Oral Lactulose Vs. Polyethylene Glycol for Bowel Preparation in Colonoscopy: a Randomized Controlled Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Laxatives for the Management of Constipation in People Receiving Palliative Care (Review)
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by UCL Discovery Laxatives for the management of constipation in people receiving palliative care (Review) Candy B, Jones L, Larkin PJ, Vickerstaff V, Tookman A, Stone P This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2015, Issue 5 http://www.thecochranelibrary.com Laxatives for the management of constipation in people receiving palliative care (Review) Copyright © 2015 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 BACKGROUND .................................... 2 OBJECTIVES ..................................... 4 METHODS ...................................... 4 RESULTS....................................... 7 Figure1. ..................................... 8 Figure2. ..................................... 9 Figure3. ..................................... 10 DISCUSSION ..................................... 13 AUTHORS’CONCLUSIONS . 14 ACKNOWLEDGEMENTS . 14 REFERENCES ..................................... 15 CHARACTERISTICSOFSTUDIES . 17 DATAANDANALYSES. 26 ADDITIONALTABLES. 26 APPENDICES ..................................... 28 WHAT’SNEW..................................... 35 HISTORY....................................... 35 CONTRIBUTIONSOFAUTHORS . 36 DECLARATIONSOFINTEREST . 36 SOURCESOFSUPPORT . 36 DIFFERENCES -

3.2.2 Misuse of Stimulant Laxatives
Medicines Adverse Reactions Committee Meeting date 10/06/2021 Agenda item 3.2.2 Title Misuse of stimulant laxatives Submitted by Medsafe Pharmacovigilance Paper type For advice Team Active ingredient Product name Sponsor Bisacodyl Bisacodyl Laxative (Pharmacy Health) PSM Healthcare Limited trading as API tablet Consumer Brands Dulcolax tablet Sanofi-Aventis New Zealand Limited Dulcolax Suppository Sanofi-Aventis New Zealand Limited *Lax-Suppositories Bisacodyl AFT Pharmaceuticals Limited *Lax-Tab tablet AFT Pharmaceuticals Limited Docusate sodium *Coloxyl tablet Pharmacy Retailing (New Zealand) Limited trading as Healthcare Logistics Docusate sodium + Coloxyl with Senna tablet Pharmacy Retailing (New Zealand) sennosides Limited trading as Healthcare Logistics *Laxsol tablet Pharmacy Retailing (New Zealand) Limited trading as Healthcare Logistics Glycerol *Glycerol Suppositories PSM Healthcare Limited trading as API Consumer Brands Sennosides *Senokot tablet Reckitt Benckiser (New Zealand) Limited Sodium picosulfate Dulcolax SP Drops oral solution Sanofi-Aventis New Zealand Limited PHARMAC funding *Pharmaceutical Schedule Lax-Tab tablets, Lax-Suppositories Bisacodyl, Coloxyl tablets and Glycerol Suppositories are fully-funded only on a prescription. Senokot tablets are part- funded. Previous MARC Misuse of stimulant laxatives has not been discussed previously. meetings International action Following a national safety review published in August 2020, the MHRA in the UK has introduced pack size restrictions, revised recommended ages for use -

1: Gastro-Intestinal System
1 1: GASTRO-INTESTINAL SYSTEM Antacids .......................................................... 1 Stimulant laxatives ...................................46 Compound alginate products .................. 3 Docuate sodium .......................................49 Simeticone ................................................... 4 Lactulose ....................................................50 Antimuscarinics .......................................... 5 Macrogols (polyethylene glycols) ..........51 Glycopyrronium .......................................13 Magnesium salts ........................................53 Hyoscine butylbromide ...........................16 Rectal products for constipation ..........55 Hyoscine hydrobromide .........................19 Products for haemorrhoids .................56 Propantheline ............................................21 Pancreatin ...................................................58 Orphenadrine ...........................................23 Prokinetics ..................................................24 Quick Clinical Guides: H2-receptor antagonists .......................27 Death rattle (noisy rattling breathing) 12 Proton pump inhibitors ........................30 Opioid-induced constipation .................42 Loperamide ................................................35 Bowel management in paraplegia Laxatives ......................................................38 and tetraplegia .....................................44 Ispaghula (Psyllium husk) ........................45 ANTACIDS Indications: -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Constpation Refworks
Guidelines for Management of Idiopathic Childhood Constipation Introduction • Constipation is common in childhood affecting up to 30% of the child population. Symptoms become chronic in more than one third of patients and constipation is a common reason for referral to secondary care. • ‘Idiopathic Constipation’ refers to constipation not explained by anatomical or physiological abnormalities. • A NICE guideline entitled ‘Diagnosis and management of idiopathic childhood constipation in primary and secondary care’ was published in 2010 and the RHSC paediatric department endorses its approach. Key steps are to: 1) Identify symptoms of constipation and faecal impaction through history and physical examination 2) Recognise features in history / examination indicative of alternative underlying pathology (termed red and amber flags) 3) Provide advice on diagnosis 4) Prescribe and supervise a disimpaction regimen (where evidence of faecal impaction exists) followed by a sustained course of maintenance laxative therapy. Lothian Guideline • Click on icons for quick link to our simple to use xxx YYY iiiii flow chart formulary referral checklist. • Referrals will not be accepted without evidence of use of the above guidance. • We have provided worked examples of common scenarios encountered in primary care (Figure 4). • Finally please see our links to other useful resources (Figure 5). Click b to return to top Lothian Guideline for Management of Idiopathic Childhood Constipation. Take a history - 2 or more from the following indicate that the child is constipated: • <3 stools per week............................................................................................................................ (type 3 or 4, see Bristol Stool Form Scale) Note - this does not apply to breast fed babies over 6wks who may stool less frequently. • Large stools that block the toilet or 'rabbit dropping' type 1 stool (see Bristol Stool Form Scale) • Overflow soiling (very loose, smelly stool passed without sensation) • Poor appetite that improves with passage of large stool. -
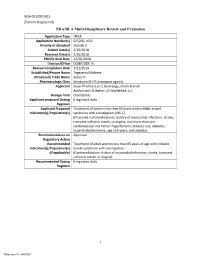
I NDA/BLA Multi-Disciplinary Review and Evaluation
NDA 021200 S015 Zelnorm (tegaserod) NDA/BLA Multi-Disciplinary Review and Evaluation Application Type sNDA Application Number(s) 021200, s015 Priority or Standard Standard Submit Date(s) 2/26/2018 Received Date(s) 2/26/2018 PDUFA Goal Date 12/26/2018 Division/Office DGIEP/ODE III Review Completion Date 3/22/2019 Established/Proper Name Tegaserod Maleate (Proposed) Trade Name Zelnorm Pharmacologic Class Serotonin (5-HT4) receptor agonist Applicant Sloan Pharma S.a.r.l, Bertrange, Cham Branch Authorized US Agent: US WorldMed, LLC Dosage form Oral tablets Applicant proposed Dosing 6 mg twice daily Regimen Applicant Proposed Treatment of women less than 65 years with irritable bowel Indication(s)/Population(s) syndrome with constipation (IBS-C). (Proposed contraindications: history of myocardial infarction, stroke, transient ischemic attack, or angina, and more than one cardiovascular risk factor: hypertension, tobacco use, diabetes, hypercholesterolemia, age ≥55 years, and obesity). Recommendation on Approval Regulatory Action Recommended Treatment of adult women less than 65 years of age with irritable Indication(s)/Population(s) bowel syndrome with constipation (if applicable) (Contraindication: history of myocardial infarction, stroke, transient ischemic attack, or angina). Recommended Dosing 6 mg twice daily Regimen i Reference ID: 4407897 NDA 021200 S015 Zelnorm (tegaserod) Table of Contents Reviewers of Multi-Disciplinary Review and Evaluation .............................................. 1 Glossary ........................................................................................................................ -

Laxatives Or Methylnaltrexone for the Management of Constipation in Palliative Care Patients (Review)
Laxatives or methylnaltrexone for the management of constipation in palliative care patients (Review) Candy B, Jones L, Goodman ML, Drake R, Tookman A This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2011, Issue 1 http://www.thecochranelibrary.com Laxatives or methylnaltrexone for the management of constipation in palliative care patients (Review) Copyright © 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 SUMMARY OF FINDINGS FOR THE MAIN COMPARISON . ..... 3 BACKGROUND .................................... 4 OBJECTIVES ..................................... 4 METHODS...................................... 5 RESULTS....................................... 7 Figure1. ..................................... 8 Figure2. ..................................... 9 DISCUSSION ..................................... 13 AUTHORS’CONCLUSIONS . 14 ACKNOWLEDGEMENTS . 15 REFERENCES..................................... 15 CHARACTERISTICSOFSTUDIES . .. 17 DATAANDANALYSES. 28 Analysis 1.1. Comparison 1 Methylnaltrexone versus placebo, Outcome 1 Proportion who had rescue-free laxation within 4hours..................................... 28 Analysis 1.2. Comparison 1 Methylnaltrexone versus placebo, Outcome 2 Laxation within 24 hours. 29 Analysis 1.3. Comparison 1 Methylnaltrexone versus placebo, Outcome 3 Tolerability: proportion -

Artigo Original / Original Article
ARQGA/1308 RANDOMIZED CLINICAL TRIAL COMPARING SODIUM PICOSULFATE WITH MANNITOL IN THE PREPARATION FOR COLONOSCOPY IN HOSPITALIZED PATIENTS Suzana MÜLLER, Carlos Fernando de Magalhães FRANCESCONI Ismael MAGUILNIK and Helenice Pankowsky BREYER ABSTRACT – Background - The cleansing of the colon for a colonoscopy exam must be complete so as to allow the visualization and inspection of the intestinal lumen. The ideal cleansing agent should be easily administered, have a low cost, and minimum collateral effects. Sodium picosulfate together with the magnesium citrate is a cathartic stimulant and mannitol is an osmotic laxative, both usually used for this purpose. Aims - Assess the colon cleanliness comparing the use of mannitol and sodium picosulfate as well as evaluate the level of patient satisfaction, the presence of foam, pain, and abdominal distension in hospitalized patients undergoing colonoscopy. Methods - A prospective, randomized, single-blind study with 80 patients that compared two groups: mannitol (40) and sodium picosulfate (40). Both groups received the same dietary orientation. The study was approved by the hospital’s Ethics and Research Committee. The endoscopist was blind to the type of preparation. Outcomes evaluated: level of the colon’s cleanliness, patient’s satisfaction, the presence of foam, abdominal pain and distension, and the duration of the exam. The data was analyzed by means of the chi-squared test for proportions and Mann-Whitney for independent samples. Results - There were no statistically significant differences between the groups in relation to the level of the colon’s cleanliness, patient’s satisfaction, the presence of foam, abdominal pain, and the duration of the exam. Fifteen percent of the exams of the mannitol group were interrupted while from the sodium picosulfate group it was 5%. -

Pharmaceutical Product Catalogue
PHARMACEUTICAL PRODUCT CATALOGUE Index of products LAXATIVES ....................................................................pp. 6 -11 · Emuliquen Simple · Emuliquen Laxante · Puntualsenna · Lactulosa Lainco · Clisteran · Kanova Adultos · Kanova Niños · Ezor · Plantago Ovata Lainco · Magnesia Lainco EVACUANTS ..............................................................pp.12 -15 · Evacuante Lainco Simple · Foslainco · Lainema · Enema Salino Lainco ANTISEPTICS .............................................................pp.16 - 21 · Curadona · Curadona Scrub · Curadona Gel · Curadona Vaginal · Yodinco · Yodinco Gel · Yodinco Scrub · Mercromina Film · Lainco Clorhexidina 2% Acuosa · Lainco Clorhexidina 0,5% Alcohólica · Lainco Clorhexidina 2% Alcohólica · Lainco Clorhexidina 2% Alcohólica Color · Lainco Clorhexidina Gel · Lainco Clorhexidina Scrub LOCAL ANAESTHETICS .................................pp. 22 - 23 · Tetracaína Lainco ANTI-DIARRHOEALS / ANTIFLATULENTS ..............................................pp. 22 - 23 · Ultra Adsorb ANTITOXICS ...........................................................pp. 24 - 27 · Carbon Ultra Adsorbente · Carboliq NASAL PREPARATIONS .................................pp. 28 - 29 · Lairesp · Lainasal Hidratante COUGH SUPPRESSANTS .............................pp. 28 - 29 · Laitos HYGIENE AND COSMETICS ...................pp. 30 - 31 · Gel Corporal Aloe Vera Lainco · Calamina Lainco · Vaselai LAINCO is a chemical company dedicated to the research, development, manufacture, packaging and marketing of pharmaceutical -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

WO 2008/019854 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (43) International Publication Date (10) International Publication Number 21 February 2008 (21.02.2008) PCT WO 2008/019854 Al (51) International Patent Classification: (74) Agents: BEST, Michael et al.; Lederer & Keller, Prinzre- A61K 9/00 (2006.01) A61K 9/50 (2006.01) gentenstrasse 16, 80538 Mϋnchen (DE). A61K 9/28 (2006.01) (81) Designated States (unless otherwise indicated, for every (21) International Application Number: kind of national protection available): AE, AG, AL, AM, PCT/EP2007/007243 AT,AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, (22) International Filing Date: 16 August 2007 (16.08.2007) ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, KZ, LA, LC, LK, (25) Filing Language: English LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PG, PH, PL, (26) Publication Language: English PT, RO, RS, RU, SC, SD, SE, SG, SK, SL, SM, SV, SY, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (30) Priority Data: ZM, ZW 06017263.2 18 August 2006 (18.08.2006) EP 11/516,573 7 September 2006 (07.09.2006) US (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant (for all designated States except US): LOSAN GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, PHARMA GMBH [DE/DE]; Otto-Hahn-Strasse 13, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, TM), 79395 Neuenburg (DE). -

Full Prescribing Information for Solution (3) CLENPIQ
HIGHLIGHTS OF PRESCRIBING INFORMATION ---------------------DOSAGE FORMS AND STRENGTHS---------------------- CLENPIQ oral solution: Each bottle contains 10 mg of sodium picosulfate, These highlights do not include all the information needed to use ® 3.5 g of magnesium oxide, and 12 g of anhydrous citric acid in 160 mL of CLENPIQ safely and effectively. See full prescribing information for solution (3) CLENPIQ. -------------------------------CONTRAINDICATIONS------------------------------ ® • Patients with severe reduced renal impairment (creatinine clearance less CLENPIQ (sodium picosulfate, magnesium oxide, and anhydrous citric than 30 mL/minute) (4, 5.3, 8.6) acid) oral solution • Gastrointestinal (GI) obstruction or ileus (4) Initial U.S. Approval: 2012 • Bowel perforation (4) • ----------------------------RECENT MAJOR CHANGES-------------------------- Toxic colitis or toxic megacolon (4) Indications and Usage (1) 08/2019 • Gastric retention (4) Dosage and Administration (2.1) 10/2019 • Hypersensitivity to any of the ingredients in CLENPIQ (4) Dosage and Administration (2.2) 08/2019, 10/2019 Dosage and Administration, Day-Before Dosage Regimen (2.3) -----------------------WARNINGS AND PRECAUTIONS------------------------ Removed 10/2019 • Risk of fluid and electrolyte abnormalities, arrhythmia, seizures, and renal Warnings and Precautions (5.1) 08/2019 impairment: Encourage adequate hydration, assess concurrent medications, and consider laboratory assessments prior to and after use. (5.1, 5.2, 5.3, 5.4, ----------------------------INDICATIONS AND USAGE--------------------------- 7.1) CLENPIQ® is a combination of sodium picosulfate, a stimulant laxative, and • Use in patients with renal impairment or taking concomitant medications magnesium oxide and anhydrous citric acid, which form magnesium citrate, that affect renal function: Use caution, ensure adequate hydration, and an osmotic laxative, indicated for cleansing of the colon as a preparation for consider testing.