The Nursing Outcomes Classification Acta Paulista De Enfermagem, Vol
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sigma Theta Tau International Honor Society of Nursing
Sigma Theta Tau International Honor Society of Nursing DELTA ZETA CHAPTER NEWS Lehman College Department of Nursing Spring 2014 DELTA ZETA CELEBRATES 34TH INDUCTION CEREMONY Chapter Officers President Theresa L. Lundy Vice-President Shirlee Cohen Secretary Dorothy Oliver-Phinn Treasurer 2014 Inductees Farley Villarente When Lehman College’s Department of Nursing geared up to create innovative Faculty Counselors programs that would tackle the growing need for baccalaureate prepared registered Dr. Eleanor Campbell nurses and advanced practice nurses, graduates from both the undergraduate and Dr. Scott Saccomano graduate nursing programs exploded. For Delta Zeta, that means welcoming many new members that are part of a very large graduating class. This year Delta Zeta welcomed Leadership Succession 76 new members into the Honor Society of Nursing and two dual members, Dr. Committee Claudette Gordon and Natasha Nurse. Sybilla Daniels-Douglas Among the inductees were five nurse leaders from Colombia South America who Alcasia Pasci joined us via Skype. Dr. Martha Whetsell introduced the nurse leaders: Dr. Gloria Maria Ateohurta, President of Universidad La Libre in Pereira, Colombia. She is the Membership Chair & first nurse of South America to be a President of a University. Dr. Mercy Soto is Dean Heritage Committee and Professor of Nursing at Universidad La Libre. Her research is in cardiovascular Harriet Parness problems and Hope. Dr. Maria Elena Lopez is Director of Graduate Nursing Programs at Universidad La Libre. Dr. Lopez’ research is in obesity in children. Dr. Lili Andrea Newsletter Editor Buitrago is the Director of Nursing Undergraduate Programs at Universidad La Libre Theresa L. Lundy and her research is in Obesity in Women. -
Online Induction System Manual
Online Induction System Manual Page | 1 All chapters of the Honor Society of Nursing, Sigma Theta Tau International (STTI) use the Online Induction System to create a new induction, upload and invite candidates, and pull reports related to your induction. Use the contents of this manual to utilize the system successfully. If you have additional questions, email [email protected], or telephone 888.634.7575 (U.S./Canada toll-free) or +1.317.634.8171 (International). Table of Contents Creating a New Induction Edit Contact Information Edit Ceremony Edit Ceremony Fees Induction Summary Page Uploading Candidates to an Induction Download a Template Upload the Template Managing Errors Adding a Single Candidate Editing a Candidate’s Information Sending Messages to Candidates Schedule the Invitation Schedule Reminders Pulling Reports Types of Reports Accessing Previous Inductions Page | 2 Creating a New Induction In this system, you will be able to create an induction any time you want to invite candidates. According to the bylaws, your chapter must invite and induct eligible members a minimum of one time per year. You can choose to have an induction ceremony, a virtual ceremony, or no ceremony with each induction. You can also separate inductions by campus. This will allow you to invite and induct members in the way that is most convenient for them! There are a few questions you should be able to answer before creating a new induction, so you have all the necessary information to complete each step: Who will serve as the induction contact? This person should be comfortable answering questions from candidates. -

Rhonda M. Board, Phd, RN, CCRN-K Curriculum Vitae
Rhonda M. Board, PhD, RN, CCRN-K Curriculum Vitae Northeastern University phone: (617) 373-5248 408 Robinson Hall email: [email protected] Boston, MA 02115 FORMAL EDUCATION 1999 Ph.D., The Ohio State University, Columbus Major: Nursing, Cognate: Human Development & Family Science 1994 M.S., The Ohio State University Major: Pediatric Nursing 1988 B.S., State University of New York, Binghamton Major: Nursing 1985 Diploma, Crouse-Irving Memorial Hospital, School of Nursing, Syracuse, New York LICENSURE 1999 Registered Nurse, Massachusetts 1986 Registered Nurse, New York (inactive) CERTIFICATION 1992-present C.C.R.N./C.C.R.N.-K. (Critical-Care) in Pediatrics, American Association of Critical- Care Nurses (AACN) 2007 End-of-Life Nursing Education Consortium (ELNEC) Critical Care Program Trainer EMPLOYMENT HISTORY Academic Appointments 2019-present PhD Program Director, Northeastern University School of Nursing, Boston, Massachusetts 2005-present Associate Professor (with tenure), Northeastern University School of Nursing, 2018-2019 Interim Dean, Northeastern University School of Nursing 2011-2012 Interim Associate Dean for Undergraduate Education, Northeastern University Bouvé College of Health Sciences 1999-2005 Assistant Professor, Northeastern University School of Nursing 1994-1995 Graduate Research Associate, The Ohio State University College of Nursing, Columbus 1994-1996 Clinical Faculty, Capital University School of Nursing Columbus, Ohio 1995-1997; Graduate Teaching Associate, The Ohio State University College of Nursing 1992-1994 -

The Lived Experience of Faith Community Nurses Living the Call to Health Ministry
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2010 The Lived Experience of Faith Community Nurses Living the Call to Health Ministry Deborah Mobley Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Nursing Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/101 This Dissertation is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. © Deborah Darlene Simpson Mobley 2009 All Rights Reserved i THE LIVED EXPERIENCE OF FAITH COMMUNITY NURSES LIVING THE CALL TO HEALTH MINISTRY A Dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy at Virginia Commonwealth University. by DEBORAH DARLENE SIMPSON MOBLEY Master of Nursing Science (Nursing Administration), Virginia Commonwealth University, 1994 Bachelor of Science (Nursing), Virginia Commonwealth University, 1989 Director: Inez Tuck, Ph.D., R.N., M.B.A., MDiv. Professor, Department of Adult Health and Nursing Systems Virginia Commonwealth University Richmond, Virginia December 2009 ii Dedication To my husband Jerry, who promised more than 33 years ago to love me for better and for worse, and who continues to love me through everything. I am so very blessed to have him as my spouse. To my family, my sister, Gina, and my nephews, Matthew and Robert. May you be blessed for all of your love and support. I pray that I give each of you the gifts you have given me as you continue on your journey. -

Adult Nursing Interested in Nursing at BU……
Download our free Open Day app #BUopenday #Belongatbu #HSSatBU Department of Nursing Science BSc (Hons) Adult Nursing Interested in Nursing at BU……. • What nursing is • Skills & qualities • Why BU? • Application Mentimeter code: What is Nursing…….? Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups and communities, sick or well and in all settings. Nursing includes the promotion of health, prevention of illness, and the care of ill, disabled and dying people. Advocacy, promotion of a safe environment, research, participation in shaping health policy and in patient and health systems management, and education are also key nursing roles. (ICN, 2002) Promote What do Adult Health of Adult Nurses Do? Population Care for & Support Adults Develop and Physical Needs Lead Care Social Needs Psychological Needs Packages Spiritual Needs Adult Nurses Direct care Working as part of Evidence Based Interprofessional Teams Ensure Manage ill Effective health & Delivery of Disease care Individuality/ expectations NHS Values Diversity of settings Nurses respond to Healthcare Evolving role provision Legislation Key Skills and Qualities Caring Empathetic Resourceful Critical thinker Team worker Empower Subject Knowledge Excellent communicator Independent learner Help other make lifestyle changes Respect the right of others Nurses work in…… • Nursing Homes • People’s homes • Health Centres • Community • Workplaces • Schools • Prisons • Hospitals • GP surgeries • Independent • Private sector • Overseas • -

A Nursing Student’S Perspective on Caring in Tanzania
alphasigma theta tau international chi honor societynews of nursing BOSTON WILLIAM F. CONNELL Winter 2015 COLLEGE SCHOOL OF NURSING ders Lea hip S y c t h i 45th Anniversary o n l u a r m of s Alpha Chi Chapter h m i p o C officers Alpha Chi Chapter, Boston College Sigma Theta Tau International Officers & Committees 2014–2015 Administrative Assistant Catherine Hill [email protected] Web Master Angela Bowser [email protected] President Kelly Stamp [email protected] Vice-President Louisa Dichard [email protected] Secretary Barbara MacIntrye [email protected] Treasurer Diana Kach [email protected] Faculty Counselor Colleen Simonelli [email protected] Governance Committee Colleen Simonelli, Chair [email protected] Rosemary Byrne [email protected] Louisa Dichard [email protected] Maureen Connolly [email protected] Student Representative Leadership Succession Maureen Connolly, Chair [email protected] Helen Williams [email protected] Program Committee Louisa Dichard, Chair [email protected] Diana Kach [email protected] Barbara MacIntrye [email protected] Publicity /Newsletter Chair & Committee Luanne Nugent, Co-Chair [email protected] Jacqueline Sly, Co-Chair [email protected] Student Representative Colleen McGauley Yvonne Shih alpha chi news • 2015 2 officers Awards & Scholarships Committee Margie Sipe, Chair [email protected] Carina Katigbak [email protected] Research Development Committee Viola Benavente, Chair [email protected] Stewart Bond [email protected] Joyce Edmonds -
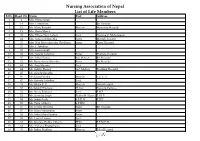
Nursing Association of Nepal List of Life Members S.No
Nursing Association of Nepal List of Life Members S.No. Regd. No. Name Post Address 1 2 Mrs. Prema Singh 2 14 Mrs. I. Mathema Bir Hospital 3 15 Ms. Manu Bangdel Matron Maternity Hospital 4 19 Mrs. Geeta Murch 5 20 Mrs. Dhana Nani Lohani Lect. Nursing C. Maharajgunj 6 24 Mrs. Saraswati Shrestha Sister Mental Hospital 7 25 Mrs. Nati Maya Shrestha (Pradhan) Sister Kanti Hospital 8 26 Mrs. I. Tuladhar 9 32 Mrs. Laxmi Singh 10 33 Mrs. Sarada Tuladhar Sister Pokhara Hospital 11 37 Mrs. Mita Thakur Ad. Matron Bir Hospital 12 42 Ms. Rameshwori Shrestha Sister Bir Hospital 13 43 Ms. Anju Sharma Lect. 14 44 Ms. Sabitry Basnet Ast. Matron Teaching Hospital 15 45 Ms. Sarada Shrestha 16 46 Ms. Geeta Pandey Matron T.U.T. H 17 47 Ms. Kamala Tuladhar Lect. 18 49 Ms. Bijaya K. C. Matron Teku Hospital 19 50 Ms.Sabitry Bhattarai D. Inst Nursing Campus 20 52 Ms. Neeta Pokharel Lect. F.H.P. 21 53 Ms. Sarmista Singh Publin H. Nurse F. H. P. 22 54 Ms. Sabitri Joshi S.P.H.N F.H.P. 23 55 Ms. Tuka Chhetry S.P.HN 24 56 Ms. Urmila Shrestha Sister Bir Hospital 25 57 Ms. Maya Manandhar Sister 26 58 Ms. Indra Maya Pandey Sister 27 62 Ms. Laxmi Thakur Lect. 28 63 Ms. Krishna Prabha Chhetri PHN F.P.M.C.H. 29 64 Ms. Archana Bhattacharya Lect. 30 65 Ms. Indira Pradhan Matron Teku Hospital S.No. Regd. No. Name Post Address 31 67 Ms. -

Lawrlwytho'r Atodiad Gwreiddiol
Operational services structure April 2021 14/04/2021 Operational Leadership Structures Director of Operations Director of Nursing & Quality Medical Director Lee McMenamy Joanne Hiley Dr Tessa Myatt Medical Operations Operations Clinical Director of Operations Deputy Director of Nursing & Deputy Medical Director Hazel Hendriksen Governance Dr Jose Mathew Assistant Clinical Director Assistant Director of Assistant Clinical DWiraerctringor ton & Halton Operations Corporate Corporate Lorna Pink Assistant Assistant Director Julie Chadwick Vacant Clinical Director of Nursing, AHP & Associate Clinical Director Governance & Professional Warrington & Halton Compliance Standards Assistant Director of Operations Assistant Clinical Director Dr Aravind Komuravelli Halton & Warrington Knowsley Lee Bloomfield Claire Hammill Clare Dooley Berni Fay-Dunkley Assistant Director of Operations Knowsley Associate Medical Director Nicky Over Assistant Clinical Director Allied Health Knowsley Assistant Director of Sefton Professional Dr Ashish Kumar AssiOstapenrta Dtiironesc tKnor oofw Oslpeeyr ations Sara Harrison Lead Nicola Over Sefton James Hester Anne Tattersall Assistant Clinical Director Associate Clinical Director Assistant Director of St Helens & Knowsley Inpatients St Helens Operations Sefton Debbie Tubey Dr Raj Madgula AssistanAt nDniree Tcatttore ofrs aOllp erations Head of St Helens & Knowsley Inpatients Safeguarding Tim McPhee Assistant Clinical Director Sarah Shaw Assistant Director of Associate Medical Director Operations St Helens Mental Health -

THE DEVELOPMENT of NURSING EDUCATION in the ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I
THE DEVELOPMENT OF NURSING EDUCATION IN THE ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I. GARDNER, B.S.N., M.S.N., M.Ed. A DISSERTATION IN HIGHER EDUCATION Submitted to the Graduate Faculty of Texas Tech University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF EDUCATION Approved Accepted Dean of the Graduate School August, 1993 ft 6 l^yrr^7^7 801 J ,... /;. -^o ACKNOWLEDGEMENTS C?^ /c-j/^/ C^ ;^o.^^ I would like to thank Dr. Clyde Kelsey, Jr., for his C'lp '^ ^unflagging support, his advice and his constant vigil and encouragement in the writing of this dissertation. I would also like to thank Dr. Patricia Yoder-Wise who acted as co-chairperson of my committee. Her advice was invaluable. Drs. Mezack, Willingham, and Ewalt deserve much praise for the many times they critically read the manuscript and gave their input. I would also like to thank Ms. Janey Parris, Senior Program Officer of Health, Guyana, the government officials of the Caribbean Embassies, representatives from the Caribbean Nursing Organizations, educators from the various nursing schools and librarians from the archival institutions and libraries in Trinidad and Tobago and Jamaica. These individuals agreed to face-to-face interviews, answered telephone questions and mailed or faxed information on a regular basis. Much thanks goes to Victor Williams for his computer assistance and to Hannelore Nave for her patience in typing the many versions of this manuscript. On a personal level I would like to thank my niece Eloise Walters for researching information in the nursing libraries in London, England and my husband Clifford for his belief that I could accomplish this task. -

The CDC Guide to Strategies to Support Breastfeeding Mothers And
Contents Using Tis Guide ............................................................................................................................ 1 Introduction ................................................................................................................................... 3 Strategy 1. Maternity care practices ................................................................................................. 5 Strategy 2. Professional education .................................................................................................. 11 Strategy 3. Access to professional support ...................................................................................... 15 Strategy 4. Peer support programs ................................................................................................. 19 Strategy 5. Support for breastfeeding in the workplace .................................................................. 23 Strategy 6. Support for breastfeeding in early care and education................................................... 29 Strategy 7. Access to breastfeeding education and information ...................................................... 33 Strategy 8. Social marketing .......................................................................................................... 37 Strategy 9. Addressing the marketing of infant formula ................................................................. 43 References .................................................................................................................................... -

Sylvia Haslett
Sylvia Miller 2345 E San Ramon Ave, Fresno, CA 93740 (559) 278-2041 California R.N. License RN 219661 California N.P. Furnishing Number 95000917 _________________________________________________________________ EDUCATION Fresno State College August 1967 to September 1971 Fresno, California Bachelor of Science, Nursing California State University August 1973 to June 1976 Fresno, California Masters of Science, Nursing Medical Surgical Nursing North Dakota State University Fargo, North Dakota Methods of Research in Education -Winter Qtr. 1980 Statistics in Education -Spring Qtr. 1981 Louisiana State University Baton Rouge, Louisiana Utilization of Television in Education -Fall, 1983 Utilization of Media in Education -Fall, 1983 Production of Educational Media -Spring, 1984 California State University May 1987 to December 1990 Fresno, California Master of Art, Education University of San Francisco August 1992 to May 1998 San Francisco, California School of Education, Curriculum and Instruction Doctorate of Education California State University January 2013 to May 2014 Fresno, California Post Masters Certificate, Family Nurse Practitioner CERTIFICATION AANP Family Nurse Practitioner Certificaion # F0914420 9/10/2014 to 9/9/2019 ADDITIONAL EDUCATIONAL QUALIFICATIONS 1 Pain Resource Nurse Training Course September 2012 End of Life Nursing Education Consortium Geriatrics Trainer January 2011 Harvard Medical School Center for Palliative Care, Faculty Scholar Program in Palliative Care Education & Practice November 2007 End of Life Nursing Education -

STTI Scholarship Defined
STTI Scholarship Defined The mission of the Honor Society of Nursing, Sigma Theta Tau International (STTI), is advancing world health and celebrating nursing excellence in scholarship, leadership, and service. Nurses in all settings develop and use scientific evidence to advance health. Sigma Theta Tau International has promoted the development of and shared definitions and resources related to clinical scholarship (Dreher, 1999) and the scholarship of reflective practice (Freshwater, Horton-Deutsch, Sherwood & Taylor, 2005). Over the past decade, understanding of the nature of scholarship has expanded to embrace implementation and translation sciences, the harnessing of large sets of clinical data to provide evidence for practice increasingly in real time, the potential of social media to provide leading indicators of population health status, and additional focus on health outcomes related to health care policy. For that reason, STTI is building on the work of Dreher and of Freshwater et al. to provide an expanded understanding of scholarship to inform not only the development of, but also the translation of scientific evidence in all aspects of nursing practice. Clinical scholarship is described by Dreher (1999) as an intellectual endeavor that entails systematic inquiry and scrutiny of practice in an effort to continually improve nursing practice. Clinical scholarship is informed by and inspires research. It enhances the development of nursing knowledge by testing clinical realities against theories in varied settings with diverse populations. Dreher describes clinical scholarship as entailing observation, analysis, synthesis, application, and dissemination. She also describes clinical scholarship as being characterized by the fact that it is value-driven, autonomous, and creative.