Brain Infection and Pathogenesis
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.08.139329; this version posted June 19, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. The hypothalamus as a hub for SARS-CoV-2 brain infection and pathogenesis Sreekala Nampoothiri1,2#, Florent Sauve1,2#, Gaëtan Ternier1,2ƒ, Daniela Fernandois1,2 ƒ, Caio Coelho1,2, Monica ImBernon1,2, Eleonora Deligia1,2, Romain PerBet1, Vincent Florent1,2,3, Marc Baroncini1,2, Florence Pasquier1,4, François Trottein5, Claude-Alain Maurage1,2, Virginie Mattot1,2‡, Paolo GiacoBini1,2‡, S. Rasika1,2‡*, Vincent Prevot1,2‡* 1 Univ. Lille, Inserm, CHU Lille, Lille Neuroscience & Cognition, DistAlz, UMR-S 1172, Lille, France 2 LaBoratorY of Development and PlasticitY of the Neuroendocrine Brain, FHU 1000 daYs for health, EGID, School of Medicine, Lille, France 3 Nutrition, Arras General Hospital, Arras, France 4 Centre mémoire ressources et recherche, CHU Lille, LiCEND, Lille, France 5 Univ. Lille, CNRS, INSERM, CHU Lille, Institut Pasteur de Lille, U1019 - UMR 8204 - CIIL - Center for Infection and ImmunitY of Lille (CIIL), Lille, France. # and ƒ These authors contriButed equallY to this work. ‡ These authors directed this work *Correspondence to: [email protected] and [email protected] Short title: Covid-19: the hypothalamic hypothesis 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.06.08.139329; this version posted June 19, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity.