Fibroadenoma of Bilateral Axillary Ectopic Breast Tissue: a Rare Case Report Based on Orem’S Self Care Theory
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

How Do Nurses Feel About Their Cultural Competence? a Literature Review
How do nurses feel about their cultural competence? A Literature Review Fidele Sindayigaya Bachelor’s thesis November 2016 Degree Programme in Nursing Social services, Health & Sport Author(s) Type of publication: Date: November 2016 Bachelor’s thesis Fidele SINGAYIGAYA Language of Publication: English Number of pages Permission for web 40 publication: x Title of Publication: How do nurses feel about their cultural competence? Degree Programme in Nursing, Bachelor of Health Care Tutors: Marjo Palovaara & Garbrah William Assigned by Abstract The aim of this study was to explore and analyse through literature review, the cultural competence of Nurse. The purpose of this study was to provide information to both nursing students and nurses on how to enhance their cultural competence, and answering the future needs of social and health care services, in a multicultural environment. The method used in conducting this research is the review of literature; data for the research was acquired from electronic databases such as CINAHL and PubMed. Moreover the research filters used consist of free link full text, publication year 2000-2016, English language and reference available. The data that emerged from the studies indicated that most of the nurses reported the feelings of apprehension, loneliness, and lacks of confidence during their cultural competence. Furthermore, the studies found that nurses need to recognize their own cultural values in seeking cultural competence; the nurses perceived the fear of mistakes and crossing boundaries related to the cultural and religious practices of minority patients as particularly stressful. Keywords/tags (subjects) culture, cultural competence, transcultural nursing, and health communication Miscellaneous Table of contents 1. -
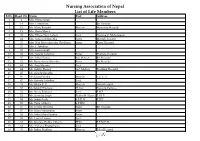
Nursing Association of Nepal List of Life Members S.No
Nursing Association of Nepal List of Life Members S.No. Regd. No. Name Post Address 1 2 Mrs. Prema Singh 2 14 Mrs. I. Mathema Bir Hospital 3 15 Ms. Manu Bangdel Matron Maternity Hospital 4 19 Mrs. Geeta Murch 5 20 Mrs. Dhana Nani Lohani Lect. Nursing C. Maharajgunj 6 24 Mrs. Saraswati Shrestha Sister Mental Hospital 7 25 Mrs. Nati Maya Shrestha (Pradhan) Sister Kanti Hospital 8 26 Mrs. I. Tuladhar 9 32 Mrs. Laxmi Singh 10 33 Mrs. Sarada Tuladhar Sister Pokhara Hospital 11 37 Mrs. Mita Thakur Ad. Matron Bir Hospital 12 42 Ms. Rameshwori Shrestha Sister Bir Hospital 13 43 Ms. Anju Sharma Lect. 14 44 Ms. Sabitry Basnet Ast. Matron Teaching Hospital 15 45 Ms. Sarada Shrestha 16 46 Ms. Geeta Pandey Matron T.U.T. H 17 47 Ms. Kamala Tuladhar Lect. 18 49 Ms. Bijaya K. C. Matron Teku Hospital 19 50 Ms.Sabitry Bhattarai D. Inst Nursing Campus 20 52 Ms. Neeta Pokharel Lect. F.H.P. 21 53 Ms. Sarmista Singh Publin H. Nurse F. H. P. 22 54 Ms. Sabitri Joshi S.P.H.N F.H.P. 23 55 Ms. Tuka Chhetry S.P.HN 24 56 Ms. Urmila Shrestha Sister Bir Hospital 25 57 Ms. Maya Manandhar Sister 26 58 Ms. Indra Maya Pandey Sister 27 62 Ms. Laxmi Thakur Lect. 28 63 Ms. Krishna Prabha Chhetri PHN F.P.M.C.H. 29 64 Ms. Archana Bhattacharya Lect. 30 65 Ms. Indira Pradhan Matron Teku Hospital S.No. Regd. No. Name Post Address 31 67 Ms. -

Lawrlwytho'r Atodiad Gwreiddiol
Operational services structure April 2021 14/04/2021 Operational Leadership Structures Director of Operations Director of Nursing & Quality Medical Director Lee McMenamy Joanne Hiley Dr Tessa Myatt Medical Operations Operations Clinical Director of Operations Deputy Director of Nursing & Deputy Medical Director Hazel Hendriksen Governance Dr Jose Mathew Assistant Clinical Director Assistant Director of Assistant Clinical DWiraerctringor ton & Halton Operations Corporate Corporate Lorna Pink Assistant Assistant Director Julie Chadwick Vacant Clinical Director of Nursing, AHP & Associate Clinical Director Governance & Professional Warrington & Halton Compliance Standards Assistant Director of Operations Assistant Clinical Director Dr Aravind Komuravelli Halton & Warrington Knowsley Lee Bloomfield Claire Hammill Clare Dooley Berni Fay-Dunkley Assistant Director of Operations Knowsley Associate Medical Director Nicky Over Assistant Clinical Director Allied Health Knowsley Assistant Director of Sefton Professional Dr Ashish Kumar AssiOstapenrta Dtiironesc tKnor oofw Oslpeeyr ations Sara Harrison Lead Nicola Over Sefton James Hester Anne Tattersall Assistant Clinical Director Associate Clinical Director Assistant Director of St Helens & Knowsley Inpatients St Helens Operations Sefton Debbie Tubey Dr Raj Madgula AssistanAt nDniree Tcatttore ofrs aOllp erations Head of St Helens & Knowsley Inpatients Safeguarding Tim McPhee Assistant Clinical Director Sarah Shaw Assistant Director of Associate Medical Director Operations St Helens Mental Health -

INCREASING BREASTFEEDING SUPPORT 1 INCREASING BREAST FEEDING SUPPORT AMONG NEONATAL NURSES by Lawanda Bailey-Guess GEORGANN
INCREASING BREASTFEEDING SUPPORT 1 INCREASING BREAST FEEDING SUPPORT AMONG NEONATAL NURSES By Lawanda Bailey-Guess GEORGANN WEISSMAN, DNP, GNP-BC, CNE, Faculty Mentor and Chair TERRI JONES, DNP, Committee Member KIMBERLY NERUD, PHD, Committee Member REGINA DENNIS, MSN, MBA Patrick Robinson, PhD, Dean, School of Nursing and Health Sciences A DNP Project Presented in Partial Fulfillment Of the Requirements for the Degree of Doctor of Nursing Practice Capella University November 2018 INCREASING BREASTFEEDING SUPPORT 2 Abstract The importance of breastfeeding support remains a global phenomenon, as breastfeeding remains the algorithm of healthcare promotion throughout the life span. The purpose of this project reviews benefits of improving breastfeeding, and breast milk production, among lactating women and their infants by increasing knowledge, skills and positive breastfeeding attitudes among Neonatal Intensive Care Unit (NICU) nurses. The project health care facility has approximately 30% of its neonatal infants who receive breast milk within four weeks of life (Project Facility, 2017) compared to the Center for Disease Control (CDC) recommendation of 75% for early breastfeeding initiation (CDC, 2017). The project‟s quality improvement program provided a descriptive quantitative design in which questionnaires were distributed among neonatal nurses and breastfeeding mothers to query access and implement the CDC guidelines, Baby Friendly benchmarks, and Healthy People 2020 goals. The Breastfeeding Support Program was implemented as a 3 day breastfeeding support class, implementation of hands-on policy, and a quality improvement tool. The key findings of this project study demonstrated evidence that neonatal nurses were not given consistent interactive breastfeeding in-service. As such, neonatal nurses should be given a „hands on‟ breastfeeding support class and policy review annually per CDC recommendations. -

THE DEVELOPMENT of NURSING EDUCATION in the ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I
THE DEVELOPMENT OF NURSING EDUCATION IN THE ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I. GARDNER, B.S.N., M.S.N., M.Ed. A DISSERTATION IN HIGHER EDUCATION Submitted to the Graduate Faculty of Texas Tech University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF EDUCATION Approved Accepted Dean of the Graduate School August, 1993 ft 6 l^yrr^7^7 801 J ,... /;. -^o ACKNOWLEDGEMENTS C?^ /c-j/^/ C^ ;^o.^^ I would like to thank Dr. Clyde Kelsey, Jr., for his C'lp '^ ^unflagging support, his advice and his constant vigil and encouragement in the writing of this dissertation. I would also like to thank Dr. Patricia Yoder-Wise who acted as co-chairperson of my committee. Her advice was invaluable. Drs. Mezack, Willingham, and Ewalt deserve much praise for the many times they critically read the manuscript and gave their input. I would also like to thank Ms. Janey Parris, Senior Program Officer of Health, Guyana, the government officials of the Caribbean Embassies, representatives from the Caribbean Nursing Organizations, educators from the various nursing schools and librarians from the archival institutions and libraries in Trinidad and Tobago and Jamaica. These individuals agreed to face-to-face interviews, answered telephone questions and mailed or faxed information on a regular basis. Much thanks goes to Victor Williams for his computer assistance and to Hannelore Nave for her patience in typing the many versions of this manuscript. On a personal level I would like to thank my niece Eloise Walters for researching information in the nursing libraries in London, England and my husband Clifford for his belief that I could accomplish this task. -

The CDC Guide to Strategies to Support Breastfeeding Mothers And
Contents Using Tis Guide ............................................................................................................................ 1 Introduction ................................................................................................................................... 3 Strategy 1. Maternity care practices ................................................................................................. 5 Strategy 2. Professional education .................................................................................................. 11 Strategy 3. Access to professional support ...................................................................................... 15 Strategy 4. Peer support programs ................................................................................................. 19 Strategy 5. Support for breastfeeding in the workplace .................................................................. 23 Strategy 6. Support for breastfeeding in early care and education................................................... 29 Strategy 7. Access to breastfeeding education and information ...................................................... 33 Strategy 8. Social marketing .......................................................................................................... 37 Strategy 9. Addressing the marketing of infant formula ................................................................. 43 References .................................................................................................................................... -

Nursing Leadership and Client Care Management
West Virginia Wesleyan College BSN Preceptor Orientation Manual For NURS 420: Leadership in Healthcare 2015-16 2 Welcome to NURS 420, Leadership in Healthcare! This preceptor orientation manual has been designed for students, faculty, and preceptors to assist students to have a successful clinical experience. The Philosophy of the West Virginia Wesleyan College endeavors to graduate men and women, who think critically and creatively, communicate effectively, act responsibly and demonstrate their local and world citizenship through service. We appreciate the registered nurses who agree to function as preceptors and role models for our students. It is out intent to make this journey personally and professionally growth producing for students and preceptors, and an enjoyable learning experience for all. Please take the time to carefully review this manual. If you have questions or suggestions, please don’t hesitate to contact the Wesleyan College Department of Nursing office, 304-473-8224. West Virginia Wesleyan College Susan P. Rice PhD, MPH, RN/NM Creator of Preceptor Manual Barbara Frye MSN, RN Faculty Revised December 2015 3 Table of Contents PART I: Course Information Introduction to the course………………………………………………………………………. 4 NURS 420 Clinical Objectives………………………………………………………………….. 4 SON Mission & Goals…………………………………………….…………………………………..5 Student Learning Outcomes.…………………………………………………………………….6 Preceptor-Guided clinical: Overview…………………………………….………………….8 West Virginia Board of Registered Nursing: Regulations………………………..8 Roles and Responsibilities of Preceptors, Students, Faculty…………………..9 PART II: Useful Information and Reference Phases of Preceptor-Student Working Relationship……………………………….13 Adult Learner-Centered Teaching Strategies………………………………………….14 “Reality Shock”…………………………………………………………………………………………16 Weekly Guidelines for Student Activity…………………………………………………..17 Some Tips from Expert Preceptors………………………………………………………….18 References…………………………………………………………………………………….………….19 APPENDECES Appendix A; Preceptor Resume………………………………………………………………………. -

The Case of Modern Matrons in the English NHS
The dynamics of professions and development of new roles in public services organizations: The case of modern matrons in the English NHS Abstract This study contributes to research examining how professional autonomy and hierarchy impacts upon the implementation of policy designed to improve the quality of public services delivery through the introduction of new managerial roles. It is based on an empirical examination of a new role for nurses - modern matrons - who are expected by policy makers to drive organizational change aimed at tackling health care acquired infections [HCAI] in the National Health Service [NHS] within England. First, we show that the changing role of nurses associated with their ongoing professionalisation limit modern matron‟s influence over their own ranks in tackling HCAI. Second, modern matrons influence over doctors is limited. Third, government policy itself appears inconsistent in its support for the role of modern matrons. Modern matrons‟ attempts to tackle HCAI appear more effective where infection control activity is situated in professional practice and where modern matrons integrate aspirations for improved infection control within mainstream audit mechanisms in a health care organization. Key words: professions, NHS, modern matrons, health care acquired infections Introduction The organization and management of professional work remains a significant area of analysis (Ackroyd, 1996; Freidson, 2001; Murphy, 1990; Reed, 1996). It is argued that professional autonomy and hierarchy conflict with bureaucratic and managerial methods of organizing work, especially attempts at supervision (Broadbent and Laughlin, 2002; Freidson, 2001; Larson, 1979). Consequently, the extension of managerial prerogatives and organizational controls are seen to challenge the autonomy, legitimacy and power of professional groups (Clarke and Newman, 1997; Exworthy and Halford, 1999). -

Fiscal Year 2011 Air Force Medical Programs March 10, 2010
United States Air Force Testimony Before the Senate Appropriations Subcommittee on Defense Medical Programs Statement of Major General Kimberly A. Siniscalchi, Assistant Air Force Surgeon General, Nursing Services March 10, 2010 Not for publication until released by the Senate Appropriations Subcommittee on Defense Fiscal Year 2011 Air Force Medical Programs March 10, 2010 UNITED STATES AIR FORCE MAJOR GENERAL KIMBERLY A. SINISCALCHI Maj Gen Kimberly A. Siniscalchi is Assistant Air Force Surgeon General, Medical Force Development, and Assistant Air Force Surgeon General, Nursing Services, Office of the Surgeon General, Headquarters U.S. Air Force, Arlington, VA. As Assistant Air Force Surgeon General, Medical Force Development, she establishes new and appraises existing personnel policy and staffing requirements for 34,000 active duty officer and enlisted medical personnel. Her directorate is responsible for all medical force education and training. As Assistant Air Force Surgeon General, Nursing Services, she creates and evaluates nursing policies and programs for 19,000 active-duty, Guard and Reserve nursing personnel. She interacts with Air Staff, Joint Staff, other services and major commands to ensure the highest caliber of nursing care and personnel. General Siniscalchi received her commission in 1979 through the Reserve Officer Training Corps program at the University of Pittsburgh, PA. Her leadership experience includes commanding eight consecutive years at squadron and group levels, and serving Presidents George H. W. Bush and -

Aberdeen Areawide Breastfeeding Policy
Aberdeen Area Wide Breastfeeding Policy Date: 9/12/2012 Author: Clifton Kenon Jr., DNP, MSN, RNC, IBCLC, RLC Background This facility believes that breastfeeding is the healthiest way for a woman to feed her baby and recognizes the important health benefits that exist for both the mother and her child. All families have the right to receive clear and impartial information to enable them to make a fully informed choice as to how they feed and care for their babies. Health-care staff will not discriminate against any woman in her chosen method of infant feeding and will fully support her in whatever choice she makes. Goals of this Policy To ensure that the health benefits of breastfeeding and the potential health risks of formula feeding are discussed with all women and their families so that informed choices may be made in regards to infant nutrition. To enable maternal/child staff to create an environment where breastfeeding is promoted, protected and assisted in hopes of creating an environment and culture where women are given reliable, evidence-based, and consistent information to support them to breastfeed exclusively for six months, and to continue to breastfeed with complementary other foods past then. In support of this policy It is mandatory that all staff adhere to this policy to avoid conflicting advice. Any deviation from the policy must be justified and recorded in the mother's and/or baby's health-care records. The policy should be implemented in conjunction with existing maternal and infant care policies. It is the responsibility of all health-care professionals to consult with the baby’s medical provider (medical doctor, advanced practice nurse, doctor of osteopathy etc.) should concerns arise about the baby's health. -

Arabella D'havé, Chief of Terminologie, Classification
Usability of SNOMED CT for secondary use of data in nursing Arabella D’Havé, Chief of Terminologie, Classification, Grouping & Audit Belgian Federal Public Service of Health, Food Chain Safety and Environment Terminology Center ABSTRACT RESULTS Objective: To create an interoperable list of SNOMED CT concepts pertinent to According to the purpose of the study, a total number of 405,131 nursing concepts nursing practice through cross-mapping of seven standardized nursing languages were extracted from UMLS. For each interface terminology of nursing, the number of recognized as interface nursing terminologies to support secondary use of data. unique concepts was extracted, 410 concepts from the Clinical Care Classification Design: The UMLS Metathesaurus was queried in order to retrieve all SNOMED CT (CCC; formerly Home Health Care Classification), 1,689 concepts from the concepts where the concept was also represented within seven standardized nursing International Classification for Nursing Practice (ICNP), 237 concepts from the NANDA- languages recognized both nationally and internationally for use as an interface International (NANDA-I; Nursing Diagnosis Classification), 11,255 from the Nursing terminology in paper-based as well as electronic health records. A candidate list of Intervention Classification (NIC), 5,707 from the Nursing Outcome Classification SNOMED CT concepts was retrieved and presented to a project team in the University (NOC), 554 from the Omaha System, 199 from the Perioperative Nursing Data Set Hospitals Leuven in order to validate the SNOMED CT concepts that are present or (PNDS), 9,065 from the ABC Coding Solutions system, and 376,015 from the Logical missing from this list to accommodate with the mandatory Minimum Nursing Dataset Observation Identifiers Names and Codes (LOINC). -

Nursing Management of the Patient with Multiple Sclerosis
Nursing Management of the Patient with Multiple Sclerosis AANN, ARN, and IOMSN Clinical Practice Guideline Series This publication was made possible by an educational grant from TEVA Neuroscience. Editors American Association Hilaire J. Thompson, PhD RN CNRN FAAN of Neuroscience Nurses Kristen L. Mauk, PhD DNP RN CRRN GCNS-B, GNP-BC 4700 W. Lake Avenue FAAN Glenview, IL 60025-1485 Chairs 888.557.2266, Fax 847.375.6430 Amy Perrin Ross, MSN APN MSCN CNRN International phone 847.375.4733 Suzanne C. Smeltzer, EdD RN MSCN FAAN [email protected] • www.AANN.org Joan Kram, MBA RN FACHE Content Authors Executive Director Megan Barrett, DNP MSCN ARNP June M. Pinyo, MA Cheryl Blaschuk, MSN RN MSCN FNP Managing Editor Kathleen Costello, MS ANP-BC MSCN Constance Easterling, MSN MSCN ARNP Sonya L. Jones Ann Gutierrez, MSN RN CRRN CBIS Senior Graphic Designer June Halper, MSN APN-C MSCN FAAN Paule Joseph, MSN FNP-BC RN CRRN BCLNC-C Association of Rehabilitation Nurses Patricia Kennedy, RN CNP MSCN 4700 W. Lake Avenue Mary Kitten, MSN RN MSCN CRRN Glenview, IL 60025-1485 Martha Lightfoot, ANP 800.229.7530 Elizabeth McAndrews, MSN CRNP [email protected] • www.rehabnurse.org Margie O’Leary, MSN RN MSCN Brant J. Oliver, MSN MPH FNP-BC PMHNP-BC Karen Nason, CAE Patricia Pagnotta, MSN ARNP MSCN CNRN Executive Director Dorothea Cassidy Pfohl, BSN MSCN RN Yaritza Rosario, APN MSCN International Organization of Angela Stone Schmidt, PhD MNSc RNP RN Multiple Sclerosis Nurses Matthew Sorenson, PhD RN 359 Main Street, Suite A Alpa Uchil, MPH RN Hackensack, NJ 07601 201.487.1050, Fax 201.678.2291 Content Reviewers www.iomsn.org Lisa Duffy, PhD(c) CPNP-PC CNRN Debra A.