NANDA Nursing Diagnosis 2018-2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
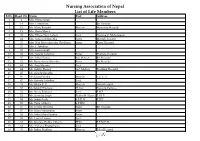
Nursing Association of Nepal List of Life Members S.No
Nursing Association of Nepal List of Life Members S.No. Regd. No. Name Post Address 1 2 Mrs. Prema Singh 2 14 Mrs. I. Mathema Bir Hospital 3 15 Ms. Manu Bangdel Matron Maternity Hospital 4 19 Mrs. Geeta Murch 5 20 Mrs. Dhana Nani Lohani Lect. Nursing C. Maharajgunj 6 24 Mrs. Saraswati Shrestha Sister Mental Hospital 7 25 Mrs. Nati Maya Shrestha (Pradhan) Sister Kanti Hospital 8 26 Mrs. I. Tuladhar 9 32 Mrs. Laxmi Singh 10 33 Mrs. Sarada Tuladhar Sister Pokhara Hospital 11 37 Mrs. Mita Thakur Ad. Matron Bir Hospital 12 42 Ms. Rameshwori Shrestha Sister Bir Hospital 13 43 Ms. Anju Sharma Lect. 14 44 Ms. Sabitry Basnet Ast. Matron Teaching Hospital 15 45 Ms. Sarada Shrestha 16 46 Ms. Geeta Pandey Matron T.U.T. H 17 47 Ms. Kamala Tuladhar Lect. 18 49 Ms. Bijaya K. C. Matron Teku Hospital 19 50 Ms.Sabitry Bhattarai D. Inst Nursing Campus 20 52 Ms. Neeta Pokharel Lect. F.H.P. 21 53 Ms. Sarmista Singh Publin H. Nurse F. H. P. 22 54 Ms. Sabitri Joshi S.P.H.N F.H.P. 23 55 Ms. Tuka Chhetry S.P.HN 24 56 Ms. Urmila Shrestha Sister Bir Hospital 25 57 Ms. Maya Manandhar Sister 26 58 Ms. Indra Maya Pandey Sister 27 62 Ms. Laxmi Thakur Lect. 28 63 Ms. Krishna Prabha Chhetri PHN F.P.M.C.H. 29 64 Ms. Archana Bhattacharya Lect. 30 65 Ms. Indira Pradhan Matron Teku Hospital S.No. Regd. No. Name Post Address 31 67 Ms. -

Lawrlwytho'r Atodiad Gwreiddiol
Operational services structure April 2021 14/04/2021 Operational Leadership Structures Director of Operations Director of Nursing & Quality Medical Director Lee McMenamy Joanne Hiley Dr Tessa Myatt Medical Operations Operations Clinical Director of Operations Deputy Director of Nursing & Deputy Medical Director Hazel Hendriksen Governance Dr Jose Mathew Assistant Clinical Director Assistant Director of Assistant Clinical DWiraerctringor ton & Halton Operations Corporate Corporate Lorna Pink Assistant Assistant Director Julie Chadwick Vacant Clinical Director of Nursing, AHP & Associate Clinical Director Governance & Professional Warrington & Halton Compliance Standards Assistant Director of Operations Assistant Clinical Director Dr Aravind Komuravelli Halton & Warrington Knowsley Lee Bloomfield Claire Hammill Clare Dooley Berni Fay-Dunkley Assistant Director of Operations Knowsley Associate Medical Director Nicky Over Assistant Clinical Director Allied Health Knowsley Assistant Director of Sefton Professional Dr Ashish Kumar AssiOstapenrta Dtiironesc tKnor oofw Oslpeeyr ations Sara Harrison Lead Nicola Over Sefton James Hester Anne Tattersall Assistant Clinical Director Associate Clinical Director Assistant Director of St Helens & Knowsley Inpatients St Helens Operations Sefton Debbie Tubey Dr Raj Madgula AssistanAt nDniree Tcatttore ofrs aOllp erations Head of St Helens & Knowsley Inpatients Safeguarding Tim McPhee Assistant Clinical Director Sarah Shaw Assistant Director of Associate Medical Director Operations St Helens Mental Health -

Use of Nursing Diagnosis in CA Nursing Schools
USE OF NURSING DIAGNOSIS IN CALIFORNIA NURSING SCHOOLS AND HOSPITALS January 2018 Funded by generous support from the California Hospital Association (CHA) Copyright 2018 by HealthImpact. All rights reserved. HealthImpact 663 – 13th Street, Suite 300 Oakland, CA 94612 www.healthimpact.org USE OF NURSING DIAGNOSIS IN CALIFORNIA NURSING SCHOOLS AND HOSPITALS INTRODUCTION As part of the effort to define the value of nursing, a common language continues to arise as a central issue in understanding, communicating, and carrying out nursing's unique role in identifying and treating patient response to illness. The diagnostic process and evidence-based interventions developed and subsequently implemented by a practice discipline describe its unique contribution, scope of accountability, and value. The specific responsibility registered nurses (RN) have in assessing patient response to health and illness and determining evidence-based etiology is within the realm of nursing’s autonomous scope of practice, and is referred to as nursing diagnosis. It is an essential element of the nursing process and is followed by implementing specific interventions within nursing’s scope of practice, providing evidence that links professional practice to health outcomes. Conducting a comprehensive nursing assessment leading to the accurate identification of nursing diagnoses guides the development of the plan of care and specific interventions to be carried out. Assessing the patient’s response to health and illness encompasses a wide range of potential problems and actual concerns to be addressed, many of which may not arise from the medical diagnosis and provider orders alone, yet can impede recovery and impact health outcomes. Further, it is critically important to communicate those problems, potential vulnerabilities and related plans of care through broadly understood language unique to nursing. -

Nursing Documentation in Clinical Practice
From the Department of Nursing, Karolinska Institutet, Stockholm, Sweden Nursing Documentation in Clinical Practice Instrument development and evaluation of a comprehensive intervention programme Catrin Björvell Stockholm 2002 Nursing Documentation in Clinical Practice Instrument development and effects of a comprehensive education programme By: Catrin Björvell Cover layout: Tommy Säflund Printed at: ReproPrint AB, Stockholm ISBN 91-7349-297-3 NURSING DOCUMENTATION IN CLINICAL PRACTICE There is nothing more difficult to carry out, nor more doubtful of success, nor more dangerous to handle than to initiate a new order of thing. Machiavelli, The Prince Nursing documentation in clinical practice Instrument development and evaluation of a comprehensive intervention programme Catrin Björvell, Department of Nursing, Karolinska Institutet, Stockholm, Sweden Abstract The purpose of this study was to describe and analyse effects of a two-year comprehensive intervention concerning nursing documentation in patient records when using the VIPS model - a model designed to structure nursing documentation. Registered Nurses (RNs) from three acute care hospital wards participated in a two-year intervention programme, in addition, a fourth ward was used for comparison. The intervention consisted of education about nursing documentation in accordance with the VIPS model and organisational changes. To evaluate effects of the intervention patient records (n=269) were audited on three occasions: before the intervention, immediately after the intervention and three years after the intervention. For this purpose, a patient record audit instrument, the Cat-ch-Ing, was constructed and tested. The instrument aims at measuring both quantitatively and qualitatively to what extent the content of the nursing process is documented in the patient record. -

THE DEVELOPMENT of NURSING EDUCATION in the ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I
THE DEVELOPMENT OF NURSING EDUCATION IN THE ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I. GARDNER, B.S.N., M.S.N., M.Ed. A DISSERTATION IN HIGHER EDUCATION Submitted to the Graduate Faculty of Texas Tech University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF EDUCATION Approved Accepted Dean of the Graduate School August, 1993 ft 6 l^yrr^7^7 801 J ,... /;. -^o ACKNOWLEDGEMENTS C?^ /c-j/^/ C^ ;^o.^^ I would like to thank Dr. Clyde Kelsey, Jr., for his C'lp '^ ^unflagging support, his advice and his constant vigil and encouragement in the writing of this dissertation. I would also like to thank Dr. Patricia Yoder-Wise who acted as co-chairperson of my committee. Her advice was invaluable. Drs. Mezack, Willingham, and Ewalt deserve much praise for the many times they critically read the manuscript and gave their input. I would also like to thank Ms. Janey Parris, Senior Program Officer of Health, Guyana, the government officials of the Caribbean Embassies, representatives from the Caribbean Nursing Organizations, educators from the various nursing schools and librarians from the archival institutions and libraries in Trinidad and Tobago and Jamaica. These individuals agreed to face-to-face interviews, answered telephone questions and mailed or faxed information on a regular basis. Much thanks goes to Victor Williams for his computer assistance and to Hannelore Nave for her patience in typing the many versions of this manuscript. On a personal level I would like to thank my niece Eloise Walters for researching information in the nursing libraries in London, England and my husband Clifford for his belief that I could accomplish this task. -

The CDC Guide to Strategies to Support Breastfeeding Mothers And
Contents Using Tis Guide ............................................................................................................................ 1 Introduction ................................................................................................................................... 3 Strategy 1. Maternity care practices ................................................................................................. 5 Strategy 2. Professional education .................................................................................................. 11 Strategy 3. Access to professional support ...................................................................................... 15 Strategy 4. Peer support programs ................................................................................................. 19 Strategy 5. Support for breastfeeding in the workplace .................................................................. 23 Strategy 6. Support for breastfeeding in early care and education................................................... 29 Strategy 7. Access to breastfeeding education and information ...................................................... 33 Strategy 8. Social marketing .......................................................................................................... 37 Strategy 9. Addressing the marketing of infant formula ................................................................. 43 References .................................................................................................................................... -

Nurse Practice Act
Georgia Board of Nursing O.C.G.A. § 43-26 Nurse Practice Act Revised July 2019 Table of Contents Article One Registered Nurses Page Title Code Section Number Short Title O.C.G.A. § 43-26-1 Page 5 Legislative Intent O.C.G.A. § 43-26-2 Page 5 Definitions O.C.G.A. § 43-26-3 Page 5 Georgia Board of Nursing; Membership; Meetings; Officers O.C.G.A. § 43-26-4 Page 8 General Powers and Responsibilities of the Board O.C.G.A. § 43-26-5 Page 9 Use of Certain Titles and Abbreviations by Licensed Nurses O.C.G.A. § 43-26-6 Page 11 Requirements for Licensure as a Registered Professional Nurse O.C.G.A. § 43-26-7 Page 12 Temporary Permits O.C.G.A. § 43-26-8 Page 16 Biennial Renewal of Licenses; Continuing Competency O.C.G.A. § 43-26-9 Page 17 Requirements Inactive Status O.C.G.A. § 43-26-9.1 Page 18 Practicing as a Registered Professional Nurse Without a License O.C.G.A. § 43-26-10 Page 18 Prohibited Denial or Revocation of Licenses; Other Discipline O.C.G.A. § 43-26-11 Page 19 Administration of Anesthesia By Certified Registered Nurse O.C.G.A. § 43-26-11.1 Page 20 Anesthetist Exceptions to Licensure O.C.G.A. § 43-26-12 Page 20 Certain Information Given to the Board by Licensees O.C.G.A. § 43-26-13 Page 23 Article Two Licensed Practical Nurses Page Title Code Section Number Short Title O.C.G.A. -

The Benefits of Using Standardized Nursing Terminology
Page 1 of 20 Selecting a Standardized Terminology for the Electronic Health Record that Reveals the Impact of Nursing on Patient Care By Cynthia B. Lundberg, R.N., BSN; SNOMED Terminology Solutions; Judith J. Warren, PhD, RN, BC, FAAN, FACMI; University of Kansas; Jane Brokel, PhD, RN, NANDA International; Gloria M. Bulechek, PhD, RN, FAAN; Nursing Interventions Classification; Howard K. Butcher, PhD, RN, APRN, BC; Nursing Interventions Classification; Joanne McCloskey Dochterman, PhD, RN, FAAN; Nursing Interventions Classification; Marion Johnson, PhD, RN; Nursing Outcomes Classification; Meridean Maas PhD, RN; Nursing Outcomes Classification; Karen S. Martin, RN, NSN, FAAN; Omaha System; Sue Moorhead PhD, RN, Nursing Outcomes Classification; Christine Spisla, RN, MSN; SNOMED Terminology Solutions; Elizabeth Swanson, PhD, RN; Nursing Outcomes Classification, Sharon Giarrizzo-Wilson, RN, BSN/MS, CNOR, Association of PeriOperative Registered Nurses Citation: Lundberg, C., Warren, J.., Brokel, J., Bulechek, G., Butcher, H., McCloskey Dochterman, J., Johnson, M., Mass, M., Martin, K., Moorhead, S., Spisla, C., Swanson, E., & Giarrizzo-Wilson, S. (June, 2008). Selecting a Standardized Terminology for the Electronic Health Record that Reveals the Impact of Nursing on Patient Care. Online Journal of Nursing Informatics (OJNI), 12, (2). Available at http:ojni.org/12_2/lundberg.pdf Page 2 of 20 Abstract Using standardized terminology within electronic health records is critical for nurses to communicate their impact on patient care to the multidisciplinary team. The universal requirement for quality patient care, internal control, efficiency and cost containment, has made it imperative to express nursing knowledge in a meaningful way that can be shared across disciplines and care settings. The documentation of nursing care, using an electronic health record, demonstrates the impact of nursing care on patient care and validates the significance of nursing practice. -

Barriers to Implementation of Nursing Process Among Nurses Working in Narok County Referral Hospital
BARRIERS TO IMPLEMENTATION OF NURSING PROCESS AMONG NURSES WORKING IN NAROK COUNTY REFERRAL HOSPITAL Lekenit Saretin Anna, Dr. Agnes K. Mutinda and Prof. Ruth G. Gatere Journal of Health, Medicine and Nursing ISSN 2520-4025 (Online) Vol.5, Issue 4. No.3, pp 15- 35, 2020 www.iprjb.org BARRIERS TO IMPLEMENTATION OF NURSING PROCESS AMONG NURSES WORKING IN NAROK COUNTY REFERRAL HOSPITAL 1*Lekenit Saretin Anna (BScN) Post Graduate Student: Department of Nursing Sciences, School of Medicine & Health Sciences, Kenya Methodist University Corresponding authors’ E-Mail: [email protected] 2Dr. Agnes K. Mutinda Lecturer: Department of Nursing Sciences, School of Medicine & Health Sciences, Kenya Methodist University 3Prof. Ruth G. Gatere Lecturer: Department of Nursing Sciences, School of Medicine & Health Sciences, Kenya Methodist University Abstract Purpose of the study: This study therefore assessed barriers of nursing process implementation by Narok County Referral Hospital nurses. Methodology: A descriptive cross sectional study design was used to collect data from 102 randomly sampled nurses in NCRH. The study instruments used were self-administered questionnaires and key informant interview. SPSS version 20.0 was used to analyze quantitative data and sample characteristics were analyzed using mean and median. Themes were used to analyze qualitative data and narratively presented. Association between the study variables was calculated using chi square at 95% level of significance while statistical significance of results obtained was calculated using p values of 0.05. Data analysis was presented using tables and graphs. Approval was sought from relevant authorities. Results: The study results revealed that female participants were the majority at (70.6%). -

Introduction to Perioperative Nursing
Describe an overview of the Perioperative Nursing Practice State the purpose of AORN (Association of periOperative Registered Nurse) Standards and Recommended Practices in Perioperative Clinical Practice Describe PNDS process Identify the essential components of the Perioperative Nursing Process State the purpose of Performance improvement in Perioperative Clinical Practice Describe perioperative nursing roles in the future Requires a broad knowledge base -surgical anatomy and physiology -physiologic complications -intraoperative risk factors -potentials for injury and prevention -psychosocial implications for patient & family Microsoft Clipart The purpose of this association is: ◦ Unite registered professional operating room nurses in a constant endeavor of promoting high professional standards and recommendations for optimum care of the patient before, during and after surgery ◦ Provide opportunities for learning, by offering educational activities ◦ Study, discuss, research and provide exchange of information Purpose ◦ Hold meetings for the purposes of the association ◦ To cooperate under law with other associations, health care facilities, universities, industries, technical societies, research organizations and governmental agencies for matters affecting the association ◦ To lawfully adopt policies and procedures, conduct programs to improve perioperative practice. ◦ AORN is a non-profit organization A Registered Nurse, who utilizes the nursing process, develops a plan of care, coordinates, and delivers care to patients -

Arabella D'havé, Chief of Terminologie, Classification
Usability of SNOMED CT for secondary use of data in nursing Arabella D’Havé, Chief of Terminologie, Classification, Grouping & Audit Belgian Federal Public Service of Health, Food Chain Safety and Environment Terminology Center ABSTRACT RESULTS Objective: To create an interoperable list of SNOMED CT concepts pertinent to According to the purpose of the study, a total number of 405,131 nursing concepts nursing practice through cross-mapping of seven standardized nursing languages were extracted from UMLS. For each interface terminology of nursing, the number of recognized as interface nursing terminologies to support secondary use of data. unique concepts was extracted, 410 concepts from the Clinical Care Classification Design: The UMLS Metathesaurus was queried in order to retrieve all SNOMED CT (CCC; formerly Home Health Care Classification), 1,689 concepts from the concepts where the concept was also represented within seven standardized nursing International Classification for Nursing Practice (ICNP), 237 concepts from the NANDA- languages recognized both nationally and internationally for use as an interface International (NANDA-I; Nursing Diagnosis Classification), 11,255 from the Nursing terminology in paper-based as well as electronic health records. A candidate list of Intervention Classification (NIC), 5,707 from the Nursing Outcome Classification SNOMED CT concepts was retrieved and presented to a project team in the University (NOC), 554 from the Omaha System, 199 from the Perioperative Nursing Data Set Hospitals Leuven in order to validate the SNOMED CT concepts that are present or (PNDS), 9,065 from the ABC Coding Solutions system, and 376,015 from the Logical missing from this list to accommodate with the mandatory Minimum Nursing Dataset Observation Identifiers Names and Codes (LOINC). -

FALL/WINTER 2019 DREAMING INSIDE THIS a Natural Fit ISSUE UNC Anesthesiology Comes to Wayne UNC Health Care
Carolina UNC ANESTHESIOLOGY NEWS VOLUME 4 • ISSUE 2 FALL/WINTER 2019 DREAMING INSIDE THIS A Natural Fit ISSUE UNC Anesthesiology Comes to Wayne UNC Health Care UNC Joins Wayne Anesthesiology Numbers at a Glance Chairman's Note New Hires Leadership Recognition Residency Update Spotlight on Fellows Mauck Burn Research Photo Gallery January – June 2019 Faculty Publications, Awards & Presentations Upcoming Events MAKE A GIFT L to R: Wayne UNC Health Care anesthesiologists Drs. Al Melvin, Voltaire Misa, Jamie Cummings (top) and Peter Fischer (bottom) Support the missions of UNC Department of sk UNC faculty anesthesiologists how it’s gone since joining Wayne UNC Health Care’s anesthesia care Anesthesiology by donating team this year. Sit with Wayne’s clinical supervisor for managerial perspective on whether the hospital's med.unc.edu/ CRNAs are applying their peri-anesthesia scope of practice under new physicians. Stop by pre-op for anesthesiology/donate nursing input on the feel of team communications working alongside UNC anesthesiologists. The feedback from all Abrings one to mind spelling a positive outlook for anesthesia care delivery at Wayne as UNC faculty anesthesiologists take the helm — cohesion. For more information Onboarding five UNC anesthesiologists at Wayne by year’s end is not only welcome; it’s also timely. In September www.med.unc.edu/anesthesiology 2019, construction and renovation of a surgical pavilion project was completed adding almost 100K square feet to Wayne’s operating rooms (ORs). This massive undertaking modernized 12 ORs, four procedural rooms, one endoscopy/ERCP suite and one labor & delivery unit, among others. Overhauled surgical areas provide UNC anesthesiologists an early-stage opportunity to build workplace perioperative relationships with Wayne’s pre- and Visit us on Facebook post-op nurses, Certified Registered Nurse Anesthetists (CRNAs) and OR personnel.