2018 Oral Abstracts #HS 1 a Prospective, Randomized, Double
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sara Aghamohammadi, M.D
Sara Aghamohammadi, M.D. Philosophy of Care It is a privilege to care for children and their families during the time of their critical illness. I strive to incorporate the science and art of medicine in my everyday practice such that each child and family receives the best medical care in a supportive and respectful environment. Having grown up in the San Joaquin Valley, I am honored to join UC Davis Children's Hospital's team and contribute to the well-being of our community's children. Clinical Interests Dr. Aghamohammadi has always had a passion for education, she enjoys teaching principles of medicine, pediatrics, and critical care to medical students, residents, and nurses alike. Her clinical interests include standardization of practice in the PICU through the use of protocols. Her team has successfully implemented a sedation and analgesia protocol in the PICU, and she helped develop the high-flow nasal cannula protocol for bronchiolitis. Additionally, she has been involved in the development of pediatric pain order sets and is part of a multi-disciplinary team to address acute and chronic pain in pediatric patients. Research/Academic Interests Dr. Aghamohammadi has been passionate about Physician Health and Well-being and heads the Wellness Committee for the Department of Pediatrics. Additionally, she is a part of the Department Wellness Champions for the UC Davis Health System and has given presentations on the importance of Physician Wellness. After completing training in Physician Health and Well-being, she now serves as a mentor for the Train-the-Trainer Physician Health and Well-being Fellowship. -

Hand Surgery
Plastic & reconstructive surgery د.ﻣﺤﻤﺪ ﺟﺎﺳﻢ ﻣﺤﻤﺪ Lec 2 اﺧﺗﺻﺎص اﻟﺟراﺣﺔ اﻟﺗﻘوﯾﻣﯾﺔ 5TH Stage HAND SURGERY Congenital hand abnormalities SWANSON CLASSIFICATION OF CONGENITAL UPPER LIMB ABNORMALITIES I. Failure of Formation of Parts A. Transverse: truncated limb B. Longitudinal: Radial club hand (Preaxial Deficiency) Cleft hand (Central Deficiency) Ulnar club hand(postaxial deficiency) Phocomelia (Intercalary Deficiency) II. Failure of Differentiation or Separation of Parts A. Symphalangism B. Syndactyly C. Contracture: Arthrogryposis Trigger finger Clasped thumb Camptodactyly Clinodactyly III. Duplication: Polydactyly IV. Overgrowth: Macrodactyly V. Undergrowth: Thumb hypoplasia VI. Congenital Constriction Ring Syndrome VII. Generalized Skeletal Abnormalities and Syndromes. Preaxial Deficiency: Radial Club Hand: They are typically sporadic and unilateral, more common in males, and more common on the right side Radial dysplasias are commonly associated with syndromes including Fanconi anemia, thrombocytopenia absent radius (TAR) syndrome, Holt-Oram syndrome (associated with cardiac septal defects), and VATER(vertebral abnormality, anal imperforation, tracheoesophageal fistula, radial, or renal anomalies. The clinical manifestation of radial club hand is a shortened forearm with radial deviation at the wrist. The pathology affects all structures on the preaxial side of the limb: skeleton, musculotendinous units, joints, neurovascular structures, and soft tissue. CLASSIFICATION OF RADIAL DYSPLASIA I-Short radius II- Hypoplastic radius III- Partial absence of radius IV- Total absence of radius Management Type I mild type II dysplasia may only require splinting . Centralization or radialization of wrist with tendon transfer are the treatments of choice in severe type II, and in types III and IV; repair should be performed at 6 to 12 months of age. In pt with absent thumb, pollicization should be done after 6 month from 1st operation. -

University of Washington Orthopaedics & Sports Medicine
Discoveries 2018 University of Washington Orthopaedics & Sports Medicine University of Washington Department of Orthopaedics and Sports Medicine Discoveries 2018 Department of Orthopaedics and Sports Medicine University of Washington Seattle, WA 98195 EDITOR-IN-CHIEF: Howard A. Chansky, MD [email protected] ASSISTANT EDITORS: Christopher H. Allan, MD [email protected] Stephen A. Kennedy, MD, FRCSC [email protected] Adam A. Sassoon, MD, MS [email protected] MANAGING EDITOR: Fred Westerberg [email protected] Front Cover Illustration: Angie Kennedy, MSc, is a Seattle-based mixed media artist. She specializes in custom collage pieces that use mementos and artifacts to celebrate people and special life events. She drew on her experience as a former scientific researcher to create this collage of images from the pages of the current publication. The ‘W’ in the background is a nod to the University of Washington with an overlay of the current imagery arranged in an abstract assemblage. For more information www.americanheavyweight.com A pdf of this publication is available at our website: www.orthop.washington.edu. Permission Requests: All inquiries should be directed to the Managing Editor, University of Washington, Department of Orthopaedics and Sports Medicine, 1959 NE Pacific Street, Box 356500, Seattle, WA 98195-6500, or at the email address above. Contents 1 Foreword 2 From The Assistant Editors: The Modern Art of Musculoskeletal Research, Education, and Clinical Care 3 2018 Distinguished Alumnus, David J. Belfie, MD 4 New Faculty 6 Department of Orthopaedics and Sports Medicine Faculty 12 Visiting Lecturers Validation of a Rabbit Model of Trauma-Induced 14 Brandon J. Ausk, PhD, Philippe Huber, BS, Heterotopic Ossification Ted S. -

349 D.R. Laub Jr. (Ed.), Congenital Anomalies of the Upper
Index A dermatological anomalies , 182 Abductor digiti minimi (ADM) transfer , 102–103 skeletal abnormalities , 182 Abductor pollicis brevis (APB) , 186–187 upper extremity anomalies , 182, 183 ABS. See Amniotic band syndrome (ABS) visceral anomalies , 182 Achondroplasia defi nition of , 179 classifi cation/characterization , 338 description , 32, 33 defi nition of , 337–338 epidemiology of , 181 genetics , 338 genetics and embryology management , 338 molecular etiology , 180 Acrocephalosyndactyly syndrome , 32, 33, 179 prenatal diagnosis , 180–181 Acrosyndactyly repair, ABS , 300–302 molecular basis of , 180 Adactylic group IV symbrachydactyly , 129, 131 postoperative care and complications , 187 Al-Awadi syndrome , 154 treatment Amniotic band syndrome (ABS) APB release , 186–187 acrosyndactyly repair , 300–302 border digits syndactylies , 184 anesthesia concerns of fi rst web space release , 186 induction and maintenance of anesthesia , 43 patient age , 183 postoperative concerns , 43 secondary revisions , 187 preoperative preparation , 42–43 symphalangism , 184 classifi cation , 298 syndactyly ( see Syndactyly) clinical presentation thumb radial clinodactyly , 186–187 acrosyndactyly , 297–298 type II apert hand , 187–188 digital malformation , 297 Apical ectodermal ridge (AER) , 3–5 distal skeletal bones tapering , 297–298 Arthrogryposis , 210 hand deformity , 297 classic arthrogryposis , 305–306, 308 complications , 302 classifi cation , 305, 306 constriction band release defi nition of , 229, 230, 305 Upton’s technique , 299, 301 de-rotation osteotomy, shoulder , 308, 309 z-plasty , 299–300 distal , 230–231 ( see Distal arthrogryposis) diagnosis of , 296 elbow treatment digital hypoplasia reconstruction , 302 muscle transfers , 310–311 etiology of , 295–296 nonoperative management , 308 preoperative considerations , 299 posterior elbow capsular release , 309 treatment , 299 radial head dislocations , 311 Amniotic constriction band syndrome. -
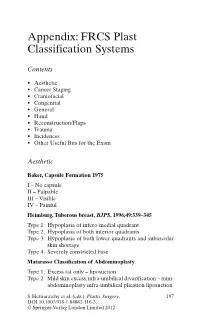
Appendix: FRCS Plast Classification Systems
Appendix: FRCS Plast Classification Systems Contents • Aesthetic • Cancer Staging • Craniofacial • Congenital • General • Hand • Reconstruction/Flaps • Trauma • Incidences • Other Useful Bits for the Exam Aesthetic Baker, Capsule Formation 1975 I – No capsule II – Palpable III – Visible IV – Painful Heimburg, Tuberous breast, BJPS , 1996;49:339–345 Type 1: Hypoplasia of infero-medial quadrant Type 2: Hypoplasia of both inferior quadrants Type 3: Hypoplasia of both lower quadrants and subareolar skin shortage Type 4: Severely constricted base Matarasso Classification of Abdominoplasty Type 1: Excess fat only – liposuction Type 2: Mild skin excess, infra-umbilical divarification – mini- abdominoplasty infra-umbilical plication liposuction S. Hettiaratchy et al. (eds.), Plastic Surgery, 197 DOI 10.1007/978-1-84882-116-3, © Springer-Verlag London Limited 2012 198 Appendix: FRCS Plast Classification Systems Type 3: Moderate skin excess, infra and superior divarifica- tion – As above Type 4: Severe skin excess – Standard abdominoplasty with plication and liposuction Paysk zones around an expander Inner zone: Fibrin layer with macrophages Central zone: Fibroblasts and myofibroblasts Transitional zone: Loose collagen Outer zone: Blood vessels and collagen Regnault classification of ptosis 1st degree: Nipples at or above IMF 2nd degree: Nipples below IMF but above most dependant portion of the breast 3rd degree: Nipples below the most dependant portion of the breast • Pseudo-ptosis – where the majority of the breast mound lies below the IMF but -

Polydactyly of the Hand
A Review Paper Polydactyly of the Hand Katherine C. Faust, MD, Tara Kimbrough, BS, Jean Evans Oakes, MD, J. Ollie Edmunds, MD, and Donald C. Faust, MD cleft lip/palate, and spina bifida. Thumb duplication occurs in Abstract 0.08 to 1.4 per 1000 live births and is more common in Ameri- Polydactyly is considered either the most or second can Indians and Asians than in other races.5,10 It occurs in a most (after syndactyly) common congenital hand ab- male-to-female ratio of 2.5 to 1 and is most often unilateral.5 normality. Polydactyly is not simply a duplication; the Postaxial polydactyly is predominant in black infants; it is most anatomy is abnormal with hypoplastic structures, ab- often inherited in an autosomal dominant fashion, if isolated, 1 normally contoured joints, and anomalous tendon and or in an autosomal recessive pattern, if syndromic. A prospec- ligament insertions. There are many ways to classify tive San Diego study of 11,161 newborns found postaxial type polydactyly, and surgical options range from simple B polydactyly in 1 per 531 live births (1 per 143 black infants, excision to complicated bone, ligament, and tendon 1 per 1339 white infants); 76% of cases were bilateral, and 3 realignments. The prevalence of polydactyly makes it 86% had a positive family history. In patients of non-African descent, it is associated with anomalies in other organs. Central important for orthopedic surgeons to understand the duplication is rare and often autosomal dominant.5,10 basic tenets of the abnormality. Genetics and Development As early as 1896, the heritability of polydactyly was noted.11 As olydactyly is the presence of extra digits. -

Clinical and Molecular Genetic Study of Kindreds with Limbs and Neurological Anomalies
Clinical and Molecular Genetic Study of Kindreds with Limbs and Neurological Anomalies PhD Dissertation By Muhammad Afzal Human Genetics 2020 Human Genetics Lab, Department of Zoology Faculty of Biological Sciences Quaid-i-Azam University, Islamabad, Pakistan Acknowledgments I offer my humblest and sincere thanks to Almighty ALLAH, Who bestowed me with potential and ability to make a solid contribution to already existing ocean of knowledge and I also feel pleasure to offer thanks for Holy Prophet Hazrat Muhammad (PBUH), Who showed us the right path and enabled us to recognize our creator. This work would not have been possible without the support and encouragement of my teacher Dr. Sajid Malik, under whose supervision I chose this topic and began the thesis. Actually, when I registered at QAU, I was nothing but today I would able to submit this thesis. He always has been a continuous source of encouragement for me. I am grateful to Dean Faculty of Biological Sciences; Prof. Dr. Muhammad Shahab and chairman department of Animal Sciences; Assoc. Prof. Dr. Sajid Malik for providing pre-requisites for this work and thus facilitating this task. Clerical and technical assistant in scientific research is an undeniable important element. So I am righteous in thanking Syed Mujahid Hussain (Lab. assistant), Naeem Masih and Samiullah for their thorough and in time assistance. I am highly thankful to Rana Mazhar (Principal Punjab group of colleges) because he provided me the financial assistance whenever I need at any time at any occasion during the field work and compilation of thesis and he never disappointed me. -

Thumb Duplication: Concepts and Techniques Michael A
CORE Metadata, citation and similar papers at core.ac.uk Provided by PubMed Central Review Article Clinics in Orthopedic Surgery 2012;4:1-17 • http://dx.doi.org/10.4055/cios.2012.4.1.1 Thumb Duplication: Concepts and Techniques Michael A. Tonkin, MD Department of Hand Surgery and Peripheral Nerve Surgery, University of Sydney, Royal North Shore Hospital, St. Leonards and Department of Hand Surgery, University of Sydney, Children’s Hospital at Westmead, Westmead, Australia Within the Oberg, Manske, Tonkin (OMT) classifi cation, thumb duplications are a failure of formation and/or differentiation affect- ing the radial-ulnar axis of the hand plate. The Wassel description of seven types of thumb duplication provides a good structure from which an approach to management is based. The aim of surgical reconstruction is to obtain a stable, mobile thumb of ad- equate size and appropriate shape. The most common form of reconstruction is removal of the lesser digit and reconstruction of the dominant digit. Surgical techniques address the problems of deviation, instability and lack of size. The disadvantages of the Bilhaut-Cloquet procedure, these being joint stiffness and a nail ridge, may be lesser concerns when reconstruction of one digit will not create a satisfactory thumb of adequate mobility, stability, alignment and size. Complicated problems of triphalangism, triplication, ulnar dimelia and the rare circumstance in which neither of the duplicated thumbs may be adequately reconstructed present specifi c challenges which demand alternative techniques. Keywords: Thumb duplication, Classifi cation, Assessment, Reconstruction Thumb duplication is classified within the International anomaly (Table 1).2) It recognises that formation and dif- Federation of Societies for Surgery of the Hand (IFSSH)/ ferentiation occur together, not as separate independent Swanson classifi cation of congenital anomalies of the hand processes, and directs us to the site of insult in the devel- and upper limb as a “duplication” (group 3).1) Included are oping limb bud. -

Pediatric Orthopedics in Practice, DOI 10.1007/978-3-662-46810-4, © Springer-Verlag Berlin Heidelberg 2015 880 Backmatter
879 Backmatter Subject Index – 880 F. Hefti, Pediatric Orthopedics in Practice, DOI 10.1007/978-3-662-46810-4, © Springer-Verlag Berlin Heidelberg 2015 880 Backmatter Subject index Bold letters: Principal article Italics: Illustrations A Acetylsalicylic acid 303, 335 Adolescent scoliosis Amyloidosis 663 Acheiropodia 804 7 Scoliosis Amyoplasia 813–814 Abducent nerve paresis 752, Achievement by proxy 10, 11 AFO 7 Ankle Foot Orthosis Anaerobes 649, 652, 657 816 Achilles tendon Aggrecan 336, 367, 762 ANA 7 antinuclear antibodies Abducted pes planovalgus – lengthening 371, 426, 431, aggressive osteomyelitis Analysis, gait 488, 490–497 433, 434, 436, 439, 443, 464, 7 osteomyelitis, aggressive 7 Gait analysis Abduction contracture 468, 475, 485, 487–490, 493, Agonist 281, 487, 492, 493, Anchor 169, 312, 550, 734 7 contracture 496, 816, 838, 840 495, 498, 664, 832, 835, 840, Andersen classification abduction pants 219–221 – shortening 358, 418, 431, 868 7 classification, Andersen Abduction splint 212, 218–221, 433, 464, 465, 467, 468, 475, Ahn classification 366 Andry, Nicolas 21, 22 248, 850 489, 496, 838 Aitken classification (congenital Anesthesia 26, 38, 135, 154, Abduction Achondrogenesis 750, 751, femoral deficiency ) 7 classi- 162, 174, 221, 243, 247, 248, – hip 195, 198, 199, 212, 213, 756, 758–760, 769 fication, femoral deficiency 255, 281, 303, 385, 386, 400, 214, 218, 219, 220, 221, Achondroplasia 56, 163, 166, Akin osteotomy 477, 479 500, 506, 559, 568, 582–585, 241–245, 247, 248, 251, 255, 242, 270, 271, 353, 409, 628, Albers-Schönberg -

Journal of Hand Surgery (European Volume)
Journal of Hand Surgery (European Volume) http://jhs.sagepub.com/ FESSH Abstracts J Hand Surg Eur Vol 2014 39: S1 DOI: 10.1177/1753193414530610 The online version of this article can be found at: http://jhs.sagepub.com/content/39/1_suppl/S1 Published by: http://www.sagepublications.com On behalf of: British Society for Surgery of the Hand Additional services and information for Journal of Hand Surgery (European Volume) can be found at: Email Alerts: http://jhs.sagepub.com/cgi/alerts Subscriptions: http://jhs.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav >> Version of Record - May 19, 2014 What is This? Downloaded from jhs.sagepub.com at UCSF LIBRARY & CKM on November 19, 2014 JHS(E) FESSH Abstracts The Journal of Hand Surgery (European Volume) 39E(Supplement 1) S1–S162 © The Author(s) 2014 Reprints and permissions: sagepub.co.uk/journalsPermissions.nav DOI: 10.1177/1753193414530610 jhs.sagepub.com A-0006 The association between cubital Clinical Relevance: This study provided useful infor- tunnel morphology and ulnar neuropathy in mation regarding the pathology and surgical treat- patients with elbow osteoarthritis ment strategies for cubital tunnel syndrome in patients with elbow osteoarthritis. Y Kawanishi1, J Miyake2, S Omori1, T Murase1, K Shimada3 (1) Department of Orthopaedic Surgery, Osaka University Graduate School of Medicine, Osaka, Japan A-0023 Clinical results of percutaneous (2) Department of Orthopaedic Surgery, Sakai City Hospital, needle fasciotomy for Dupuytren’s Japan disease – Is there any correlation between (3) Department of Orthopaedic Surgery, Osaka Koseinenkin preoperative severity or Dupuytren’s Hospital, Osaka, Japan diathesis and clinical results? Purpose: Morphological changes in the cubital tunnel Y Abe, S Tokunaga during elbow motion in patients with elbow osteoar- Sakura Orthopaedic Hospital, Hand Surgery Center, Sakura thritis have not been examined in vivo. -

Hand & Upper Extremity AOAO Board Review
Hand & Upper Extremity AOAO Board Review Matt Koepplinger, DO Assistant Professor Department of Orthopaedic Surgery No Disclosures Flexor tendon • Nonoperative partial lacerations < 60% of tendon width • Operative >60% of width • ≥ 50-60% laceration with triggering →epitendinous suture • perform repair within three weeks • # of suture strands cross the repair site is most important • ideal suture purchase 10mm from cut edge • Dorsal core sutures stronger • epitendinous suture improves tendon gliding, improves strength • Complications • Adhesions (zone 2) • 15-25% rerupture rate Jersey Finger • Avulsion injury of FDP from distal phalanx • Ring finger most likely • More retracted → sooner treatment • Treatment operative • Direct repair • ORIF if bone involved • DIP fusion if chronic/unstable • Two stage recon??? Lumbrical Plus Finger • paradoxical extension of the IP joints while attempting to flex the fingers • with FDP laceration, FDP contraction leads to pull on lumbricals • Treat with lumbrical release, tendon repair if acute • do NOT suture flexor-extensor mechanisms over bone Quadrigia Effect • active flexion lag fingers adjacent to a digit with repaired FDP tendon • a functional shortening of the FDP tendon • >1 cm advancement • Adhesions • FDP MF, RF, SF common belly • excursion combined tendons equal to shortest • Treat • Observe • Release FDP Pulley system • 25% of A2 and 100% of A4 can be incised with little resulting functional deficit • Blood supply of tendon • Indirect • diffusion through synovial sheaths • tendons located -
Klasifikace Vrozených Defektů Horní Končetiny Classification of Congenital Differences of the Upper Extremity
SOUBORNÉ REFERÁTY REVIEWS KLASIFIKACE VROZENÝCH DEFEKtů HORNÍ Končetiny CLASSIFICATION OF CONGENITAL DIFFERENCES OF THE UPPER EXTREMITY TOSHIHIKO OGINO, MD, PHD Chairman of the Sapporo Hand Surgery & Congenital Hand Differences Center, Orthopaedic Hokushin-higashi Hospital ABSTRACT Swanson et al tried to classify congenital hand anomalies according to the genetic cause and reported his classification in 1976. Since then, modifications on this classification were made and this classification was adopted by the International Federation of Society for Surgery of the Hand (IFSSH). It has been used widely as an IFSSH classification. It is relatively easy to use this classification, but it has its own limitations. The biggest one occurs in the classification of ectrodactyly. In order to solve these problems, the authors conducted clinical ad experimental studies and found that there should be at least four different types of teratogenic mechanisms of congenital defect of the digits. The first one is longitudinal deficiencies due to mesenchymal cell death in an early developmental stage; the second is abnormal induction of digital ray numbers in the hand plate including cleft hand, central polydactyly and syndactyly. The third is constriction band syndrome, which is caused after digital radiations have been formed, and the fourth is transverse deficiency, in which the critical period is not known. Based on these studies, the author modified IFSSH classification and it was adopted by the Japanese Society for Surgery of the Hand and is called Japanese modification of the IFSSH classification (Japanese modification). In this paper, the author introduced the Japanese modification of the IFSSH classification and described some recommendations.