ISBN 90-77595-05-8 No Part of This Thesis May Be Reproduced Or
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Monograph on Dematiaceous Fungi
Monograph On Dematiaceous fungi A guide for description of dematiaceous fungi fungi of medical importance, diseases caused by them, diagnosis and treatment By Mohamed Refai and Heidy Abo El-Yazid Department of Microbiology, Faculty of Veterinary Medicine, Cairo University 2014 1 Preface The first time I saw cultures of dematiaceous fungi was in the laboratory of Prof. Seeliger in Bonn, 1962, when I attended a practical course on moulds for one week. Then I handled myself several cultures of black fungi, as contaminants in Mycology Laboratory of Prof. Rieth, 1963-1964, in Hamburg. When I visited Prof. DE Varies in Baarn, 1963. I was fascinated by the tremendous number of moulds in the Centraalbureau voor Schimmelcultures, Baarn, Netherlands. On the other hand, I was proud, that El-Sheikh Mahgoub, a Colleague from Sundan, wrote an internationally well-known book on mycetoma. I have never seen cases of dematiaceous fungal infections in Egypt, therefore, I was very happy, when I saw the collection of mycetoma cases reported in Egypt by the eminent Egyptian Mycologist, Prof. Dr Mohamed Taha, Zagazig University. To all these prominent mycologists I dedicate this monograph. Prof. Dr. Mohamed Refai, 1.5.2014 Heinz Seeliger Heinz Rieth Gerard de Vries, El-Sheikh Mahgoub Mohamed Taha 2 Contents 1. Introduction 4 2. 30. The genus Rhinocladiella 83 2. Description of dematiaceous 6 2. 31. The genus Scedosporium 86 fungi 2. 1. The genus Alternaria 6 2. 32. The genus Scytalidium 89 2.2. The genus Aurobasidium 11 2.33. The genus Stachybotrys 91 2.3. The genus Bipolaris 16 2. -
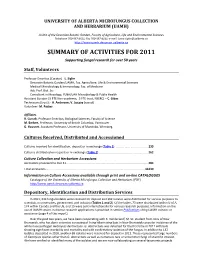
University of Alberta Microfungus Collection and Herbarium (Uamh)
UNIVERSITY OF ALBERTA MICROFUNGUS COLLECTION AND HERBARIUM (UAMH) A Unit of the Devonian Botanic Garden, Faculty of Agriculture, Life and Environmental Sciences Telephone 780‐987‐4811; Fax 780‐987‐4141; e‐mail: [email protected] http://www.uamh.devonian.ualberta.ca SUMMARY OF ACTIVITIES FOR 2011 Supporting fungal research for over 50 years Staff, Volunteers Professor Emeritus (Curator) ‐ L. Sigler Devonian Botanic Garden/UAMH, Fac. Agriculture, Life & Environmental Sciences Medical Microbiology & Immunology, Fac. of Medicine Adj. Prof. Biol. Sci. Consultant in Mycology, PLNA/UAH Microbiology & Public Health Assistant Curator (.5 FTE Non‐academic, .5 FTE trust, NSERC) – C. Gibas Technicians (trust): ‐ A. Anderson; V. Jajczay (casual) Volunteer‐ M. Packer Affiliates R. Currah, Professor Emeritus, Biological Sciences, Faculty of Science M. Berbee, Professor, University of British Columbia, Vancouver G. Hausner, Assistant Professor, University of Manitoba, Winnipeg Cultures Received, Distributed and Accessioned Cultures received for identification, deposit or in exchange (Table 1) ....................................... 233 Cultures distributed on request or in exchange (Table 2)............................................................ 262 Culture Collection and Herbarium Accessions Accessions processed to Dec 31. .................................................................................................. 284 Total accessions....................................................................................................................... -

The Mycobiome of Symptomatic Wood of Prunus Trees in Germany
The mycobiome of symptomatic wood of Prunus trees in Germany Dissertation zur Erlangung des Doktorgrades der Naturwissenschaften (Dr. rer. nat.) Naturwissenschaftliche Fakultät I – Biowissenschaften – der Martin-Luther-Universität Halle-Wittenberg vorgelegt von Herrn Steffen Bien Geb. am 29.07.1985 in Berlin Copyright notice Chapters 2 to 4 have been published in international journals. Only the publishers and the authors have the right for publishing and using the presented data. Any re-use of the presented data requires permissions from the publishers and the authors. Content III Content Summary .................................................................................................................. IV Zusammenfassung .................................................................................................. VI Abbreviations ......................................................................................................... VIII 1 General introduction ............................................................................................. 1 1.1 Importance of fungal diseases of wood and the knowledge about the associated fungal diversity ...................................................................................... 1 1.2 Host-fungus interactions in wood and wood diseases ....................................... 2 1.3 The genus Prunus ............................................................................................. 4 1.4 Diseases and fungal communities of Prunus wood .......................................... -

Chaetomium Atrobrunneum Causing Human Eumycetoma: the First Report
SYMPOSIUM Chaetomium atrobrunneum causing human eumycetoma: The first report Najwa A. Mhmoud1,2, Antonella Santona3, Maura Fiamma3, Emmanuel Edwar Siddig1, 3 1,4 3 Massimo Deligios , Sahar Mubarak BakhietID , Salvatore Rubino , Ahmed 1 Hassan FahalID * 1 Mycetoma Research Centre, University of Khartoum, Khartoum, Sudan, 2 Faculty of Medical Laboratory Sciences, University of Khartoum, Khartoum, Sudan, 3 Department of Biomedical Sciences, University of Sassari, Sassari, Italy, 4 Institute for Endemic Diseases, University of Khartoum, Khartoum, Sudan * [email protected], [email protected] Author summary In this communication, a case of black grain eumycetoma produced by the fungus C. atro- a1111111111 brunneum is reported. The patient was initially misdiagnosed with M. mycetomatis eumy- a1111111111 cetoma based on the grains' morphological and cytological features. However, further a1111111111 aerobic culture of the black grains generated a melanised fungus identified as C. atrobrun- a1111111111 neum by conventional morphological methods and by internal transcribed spacer 2 a1111111111 (ITS2) ribosomal RNA gene sequencing. This is the first-ever report of C. atrobrunneum as a eumycetoma-causative organism of black grain eumycetoma. It is essential that the causative organism is identified to the species level, as this is important for proper patient management and to predict treatment outcome and prognosis. OPEN ACCESS Citation: Mhmoud NA, Santona A, Fiamma M, Siddig EE, Deligios M, Bakhiet SM, et al. (2019) Chaetomium atrobrunneum causing human Overview eumycetoma: The first report. PLoS Negl Trop Dis Mycetoma is a chronic, progressive, granulomatous, subcutaneous inflammatory disease. It is 13(5): e0007276. https://doi.org/10.1371/journal. pntd.0007276 caused by certain fungi and bacteria, and thus, it is classified as a eumycetoma and an actino- mycetoma, respectively. -

SCEDOSPORIUM, ACREMONIUM, PHIALEMONIUM, LECYTHOPHORA Y PAECILOMYCES Haybrig Mercedes Perdomo Ziems
CARACTERIZACIÓN FENOTÍPICA Y MOLECULAR DE HONGOS FILAMENTOSOS OPORTUNISTAS: SCEDOSPORIUM, ACREMONIUM, PHIALEMONIUM, LECYTHOPHORA Y PAECILOMYCES Haybrig Mercedes Perdomo Ziems Dipòsit Legal: T. 1717-2011 ADVERTIMENT. La consulta d’aquesta tesi queda condicionada a l’acceptació de les següents condicions d'ús: La difusió d’aquesta tesi per mitjà del servei TDX (www.tesisenxarxa.net) ha estat autoritzada pels titulars dels drets de propietat intel·lectual únicament per a usos privats emmarcats en activitats d’investigació i docència. No s’autoritza la seva reproducció amb finalitats de lucre ni la seva difusió i posada a disposició des d’un lloc aliè al servei TDX. No s’autoritza la presentació del seu contingut en una finestra o marc aliè a TDX (framing). Aquesta reserva de drets afecta tant al resum de presentació de la tesi com als seus continguts. En la utilització o cita de parts de la tesi és obligat indicar el nom de la persona autora. ADVERTENCIA. La consulta de esta tesis queda condicionada a la aceptación de las siguientes condiciones de uso: La difusión de esta tesis por medio del servicio TDR (www.tesisenred.net) ha sido autorizada por los titulares de los derechos de propiedad intelectual únicamente para usos privados enmarcados en actividades de investigación y docencia. No se autoriza su reproducción con finalidades de lucro ni su difusión y puesta a disposición desde un sitio ajeno al servicio TDR. No se autoriza la presentación de su contenido en una ventana o marco ajeno a TDR (framing). Esta reserva de derechos afecta tanto al resumen de presentación de la tesis como a sus contenidos. -

Opportunistic Water-Borne Human Pathogenic Filamentous Fungi Unreported from Food
microorganisms Review Opportunistic Water-Borne Human Pathogenic Filamentous Fungi Unreported from Food Monika Novak Babiˇc 1,* ID , Jerneja Zupanˇciˇc 1, João Brandão 2 ID and Nina Gunde-Cimerman 1 1 Biotechnical Faculty, University of Ljubljana, Jamnikarjeva 101, SI-1000 Ljubljana, Slovenia; [email protected] (J.Z.); [email protected] (N.G.-C.) 2 Department of Environmental Health, National Institute of Health Doutor Ricardo Jorge, Av. Padre Cruz, 1649-016 Lisboa, Portugal; [email protected] * Correspondence: [email protected]; Tel.: +386-1-320-3405 Received: 14 June 2018; Accepted: 2 August 2018; Published: 3 August 2018 Abstract: Clean drinking water and sanitation are fundamental human rights recognized by the United Nations (UN) General Assembly and the Human Rights Council in 2010 (Resolution 64/292). In modern societies, water is not related only to drinking, it is also widely used for personal and home hygiene, and leisure. Ongoing human population and subsequent environmental stressors challenge the current standards on safe drinking and recreational water, requiring regular updating. Also, a changing Earth and its increasingly frequent extreme weather events and climatic changes underpin the necessity to adjust regulation to a risk-based approach. Although fungi were never introduced to water quality regulations, the incidence of fungal infections worldwide is growing, and changes in antimicrobial resistance patterns are taking place. The presence of fungi in different types of water has been thoroughly investigated during the past 30 years only in Europe, and more than 400 different species were reported from ground-, surface-, and tap-water. -
Phaeohyphomycoses, Emerging Opportunistic Diseases in Animals
UvA-DARE (Digital Academic Repository) Phaeohyphomycoses, Emerging Opportunistic Diseases in Animals Seyedmousavi, S.; Guillot, J.; de Hoog, G.S. DOI 10.1128/CMR.00065-12 Publication date 2013 Document Version Final published version Published in Clinical microbiology reviews Link to publication Citation for published version (APA): Seyedmousavi, S., Guillot, J., & de Hoog, G. S. (2013). Phaeohyphomycoses, Emerging Opportunistic Diseases in Animals. Clinical microbiology reviews, 26(1), 19-35. https://doi.org/10.1128/CMR.00065-12 General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:02 Oct 2021 Phaeohyphomycoses, Emerging Opportunistic Diseases in Animals S. Seyedmousavi,a,b J. -

57 Phialemonium
57 Phialemonium Dongyou Liu and R.R.M. Paterson contents 57.1 Introduction ..................................................................................................................................................................... 473 57.1.1 Classification, Morphology, and Biology ............................................................................................................ 473 57.1.2 Clinical Features and Pathogenesis ..................................................................................................................... 473 57.1.3 Diagnosis ............................................................................................................................................................. 474 57.2 Methods ........................................................................................................................................................................... 475 57.2.1 Sample Preparation .............................................................................................................................................. 475 57.2.2 Detection Procedures ........................................................................................................................................... 475 57.3 Conclusion ....................................................................................................................................................................... 476 References ................................................................................................................................................................................ -

Acremonium Phylogenetic Overview and Revision of Gliomastix, Sarocladium, and Trichothecium
available online at www.studiesinmycology.org StudieS in Mycology 68: 139–162. 2011. doi:10.3114/sim.2011.68.06 Acremonium phylogenetic overview and revision of Gliomastix, Sarocladium, and Trichothecium R.C. Summerbell1, 2*, C. Gueidan3, 4, H-J. Schroers3, 5, G.S. de Hoog3, M. Starink3, Y. Arocha Rosete1, J. Guarro6 and J.A. Scott1, 2 1Sporometrics, Inc. 219 Dufferin Street, Suite 20C, Toronto, Ont., Canada M6K 1Y9; 2Dalla Lana School of Public Health, University of Toronto, 223 College St., Toronto ON Canada M5T 1R4; 3CBS-KNAW, Fungal Biodiversity Centre, Uppsalalaan 8, 3584 CT Utrecht, The Netherlands; 4Department of Botany, The Natural History Museum, Cromwell Road, SW7 5BD London, United Kingdom; 5Agricultural Institute of Slovenia, Hacquetova 17, 1000 Ljubljana, Slovenia, Mycology Unit, Medical School; 6IISPV, Universitat Rovira i Virgili, Reus, Spain *Correspondence: Richard Summerbell, [email protected] Abstract: Over 200 new sequences are generated for members of the genus Acremonium and related taxa including ribosomal small subunit sequences (SSU) for phylogenetic analysis and large subunit (LSU) sequences for phylogeny and DNA-based identification. Phylogenetic analysis reveals that within the Hypocreales, there are two major clusters containing multiple Acremonium species. One clade contains Acremonium sclerotigenum, the genus Emericellopsis, and the genus Geosmithia as prominent elements. The second clade contains the genera Gliomastix sensu stricto and Bionectria. In addition, there are numerous smaller clades plus two multi-species clades, one containing Acremonium strictum and the type species of the genus Sarocladium, and, as seen in the combined SSU/LSU analysis, one associated subclade containing Acremonium breve and related species plus Acremonium curvulum and related species. -

Therapy of Non-Dermatophytic Mycoses in Animals
Journal of Fungi Review Therapy of Non-Dermatophytic Mycoses in Animals Daniel Elad Department of Clinical Bacteriology and Mycology, The Kimron Veterinary Institute, P.O. Box 12, Bet Dagan 50250, Israel; [email protected]; Tel.: +972-3-968168; Fax: +972-3-9681733 Received: 2 September 2018; Accepted: 29 October 2018; Published: 30 October 2018 Abstract: This review focuses on aspects of antimycotic therapy specific to veterinary medicine. In the first part, drug availability, limited mostly by economic consideration but also by clinical applicability and specific adverse effects, is described for polyenes, 5 fluorocytosine, azoles, echinocandins and terbinafine. In the second part, current knowledge and experience in the treatment of selected fungal infections are overviewed. These mycoses include disseminated mold infections in small animals (dogs and cats) and avian species, upper respiratory tract infections of small animals (sino-nasal and sino-orbital aspergillosis) and horses (guttural pouch mycosis), eumycetoma, infections caused by dimorphic fungi, (blastomycosis, histoplasmosis, coccidioidomycosis, paracoccidioidomycosis and sporothrichosis) and by yeasts and yeast-like microorganism (Cryptococcus spp. and Malassezia pachydermatis). Keywords: animal; mycosis; therapy; disseminated; upper respiratory tract; dimorphic; eumycetoma; cryptococcosis; Malassezia 1. Introduction Veterinary medical mycology often differs from the human counterpart by, among others, the clinical aspects (beyond the scope of this review), the variety of fungi involved and the antimycotic drugs available for use. Immunosuppression, induced by other infective agents or by medications, has led to a significant leap in the number of people affected and the species of fungi involved in human infections since the 1980s [1]. In veterinary mycology, this phenomenon was not observed. -

Uva-DARE (Digital Academic Repository)
UvA-DARE (Digital Academic Repository) Acremonium phylogenetic overview and revision of Gliomastix, Sarocladium, and Trichothecium. Summerbell, R.C.; Gueidan, C.; Schroers, H.J.; de Hoog, G.S.; Starink, M.; Arocha Rosete, Y.; Guarro, J.; Scott, J.A. DOI 10.3114/sim.2011.68.06 Publication date 2011 Document Version Final published version Published in Studies in Mycology Link to publication Citation for published version (APA): Summerbell, R. C., Gueidan, C., Schroers, H. J., de Hoog, G. S., Starink, M., Arocha Rosete, Y., Guarro, J., & Scott, J. A. (2011). Acremonium phylogenetic overview and revision of Gliomastix, Sarocladium, and Trichothecium. Studies in Mycology, 68(1), 139-162. https://doi.org/10.3114/sim.2011.68.06 General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:25 Sep 2021 available online at www.studiesinmycology.org StudieS in Mycology 68: 139–162. -

The Magnitude and Diversity of Infectious Diseases
Chapter 1 The Magnitude and Diversity of Infectious Diseases “All interest in disease and death is only another expression of interest in life.” Thomas Mann THE IMPORTANCE OF INFECTIOUS DISEASES IN TERMS OF HUMAN MORTALITY According to the U.S. Census Bureau, on July 20, 2011, the USA population was 311 806 379, and the world population was 6 950 195 831 [2]. The U.S. Central Intelligence agency estimates that the USA crude death rate is 8.36 per 1000 and the world crude death rate is 8.12 per 1000 [3]. This translates to 2.6 million people dying in 2011 in the USA, and 56.4 million people dying worldwide. These numbers, calculated from authoritative sources, correlate surprisingly well with the widely used rule of thumb that 1% of the human population dies each year. How many of the world’s 56.4 million deaths can be attributed to infectious diseases? According to World Health Organization, in 1996, when the global death toll was 52 million, “Infectious diseases remain the world’s leading cause of death, accounting for at least 17 million (about 33%) of the 52 million people who die each year” [4]. Of course, only a small fraction of infections result in death, and it is impossible to determine the total incidence of infec- tious diseases that occur each year, for all organisms combined. Still, it is useful to consider some of the damage inflicted by just a few of the organisms that infect humans. Malaria infects 500 million people. About 2 million people die each year from malaria [4].