Do Nurses Have the Switch Factor?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
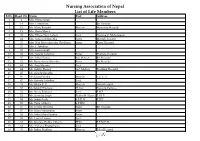
Nursing Association of Nepal List of Life Members S.No
Nursing Association of Nepal List of Life Members S.No. Regd. No. Name Post Address 1 2 Mrs. Prema Singh 2 14 Mrs. I. Mathema Bir Hospital 3 15 Ms. Manu Bangdel Matron Maternity Hospital 4 19 Mrs. Geeta Murch 5 20 Mrs. Dhana Nani Lohani Lect. Nursing C. Maharajgunj 6 24 Mrs. Saraswati Shrestha Sister Mental Hospital 7 25 Mrs. Nati Maya Shrestha (Pradhan) Sister Kanti Hospital 8 26 Mrs. I. Tuladhar 9 32 Mrs. Laxmi Singh 10 33 Mrs. Sarada Tuladhar Sister Pokhara Hospital 11 37 Mrs. Mita Thakur Ad. Matron Bir Hospital 12 42 Ms. Rameshwori Shrestha Sister Bir Hospital 13 43 Ms. Anju Sharma Lect. 14 44 Ms. Sabitry Basnet Ast. Matron Teaching Hospital 15 45 Ms. Sarada Shrestha 16 46 Ms. Geeta Pandey Matron T.U.T. H 17 47 Ms. Kamala Tuladhar Lect. 18 49 Ms. Bijaya K. C. Matron Teku Hospital 19 50 Ms.Sabitry Bhattarai D. Inst Nursing Campus 20 52 Ms. Neeta Pokharel Lect. F.H.P. 21 53 Ms. Sarmista Singh Publin H. Nurse F. H. P. 22 54 Ms. Sabitri Joshi S.P.H.N F.H.P. 23 55 Ms. Tuka Chhetry S.P.HN 24 56 Ms. Urmila Shrestha Sister Bir Hospital 25 57 Ms. Maya Manandhar Sister 26 58 Ms. Indra Maya Pandey Sister 27 62 Ms. Laxmi Thakur Lect. 28 63 Ms. Krishna Prabha Chhetri PHN F.P.M.C.H. 29 64 Ms. Archana Bhattacharya Lect. 30 65 Ms. Indira Pradhan Matron Teku Hospital S.No. Regd. No. Name Post Address 31 67 Ms. -

Lawrlwytho'r Atodiad Gwreiddiol
Operational services structure April 2021 14/04/2021 Operational Leadership Structures Director of Operations Director of Nursing & Quality Medical Director Lee McMenamy Joanne Hiley Dr Tessa Myatt Medical Operations Operations Clinical Director of Operations Deputy Director of Nursing & Deputy Medical Director Hazel Hendriksen Governance Dr Jose Mathew Assistant Clinical Director Assistant Director of Assistant Clinical DWiraerctringor ton & Halton Operations Corporate Corporate Lorna Pink Assistant Assistant Director Julie Chadwick Vacant Clinical Director of Nursing, AHP & Associate Clinical Director Governance & Professional Warrington & Halton Compliance Standards Assistant Director of Operations Assistant Clinical Director Dr Aravind Komuravelli Halton & Warrington Knowsley Lee Bloomfield Claire Hammill Clare Dooley Berni Fay-Dunkley Assistant Director of Operations Knowsley Associate Medical Director Nicky Over Assistant Clinical Director Allied Health Knowsley Assistant Director of Sefton Professional Dr Ashish Kumar AssiOstapenrta Dtiironesc tKnor oofw Oslpeeyr ations Sara Harrison Lead Nicola Over Sefton James Hester Anne Tattersall Assistant Clinical Director Associate Clinical Director Assistant Director of St Helens & Knowsley Inpatients St Helens Operations Sefton Debbie Tubey Dr Raj Madgula AssistanAt nDniree Tcatttore ofrs aOllp erations Head of St Helens & Knowsley Inpatients Safeguarding Tim McPhee Assistant Clinical Director Sarah Shaw Assistant Director of Associate Medical Director Operations St Helens Mental Health -

THE DEVELOPMENT of NURSING EDUCATION in the ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I
THE DEVELOPMENT OF NURSING EDUCATION IN THE ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I. GARDNER, B.S.N., M.S.N., M.Ed. A DISSERTATION IN HIGHER EDUCATION Submitted to the Graduate Faculty of Texas Tech University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF EDUCATION Approved Accepted Dean of the Graduate School August, 1993 ft 6 l^yrr^7^7 801 J ,... /;. -^o ACKNOWLEDGEMENTS C?^ /c-j/^/ C^ ;^o.^^ I would like to thank Dr. Clyde Kelsey, Jr., for his C'lp '^ ^unflagging support, his advice and his constant vigil and encouragement in the writing of this dissertation. I would also like to thank Dr. Patricia Yoder-Wise who acted as co-chairperson of my committee. Her advice was invaluable. Drs. Mezack, Willingham, and Ewalt deserve much praise for the many times they critically read the manuscript and gave their input. I would also like to thank Ms. Janey Parris, Senior Program Officer of Health, Guyana, the government officials of the Caribbean Embassies, representatives from the Caribbean Nursing Organizations, educators from the various nursing schools and librarians from the archival institutions and libraries in Trinidad and Tobago and Jamaica. These individuals agreed to face-to-face interviews, answered telephone questions and mailed or faxed information on a regular basis. Much thanks goes to Victor Williams for his computer assistance and to Hannelore Nave for her patience in typing the many versions of this manuscript. On a personal level I would like to thank my niece Eloise Walters for researching information in the nursing libraries in London, England and my husband Clifford for his belief that I could accomplish this task. -

The CDC Guide to Strategies to Support Breastfeeding Mothers And
Contents Using Tis Guide ............................................................................................................................ 1 Introduction ................................................................................................................................... 3 Strategy 1. Maternity care practices ................................................................................................. 5 Strategy 2. Professional education .................................................................................................. 11 Strategy 3. Access to professional support ...................................................................................... 15 Strategy 4. Peer support programs ................................................................................................. 19 Strategy 5. Support for breastfeeding in the workplace .................................................................. 23 Strategy 6. Support for breastfeeding in early care and education................................................... 29 Strategy 7. Access to breastfeeding education and information ...................................................... 33 Strategy 8. Social marketing .......................................................................................................... 37 Strategy 9. Addressing the marketing of infant formula ................................................................. 43 References .................................................................................................................................... -

Arabella D'havé, Chief of Terminologie, Classification
Usability of SNOMED CT for secondary use of data in nursing Arabella D’Havé, Chief of Terminologie, Classification, Grouping & Audit Belgian Federal Public Service of Health, Food Chain Safety and Environment Terminology Center ABSTRACT RESULTS Objective: To create an interoperable list of SNOMED CT concepts pertinent to According to the purpose of the study, a total number of 405,131 nursing concepts nursing practice through cross-mapping of seven standardized nursing languages were extracted from UMLS. For each interface terminology of nursing, the number of recognized as interface nursing terminologies to support secondary use of data. unique concepts was extracted, 410 concepts from the Clinical Care Classification Design: The UMLS Metathesaurus was queried in order to retrieve all SNOMED CT (CCC; formerly Home Health Care Classification), 1,689 concepts from the concepts where the concept was also represented within seven standardized nursing International Classification for Nursing Practice (ICNP), 237 concepts from the NANDA- languages recognized both nationally and internationally for use as an interface International (NANDA-I; Nursing Diagnosis Classification), 11,255 from the Nursing terminology in paper-based as well as electronic health records. A candidate list of Intervention Classification (NIC), 5,707 from the Nursing Outcome Classification SNOMED CT concepts was retrieved and presented to a project team in the University (NOC), 554 from the Omaha System, 199 from the Perioperative Nursing Data Set Hospitals Leuven in order to validate the SNOMED CT concepts that are present or (PNDS), 9,065 from the ABC Coding Solutions system, and 376,015 from the Logical missing from this list to accommodate with the mandatory Minimum Nursing Dataset Observation Identifiers Names and Codes (LOINC). -

FALL/WINTER 2019 DREAMING INSIDE THIS a Natural Fit ISSUE UNC Anesthesiology Comes to Wayne UNC Health Care
Carolina UNC ANESTHESIOLOGY NEWS VOLUME 4 • ISSUE 2 FALL/WINTER 2019 DREAMING INSIDE THIS A Natural Fit ISSUE UNC Anesthesiology Comes to Wayne UNC Health Care UNC Joins Wayne Anesthesiology Numbers at a Glance Chairman's Note New Hires Leadership Recognition Residency Update Spotlight on Fellows Mauck Burn Research Photo Gallery January – June 2019 Faculty Publications, Awards & Presentations Upcoming Events MAKE A GIFT L to R: Wayne UNC Health Care anesthesiologists Drs. Al Melvin, Voltaire Misa, Jamie Cummings (top) and Peter Fischer (bottom) Support the missions of UNC Department of sk UNC faculty anesthesiologists how it’s gone since joining Wayne UNC Health Care’s anesthesia care Anesthesiology by donating team this year. Sit with Wayne’s clinical supervisor for managerial perspective on whether the hospital's med.unc.edu/ CRNAs are applying their peri-anesthesia scope of practice under new physicians. Stop by pre-op for anesthesiology/donate nursing input on the feel of team communications working alongside UNC anesthesiologists. The feedback from all Abrings one to mind spelling a positive outlook for anesthesia care delivery at Wayne as UNC faculty anesthesiologists take the helm — cohesion. For more information Onboarding five UNC anesthesiologists at Wayne by year’s end is not only welcome; it’s also timely. In September www.med.unc.edu/anesthesiology 2019, construction and renovation of a surgical pavilion project was completed adding almost 100K square feet to Wayne’s operating rooms (ORs). This massive undertaking modernized 12 ORs, four procedural rooms, one endoscopy/ERCP suite and one labor & delivery unit, among others. Overhauled surgical areas provide UNC anesthesiologists an early-stage opportunity to build workplace perioperative relationships with Wayne’s pre- and Visit us on Facebook post-op nurses, Certified Registered Nurse Anesthetists (CRNAs) and OR personnel. -

Heritage Society Dinner and Silent Auction Leadership Education
September 2018 Heritage Society Dinner and Silent Auction The next Heritage Society Dinner and Silent Auction will be held 17 November 2019 during the 45th Biennial Convention. Heritage Society donors will enjoy dinner and a silent auction with many lovely and fun items to bid on. The dinner will be within walking distance of the convention center at the Riverview Ballroom at the Gaylord National Resort and Convention Center. The room offers some stunning views of the Potomac River. Check them out in this short video. We hope to see you there. Leadership Education Grant Recipients Thirty-two Sigma members attended the 29th International Nursing Research Congress in Melbourne, Australia, 19-23 July 2018, after receiving Leadership Education Grants. Heritage Society donors attending congress were able to meet the grant recipients at a meet and greet on 19 July. New Heritage Society Donors We gratefully recognize the newest Heritage Society donors who've made their commitment to support nursing worldwide. Virginia Henderson Fellows Christine Alichnie, PhD, RN Chair and Professor Emeriti Bloomsburg University of Pennsylvania President PNC-ARE, Inc. Theta Zeta and Xi Chapters Mountain Top, Pennsylvania, USA Amita Avadhani, DNP, DCC, ACNP, ANP, CCRN, FAANP Associate Professor, Post Masters DNP Executive Model Specialty Director Rutgers University School of Nursing Newark Alpha Tau Chapter New Jersey, USA Mary Bemker, PhD, RN Faculty Walden University School of Nursing Iota Gamma Chapter Louisville, Kentucky, USA News About Fellows The following individuals are serving on the 2017-2019 Sigma Marketplace Board of Directors. Sue Haddock Debra Heinrich Donna Nickitas (Secretary) Terry Siek The following individuals are serving on the 2017-2019 Sigma Building Corporation Board of Directors. -

Cross-Mapping the ICNP with NANDA, HHCC, Omaha System and NIC for Unified Nursing Language System Development
Original article Cross-mapping the ICNP with NANDA, HHCC, Omaha System and NIC for unified nursing language system development S. Hyun MSN, RN & H. A. Park PhD, RN 1 Researcher, College of Nursing Seoul National University, Seoul, Korea 2 Associate Professor, College of Nursing Seoul National University, Seoul, Korea Keywords Abstract Cross-mapping, ICNP, Nursing language plays an important role in describing and defining nursing Nursing Languages, Unified Nursing phenomena and nursing actions. There are numerous vocabularies describing Language System nursing diagnoses, interventions and outcomes in nursing. However, the lack of a standardized unified nursing language is considered a problem for further development of the discipline of nursing. In an effort to unify the nursing languages, the International Council of Nurses (ICN) has proposed the International Classification for Nursing Practice (ICNP) as a unified nursing language system. The purpose of this study was to evaluate the inclusiveness and expressiveness of the ICNP terms by cross-mapping them with the existing nursing terminologies, specifically the North American Nursing Diagnosis Association (NANDA) taxonomy I, the Omaha System, the Home Health Care Classification (HHCC) and the Nursing Interventions Classification (NIC). Nine hundred and seventy-four terms from these four classifications were cross-mapped with the ICNP terms. This was performed in accordance with the Guidelines for Composing a Nursing Diagnosis and Guidelines for Composing a Nursing Intervention, which were suggested by the ICNP development team. An expert group verified the results. The ICNP Phenomena Classification described 87.5% of the NANDA diagnoses, 89.7% of the HHCC diagnoses and 72.7% of the Omaha System problem classification scheme. -

Features of Computerized Clinical Decision Support Systems
CIN: Computers, Informatics, Nursing & Vol. 31, No. 10, 477–495 & Copyright B 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins CONTINUING EDUCATION 2.4 ANCC Contact Hours Features of This study aimed to organize the system features Computerized Clinical of decision support technologies targeted at nurs- ing practice into assessment, problem identifi- Decision Support cation, care plans, implementation, and outcome evaluation. It also aimed to identify the range of the five stage-related sequential decision supports Systems Supportive of that computerized clinical decision support sys- tems provided. MEDLINE, CINAHL, and EMBASE Nursing Practice were searched. A total of 27 studies were reviewed. The system features collected represented the A Literature Review characteristics of each category from patient as- sessment to outcome evaluation. Several features SEONAH LEE, PhD, MSN, RN were common across the reviewed systems. For the sequential decision support, all of the reviewed systems provided decision support in sequence for patient assessment and care plans. Fewer than half of the systems included problem identification. There were only three systems operating in an im- According to the Institute of Medicine,1 the development plementation stage and four systems in outcome and implementation of more sophisticated information evaluation. Consequently, the key steps for sequen- systems are essential not only to enhance quality and ef- tial decision support functions were initial patient ficiency of patient care but also to support clinical deci- assessment, problem identification, care plan, and sion making. Clinical decision support becomes more and outcome evaluation. Providing decision support in such a full scope will effectively help nurses’ clinical more a core function of health information systems to elim- 2 decision making. -
Nursing Diagnoses 2015-2017
NURSING DIAGNOSES 20mm Definitions and Classification NANDA International, Inc. NURSING DIAGNOSES: DEFINITIONS & CLASSIFICATION 2015–2017 NANDA International, Inc. NURSING DIAGNOSES: DEFINITIONS & CLASSIFICATION 2015–2017 Tenth Edition Edited by T. Heather Herdman, PhD, RN, FNI and Shigemi Kamitsuru, PhD, RN, FNI This edition first published 2014 © 2014, 2012, 2009, 2007, 2005, 2003, 2001, 1998, 1996, 1994 by NANDA International, Inc. Registered Office John Wiley & Sons, Ltd., The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial Offices 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 1606 Golden Aspen Drive, Suites 103 and 104, Ames, Iowa 50010, USA For details of our global editorial offices, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identified as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. Designations used by companies to distinguish their products are often claimed as trademarks. All brand names and product names used in this book are trade names, service marks, trademarks or registered trademarks of their respective owners. The publisher is not associated with any product or vendor mentioned in this book. -

Bowles CV March 2021.Pdf
KATHRYN H. BOWLES, PH.D., RN, FAAN, FACMI February 2021 BUSINESS ADDRESS HOME ADDRESS University of Pennsylvania, School of Nursing 1435 Wynnemoor Way 418 Curie Boulevard, 340 Claire Fagin Hall Fort Washington, PA 19034 Philadelphia, PA 19104 215-628-2056 215-898-0323 [email protected] EDUCATION Certificate 1999 National Library of Medicine Fellowship, Marine Biological Lab, Woods Hole, MA Medical Informatics PhD 1996 University of Pennsylvania Philadelphia, PA Major: Nursing MSN 1990 Villanova University Villanova, PA Major: Nursing Education, Summa Cum Laude BSN 1978 Edinboro University of Pennsylvania Edinboro, PA Major: Nursing, Magna Cum Laude ACADEMIC POSITIONS 2012 - present Professor and van Ameringen Chair in Nursing Excellence Director of the Health Informatics Minor University of Pennsylvania School of Nursing, Senior Fellow, Leonard Davis Institute of Economics Fellow, Institute of Biomedical Informatics, Perelman School of Medicine Philadelphia, PA 2013-2019 Adjunct Professor of Nursing, Hong Kong Polytechnic University, Hong Kong 2012 - 2016 Director of the Center for Integrative Sciences in Aging, University of Pennsylvania School of Nursing 1 2003 - 2012 Associate Professor with Tenure Director of the Health Informatics Minor, Director of Nursing Research, Visiting Nurse Association of Greater Philadelphia (1997-2005) Senior Fellow, Leonard Davis Institute of Economics Biobehavioral Health Sciences Division University of Pennsylvania School of Nursing 2001 - 2003 Assistant Professor Foundational Science Division -

Florida School Health Administrative Guidelines
Florida School Health Administrative Guidelines Permission to duplicate and distribute granted. April 2007 Updated May 2012 John H. Armstrong, M.D. State Surgeon General Acknowledgements Revision Reviewers (2012) • Florida Department of Health: County Health Departments o Collier County o Escambia County o Hernando County o Highlands County o Hillsborough County o Marion County o Orange County o Palm Beach County o Pinellas County o St. Johns County o St. Lucie County o Santa Rosa County o Seminole County o Suwannee County • Florida Department of Health: Tallahassee Central Office o Division of Family Health Services o Office of General Counsel o Bureau of Immunization o Division of Medical Quality Assurance o Office of Public Health Nursing o School Health Services Program • Florida Department of Education o Student Support Services Project • Florida County School Districts o Citrus County o Clay County o Escambia County o Lee County o Palm Beach County o Pasco County o Pinellas County o Seminole County o St. Johns County o Suwannee County o Volusia County Florida School Health Administrative Guidelines i April, 2007 Updated, May 2012 Table of Contents Section I: Introduction to School Health Services Purpose of the School Health Administrative Guidelines ………...............…......... I - 2 School Health Mission Statement ……...................................…..............…..…… I - 2 Overview of School Health Services …………………...........…………………....... I - 2 Responsibility for School Health Services .........................................…………….