Nursing Diagnoses 2015-2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Competency in School Nurse Practice
COMPETENCY IN SCHOOL NURSE PRACTICE CONNECTICUT STATE DEPARTMENT OF EDUCAtion – 2009 CONNECTICUT STATE DEPARTMENT OF EDUCATION Mark K. McQuillan, Commissioner George A. Coleman, Deputy Commissioner Division of Family and Student Support Services Charlene Russell-Tucker, Associate Commissioner Bureau of Health/Nutrition, Family Services and Adult Education Paul Flinter, Chief Cheryl-Ann Resha, R.N., Project Manager Publications Unit Donald G. Goranson, Jr., Editor Andrea Wadowski, Graphic Designer Janet Montague, Desktop Publisher Competency in SCHOOL NURSE PRActice CONNECTICUT STATE DEPARTMENT OF EDUCAtion This document is available on the Connecticut State Department of Education Web site at: http://www.ct.gov/sde/cwp/view.asp?q=2678&q=320768 ii COMPETENCY IN SCHOOL NURSE PRACTICE CONTENTs S ACKNOWLEDGMENTS ..................................................................................................................... iv PREFACE .............................................................................................................................................. v INTRODUCTION ................................................................................................................................ 1 Purpose ..........................................................................................................................................1 Highly Qualified Professionals .......................................................................................................1 COMPETENCIES ................................................................................................................................ -
Assessment Module
Assessment Module 1 | Page Assessment May 2017 Table of Contents About this Module/Overview/Objectives……………………………………………...Page 3 Pre-test…………………………………………………………………………………Pages 4-5 Chapter 1……………………………………………………………………………....Pages 6-12 Overview Focused Assessment vs. Comprehensive Assessment Considerations in preparing for a physical exam Geriatric Assessment Nursing Components Considerations in Elderly Residents Chapter 2……………………………………………………………………………...Pages 12-14 Root Cause of Behaviors Physiologic Social Environmental Psychosocial Chapter 3……………………………………………………………………………...Pages 14-16 Risk Assessment Eyes Ears Hemiparesis Paraplegia Where to place the resident in the room Chapter 4……………………………………………………………...………………Pages 16-18 Texas Board of Nursing and Assessments Federal Nursing Facility Regulations F272: Comprehensive Assessments State Nursing Facility Regulations Chapter 5………………………………………………………………………….......Pages 18-19 Resources “This is me” “This is me: My Care Passport” Alternate Communication Boards Pain, Pain Go Away Presentation Appendices……………………………………………………………………………Pages 20-48 2 | Page Assessment May 2017 About this Module: Assessment is a key component of nursing practice, required for planning and the provision of resident and family centered care. Information that is obtained from an accurate assessment serves as the foundation for age-appropriate nursing care, enhancing the residents’ quality of life and independence. The LVN must have a specific set of skills in order to adequately and effectively assess the resident, including: a physical assessment; a functional assessment; and any additional information about the resident that would be used to develop the care plan. This module will provide you with all of the information necessary to ensure adequate assessments are completed for each resident in the facility, meeting the state and federal requirements for resident assessment. Overview: Conditions such as functional impairment and dementia are common in nursing home residents. -
A Presentation of Post-Licensure Nursing Education Programs in California
California Board of Registered Nursing 2016-2017 Annual School Report Data Summary and Historical Trend Analysis A Presentation of Post-Licensure Nursing Education Programs in California July 9, 2018 Prepared by: Lisel Blash, MS, MPA Joanne Spetz, PhD University of California, San Francisco 3333 California Street, Suite 265 San Francisco, CA 94118 CONTENTS PREFACE AND SURVEY METHODS .............................................................................................................. 3 NURSING EDUCATION SURVEY DESIGN ............................................................................................................. 3 SURVEY PARTICIPATION ................................................................................................................................... 3 ANALYSIS ......................................................................................................................................................... 4 POST-LICENSURE RN EDUCATION PROGRAM SUMMARY AND TRENDS .............................................. 5 RN-TO-BSN PROGRAMS .................................................................................................................................. 5 Number of RN-to-BSN Programs .............................................................................................................. 5 Program Information .................................................................................................................................. 5 New Student Enrollments ......................................................................................................................... -
How to Display Your Credentials
How to Display Your Credentials How to display your credentials Common questions and answers about displaying your credentials in the proper order why do we need a standard other certifications include non-nursing way to list credentials? certifications that recognize additional skills. One example is the EMT-Basic/EMT, awarded by the Having a standard way ensures that everyone— National Registry of Emergency Medical Technicians. including nurses, healthcare providers, consumers, third-party payers, and government officials— understands the significance and value of credentials. what credentials do i Have to use? On legal documents such as prescriptions and notes what is the preferred order of credentials? on medical records, you must use the credentials required by your state for your area of practice, for The preferred order is: example, Susan Jones, RN, or Joyce Smith, APRN. Highest earned degree In professional endeavors such as speaking, Licensure writing for publication, or providing testimony State designations or requirements before a legislative body, use all your relevant National certifications credentials. Note that journals sometimes order Awards and honors credentials differently, and it is acceptable to conform to their style. Other recognitions what if i Have More than one why is this order recommended? of the same type of credential? The education degree comes first because it is List the highest education degree first, for example, a “permanent” credential, meaning it cannot be Michael Anderson, PhD, MSN. In most cases, one taken away except under extreme circumstances. degree is enough, but if your second degree is in The next two credentials (licensure and state another relevant field, you may choose to list it. -

MIGRATION of NURSING and MIDWIFERY WORKFORCE in the STATE of KERALA This Report Was Prepared by Researchers from Oxford Policy Management (Krishna D
CASE STUDY | INDIA FROM BRAIN DRAIN TO BRAIN GAIN MIGRATION OF NURSING AND MIDWIFERY WORKFORCE IN THE STATE OF KERALA This report was prepared by researchers from Oxford Policy Management (Krishna D. Rao, Aarushi Bhatnagar, Radhika Arora, Swati Srivastava, Udit Ranjan), the Centre for Development Studies, Trivandrum (S. Irudaya Rajan, Sunitha Syam), the Health Systems Research India Initiative (Arun Nair, S.J. Sini Thomas), and the WHO Country Office for India (Tomas Zapata). Please address all correspondence to Krishna D. Rao ([email protected]) and Aarushi Bhatnagar ([email protected]) © WHO, all rights reserved November 2017 Contents Acknowledgements .......................................................3 6. Discussion ....................................... 29 Abbreviations ...............................................................4 6.1 Production, stock and migration of nurses ....... 29 6.1.1 Production ...................................... 29 Executive summary ........................................................5 6.1.2 Stock .............................................. 30 1. Background ........................................ 7 6.1.3 Migration ........................................ 31 6.2 Factors influencing migration patterns ............ 33 1.1 Kerala state ..................................................9 6.2.1 Endogenous push and pull factors ....... 33 1.2 Migration of health workers........................... 10 6.2.2 Exogenous push and pull factors .........34 2. Objectives ....................................... -

Nursing Research: Challenges
NURSING RESEARCH: CHALLENGES AND OPPORTUNITIES PRESENTED BY OPARA HOPE CHIZOLUM AT GLOBAL RESEARCH NURSES WORKSHOP 24th and 25th May 2021 NNAMDI AZIKIWE UNIVERSITY TEACHING HOSPITAL, NNEWI OUTLINE FOR THE PRESENTATION INTRODUCTION WHAT IS NURSING RESEARCH? IMPORTANCE OF RESEARCH TO NURSING WHAT ARE THE OPPORTUNITIES? CHALLENGES FACED BY NURSE RESEARCHERS WAY FORWARD CONCLUSION INTRODUCTION Research is a way of thinking: examining critically the various aspects of your day-to-day work; understanding and formulating guiding principles that govern a procedure; and developing and, testing new theories that contribute to the advancement of your practice and profession (Odunze, 2019). It is a habit of questioning what you do, and a systematic examination of clinical observations to explain and find answers for what you perceive, with a view to instituting appropriate changes for a more effective professional service (Kumar et al, 2016) Today’s healthcare system is complex, and patients have increasingly varied needs. Developing solutions for the health issues of diverse populations requires providers with many different perspectives (National Institute of Nursing Research, 2016). Nurses provide direct care to their patients on a daily basis, so they know which approaches work well and which need adjusting. Nursing concerns are the heart of nursing research. even when nurses want to improve care through research findings, several barriers have hindered the progress. WHAT IS NURSING RESEARCH? Nursing research is research that provides a body of knowledge and evidence used to support nursing practices (the American Association of Colleges of Nursing, 2016) . Evidence-based practice requires using research outcomes to drive clinical decisions and care. -

Nursing Students' Perspectives on Telenursing in Patient Care After
Clinical Simulation in Nursing (2015) 11, 244-250 www.elsevier.com/locate/ecsn Featured Article Nursing Students’ Perspectives on Telenursing in Patient Care After Simulation Inger Ase Reierson, RN, MNSca,*, Hilde Solli, RN, MNSc, CCNa, Ida Torunn Bjørk, RN, MNSc, Dr.polit.a,b aFaculty of Health and Social Studies, Institute of Health Studies, Telemark University College, 3901 Porsgrunn, Norway bFaculty of Medicine, Institute of Health and Society, Department of Nursing Science, University of Oslo, 0318 Oslo, Norway KEYWORDS Abstract telenursing; Background: This article presents the perspectives of undergraduate nursing students on telenursing simulation; in patient care after simulating three telenursing scenarios using real-time video and audio nursing education; technology. information and Methods: An exploratory design using focus group interviews was performed; data were analyzed us- communication ing qualitative content analysis. technology; Results: Five main categories arose: learning a different nursing role, influence on nursing assessment qualitative content and decision making, reflections on the quality of remote comforting and care, empowering the pa- analysis tient, and ethical and economic reflections. Conclusions: Delivering telenursing care was regarded as important yet complex activity. Telenursing simulation should be integrated into undergraduate nursing education. Cite this article: Reierson, I. A., Solli, H., & Bjørk, I. T. (2015, April). Nursing students’ perspectives on telenursing in patient care after simulation. Clinical Simulation in Nursing, 11(4), 244-250. http://dx.doi.org/ 10.1016/j.ecns.2015.02.003. Ó 2015 International Nursing Association for Clinical Simulation and Learning. Published by Elsevier Inc. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/ by-nc-nd/4.0/). -
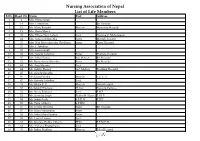
Nursing Association of Nepal List of Life Members S.No
Nursing Association of Nepal List of Life Members S.No. Regd. No. Name Post Address 1 2 Mrs. Prema Singh 2 14 Mrs. I. Mathema Bir Hospital 3 15 Ms. Manu Bangdel Matron Maternity Hospital 4 19 Mrs. Geeta Murch 5 20 Mrs. Dhana Nani Lohani Lect. Nursing C. Maharajgunj 6 24 Mrs. Saraswati Shrestha Sister Mental Hospital 7 25 Mrs. Nati Maya Shrestha (Pradhan) Sister Kanti Hospital 8 26 Mrs. I. Tuladhar 9 32 Mrs. Laxmi Singh 10 33 Mrs. Sarada Tuladhar Sister Pokhara Hospital 11 37 Mrs. Mita Thakur Ad. Matron Bir Hospital 12 42 Ms. Rameshwori Shrestha Sister Bir Hospital 13 43 Ms. Anju Sharma Lect. 14 44 Ms. Sabitry Basnet Ast. Matron Teaching Hospital 15 45 Ms. Sarada Shrestha 16 46 Ms. Geeta Pandey Matron T.U.T. H 17 47 Ms. Kamala Tuladhar Lect. 18 49 Ms. Bijaya K. C. Matron Teku Hospital 19 50 Ms.Sabitry Bhattarai D. Inst Nursing Campus 20 52 Ms. Neeta Pokharel Lect. F.H.P. 21 53 Ms. Sarmista Singh Publin H. Nurse F. H. P. 22 54 Ms. Sabitri Joshi S.P.H.N F.H.P. 23 55 Ms. Tuka Chhetry S.P.HN 24 56 Ms. Urmila Shrestha Sister Bir Hospital 25 57 Ms. Maya Manandhar Sister 26 58 Ms. Indra Maya Pandey Sister 27 62 Ms. Laxmi Thakur Lect. 28 63 Ms. Krishna Prabha Chhetri PHN F.P.M.C.H. 29 64 Ms. Archana Bhattacharya Lect. 30 65 Ms. Indira Pradhan Matron Teku Hospital S.No. Regd. No. Name Post Address 31 67 Ms. -

HMP Kingston
Report on an announced inspection of HMP Kingston 16–20 August 2010 by HM Chief Inspector of Prisons Crown copyright 2010 Printed and published by: Her Majesty’s Inspectorate of Prisons 1st Floor, Ashley House Monck Street London SW1P 2BQ England HMP Kingston 2 Contents Introduction 5 Fact page 7 Healthy prison summary 9 1 Arrival in custody Courts, escorts and transfers 17 First days in custody 17 2 Environment and relationships Residential units 21 Staff-prisoner relationships 23 Personal officers 24 3 Duty of care Bullying and violence reduction 27 Self-harm and suicide 29 Applications and complaints 30 Legal rights 31 Faith and religious activity 32 Substance use 33 4 Diversity Diversity 35 Race equality 36 Religion 38 Foreign nationals 38 Disability and older prisoners 39 Sexual orientation 41 5 Health services General 43 Clinical governance 44 Primary care 45 Pharmacy 46 Dentistry 47 Secondary care 48 Mental health 48 HMP Kingston 3 6 Activities Learning and skills and work activities 49 Physical education and health promotion 53 Time out of cell 55 7 Good order Security and rules 57 Discipline 58 Incentives and earned privileges 60 8 Services Catering 63 Prison shop 64 9 Resettlement Strategic management of resettlement 67 Offender management and planning 68 Resettlement pathways 71 10 Recommendations, housekeeping points and good practice 77 Appendices I Inspection team 86 II Prison population profile 87 III Summary of prisoner questionnaires and interviews 89 HMP Kingston 4 Introduction Kingston is a small specialist prison for life- and other indeterminate-sentenced prisoners. This very positive report, of a full announced inspection, is testament to the benefits that can flow from having a small-scale niche prison, with a settled population. -

Lawrlwytho'r Atodiad Gwreiddiol
Operational services structure April 2021 14/04/2021 Operational Leadership Structures Director of Operations Director of Nursing & Quality Medical Director Lee McMenamy Joanne Hiley Dr Tessa Myatt Medical Operations Operations Clinical Director of Operations Deputy Director of Nursing & Deputy Medical Director Hazel Hendriksen Governance Dr Jose Mathew Assistant Clinical Director Assistant Director of Assistant Clinical DWiraerctringor ton & Halton Operations Corporate Corporate Lorna Pink Assistant Assistant Director Julie Chadwick Vacant Clinical Director of Nursing, AHP & Associate Clinical Director Governance & Professional Warrington & Halton Compliance Standards Assistant Director of Operations Assistant Clinical Director Dr Aravind Komuravelli Halton & Warrington Knowsley Lee Bloomfield Claire Hammill Clare Dooley Berni Fay-Dunkley Assistant Director of Operations Knowsley Associate Medical Director Nicky Over Assistant Clinical Director Allied Health Knowsley Assistant Director of Sefton Professional Dr Ashish Kumar AssiOstapenrta Dtiironesc tKnor oofw Oslpeeyr ations Sara Harrison Lead Nicola Over Sefton James Hester Anne Tattersall Assistant Clinical Director Associate Clinical Director Assistant Director of St Helens & Knowsley Inpatients St Helens Operations Sefton Debbie Tubey Dr Raj Madgula AssistanAt nDniree Tcatttore ofrs aOllp erations Head of St Helens & Knowsley Inpatients Safeguarding Tim McPhee Assistant Clinical Director Sarah Shaw Assistant Director of Associate Medical Director Operations St Helens Mental Health -

Use of Nursing Diagnosis in CA Nursing Schools
USE OF NURSING DIAGNOSIS IN CALIFORNIA NURSING SCHOOLS AND HOSPITALS January 2018 Funded by generous support from the California Hospital Association (CHA) Copyright 2018 by HealthImpact. All rights reserved. HealthImpact 663 – 13th Street, Suite 300 Oakland, CA 94612 www.healthimpact.org USE OF NURSING DIAGNOSIS IN CALIFORNIA NURSING SCHOOLS AND HOSPITALS INTRODUCTION As part of the effort to define the value of nursing, a common language continues to arise as a central issue in understanding, communicating, and carrying out nursing's unique role in identifying and treating patient response to illness. The diagnostic process and evidence-based interventions developed and subsequently implemented by a practice discipline describe its unique contribution, scope of accountability, and value. The specific responsibility registered nurses (RN) have in assessing patient response to health and illness and determining evidence-based etiology is within the realm of nursing’s autonomous scope of practice, and is referred to as nursing diagnosis. It is an essential element of the nursing process and is followed by implementing specific interventions within nursing’s scope of practice, providing evidence that links professional practice to health outcomes. Conducting a comprehensive nursing assessment leading to the accurate identification of nursing diagnoses guides the development of the plan of care and specific interventions to be carried out. Assessing the patient’s response to health and illness encompasses a wide range of potential problems and actual concerns to be addressed, many of which may not arise from the medical diagnosis and provider orders alone, yet can impede recovery and impact health outcomes. Further, it is critically important to communicate those problems, potential vulnerabilities and related plans of care through broadly understood language unique to nursing. -

Assignment Is a Complementary Relationship Between Nurse and Bhts and Bhas That Results in Safe and Efficient Patient Care If It Is Used Appropriately
Unity Center for Behavioral Health Assignment is a complementary relationship between nurse and BHTs and BHAs that results in safe and efficient patient care if it is used appropriately. It is a critical step in the delivery of nursing care. This Photo by Unknown Author is licensed under CC BY-SA-NC 1) Define assignment and how it relates to nursing practice. 2) Explain the difference between assignment and delegation. 3) Define the roles and responsibilities within assignments of BHTs and BHAs. 4) Review the the correct steps when assigning tasks to BHTs and BHAs. 5) Review assignments, ethics and standards specific to the psychiatric mental health nurse. Assignment has a specific meaning in the Nurse Practice Act. OAR 851-06 defines the term assign as “...directing and distributing, within a given work period, the work that each staff member is already authorized by license or certification and organizational position description to perform.” Unlicensed assistive personnel (UAP) are unlicensed health care providers trained to function in a supportive role by providing patient/client care activities. When the activity to be performed is within the UAP’s position description, and there is documented education and current competency validation of the UAP having been done by the organization employing both the RN and the UAP staff member. The UAP is held accountable for the performance of their role. KEY POINT: The RN, determines the appropriate match between the patient and BHT or BHA, and assigns a task to the BHT or BHA based on their competency and job description. If a BHT or BHA does not perform their assigned task, the RN is NOT held responsible.