Hand & Upper Extremity AOAO Board Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sara Aghamohammadi, M.D
Sara Aghamohammadi, M.D. Philosophy of Care It is a privilege to care for children and their families during the time of their critical illness. I strive to incorporate the science and art of medicine in my everyday practice such that each child and family receives the best medical care in a supportive and respectful environment. Having grown up in the San Joaquin Valley, I am honored to join UC Davis Children's Hospital's team and contribute to the well-being of our community's children. Clinical Interests Dr. Aghamohammadi has always had a passion for education, she enjoys teaching principles of medicine, pediatrics, and critical care to medical students, residents, and nurses alike. Her clinical interests include standardization of practice in the PICU through the use of protocols. Her team has successfully implemented a sedation and analgesia protocol in the PICU, and she helped develop the high-flow nasal cannula protocol for bronchiolitis. Additionally, she has been involved in the development of pediatric pain order sets and is part of a multi-disciplinary team to address acute and chronic pain in pediatric patients. Research/Academic Interests Dr. Aghamohammadi has been passionate about Physician Health and Well-being and heads the Wellness Committee for the Department of Pediatrics. Additionally, she is a part of the Department Wellness Champions for the UC Davis Health System and has given presentations on the importance of Physician Wellness. After completing training in Physician Health and Well-being, she now serves as a mentor for the Train-the-Trainer Physician Health and Well-being Fellowship. -
Clinical Excellence Series Volume V an Evidence-Based Approach to Traumatic Emergencies
Clinical Excellence Series n Volume V An Evidence-Based Approach To Traumatic Emergencies Inside Neck Trauma: Don’t Put Your Neck On The Line Orthopedic Sports Injuries: Off The Sidelines And Into The Emergency Department Blunt Abdominal Trauma: Priorities, Procedures, And Pragmatic Thinking Wrist Injuries: Emergency Imaging And Management Brought to you exclusively by the publisher of: An Evidence-Based Approach To Traumatic Emergencies CEO: Robert Williford President & Publisher: Stephanie Ivy Associate Editor & CME Director: Jennifer Pai • Associate Editor: Dorothy Whisenhunt Director of Member Services: Liz Alvarez • Marketing & Customer Service Coordinator: Robin Williford Direct all questions to EB Medicine: 1-800-249-5770 • Fax: 1-770-500-1316 • Non-U.S. subscribers, call: 1-678-366-7933 EB Medicine • 5550 Triangle Pkwy Ste 150 • Norcross, GA 30092 E-mail: [email protected] • Web Site: www.ebmedicine.net The Emergency Medicine Practice Clinical Excellence Series, Volume V: An Evidence-Based Approach To Traumatic Emergencies is published by EB Practice, LLC, 5550 Triangle Pkwy Ste 150, Norcross, GA 30092. Opinions expressed are not necessarily those of this publication. Mention of products or services does not constitute endorsement. This publication is intended as a general guide and is intended to supplement, rather than substitute, professional judgment. It covers a highly technical and complex subject and should not be used for making specific medical decisions. The materials contained herein are not intended to establish policy, procedure, or standard of care. Emergency Medicine Practice, The Emergency Medicine Practice Clinical Excel- lence Series, and An Evidence-Based Approach to Traumatic Emergencies are trademarks of EB Practice, LLC. -

Broken Bones: Common Pediatric Lower Extremity Fractures—Part III
10173-06_ON2506-Hart.qxd 11/9/06 3:51 PM Page 390 Broken Bones: Common Pediatric Lower Extremity Fractures—Part III Erin S. Hart ▼ Brenda Luther ▼ Brian E. Grottkau Lower extremity injuries and fractures occur frequently in young usually have pain with hamstring stretching and hip flex- children and adolescents. Nurses are often one of the first ion/abduction). Patients also frequently demonstrate an healthcare providers to assess a child with an injury or fracture. antalgic gait and have pain during their activity or sport. Although basic fracture care and principles can be applied, An anteroposterior radiograph of the pelvis usually reveals nurses caring for these young patients must have a good under- the avulsed fragment. Comparative views of the contralat- standing of normal bone growth and development as well as eral side are often helpful in confirming the diagnosis and avoiding further unnecessary advanced imaging studies. common mechanisms of injury and fracture patterns seen in This injury is usually treated symptomatically and often children. Similar to many of the injuries in the upper extremity, involves rest, application of ice, and relaxation of the in- fractures in the lower extremity in children often can be treated volved tendon (O’Kane, 1999). Conservative treatment of nonoperatively with closed reduction and casting. However, this pelvic avulsion fractures is usually successful. Crutches are article will also review several lower extremity fractures that often needed for several weeks to reduce symptoms and frequently require surgical intervention to obtain a precise rest the extremity involved. Complications following pelvic anatomical reduction. Common mechanisms of injury, fracture avulsion fractures in children are rare, and most patients patterns, and current management techniques will be discussed. -

Hand Surgery
Plastic & reconstructive surgery د.ﻣﺤﻤﺪ ﺟﺎﺳﻢ ﻣﺤﻤﺪ Lec 2 اﺧﺗﺻﺎص اﻟﺟراﺣﺔ اﻟﺗﻘوﯾﻣﯾﺔ 5TH Stage HAND SURGERY Congenital hand abnormalities SWANSON CLASSIFICATION OF CONGENITAL UPPER LIMB ABNORMALITIES I. Failure of Formation of Parts A. Transverse: truncated limb B. Longitudinal: Radial club hand (Preaxial Deficiency) Cleft hand (Central Deficiency) Ulnar club hand(postaxial deficiency) Phocomelia (Intercalary Deficiency) II. Failure of Differentiation or Separation of Parts A. Symphalangism B. Syndactyly C. Contracture: Arthrogryposis Trigger finger Clasped thumb Camptodactyly Clinodactyly III. Duplication: Polydactyly IV. Overgrowth: Macrodactyly V. Undergrowth: Thumb hypoplasia VI. Congenital Constriction Ring Syndrome VII. Generalized Skeletal Abnormalities and Syndromes. Preaxial Deficiency: Radial Club Hand: They are typically sporadic and unilateral, more common in males, and more common on the right side Radial dysplasias are commonly associated with syndromes including Fanconi anemia, thrombocytopenia absent radius (TAR) syndrome, Holt-Oram syndrome (associated with cardiac septal defects), and VATER(vertebral abnormality, anal imperforation, tracheoesophageal fistula, radial, or renal anomalies. The clinical manifestation of radial club hand is a shortened forearm with radial deviation at the wrist. The pathology affects all structures on the preaxial side of the limb: skeleton, musculotendinous units, joints, neurovascular structures, and soft tissue. CLASSIFICATION OF RADIAL DYSPLASIA I-Short radius II- Hypoplastic radius III- Partial absence of radius IV- Total absence of radius Management Type I mild type II dysplasia may only require splinting . Centralization or radialization of wrist with tendon transfer are the treatments of choice in severe type II, and in types III and IV; repair should be performed at 6 to 12 months of age. In pt with absent thumb, pollicization should be done after 6 month from 1st operation. -

University of Washington Orthopaedics & Sports Medicine
Discoveries 2018 University of Washington Orthopaedics & Sports Medicine University of Washington Department of Orthopaedics and Sports Medicine Discoveries 2018 Department of Orthopaedics and Sports Medicine University of Washington Seattle, WA 98195 EDITOR-IN-CHIEF: Howard A. Chansky, MD [email protected] ASSISTANT EDITORS: Christopher H. Allan, MD [email protected] Stephen A. Kennedy, MD, FRCSC [email protected] Adam A. Sassoon, MD, MS [email protected] MANAGING EDITOR: Fred Westerberg [email protected] Front Cover Illustration: Angie Kennedy, MSc, is a Seattle-based mixed media artist. She specializes in custom collage pieces that use mementos and artifacts to celebrate people and special life events. She drew on her experience as a former scientific researcher to create this collage of images from the pages of the current publication. The ‘W’ in the background is a nod to the University of Washington with an overlay of the current imagery arranged in an abstract assemblage. For more information www.americanheavyweight.com A pdf of this publication is available at our website: www.orthop.washington.edu. Permission Requests: All inquiries should be directed to the Managing Editor, University of Washington, Department of Orthopaedics and Sports Medicine, 1959 NE Pacific Street, Box 356500, Seattle, WA 98195-6500, or at the email address above. Contents 1 Foreword 2 From The Assistant Editors: The Modern Art of Musculoskeletal Research, Education, and Clinical Care 3 2018 Distinguished Alumnus, David J. Belfie, MD 4 New Faculty 6 Department of Orthopaedics and Sports Medicine Faculty 12 Visiting Lecturers Validation of a Rabbit Model of Trauma-Induced 14 Brandon J. Ausk, PhD, Philippe Huber, BS, Heterotopic Ossification Ted S. -

349 D.R. Laub Jr. (Ed.), Congenital Anomalies of the Upper
Index A dermatological anomalies , 182 Abductor digiti minimi (ADM) transfer , 102–103 skeletal abnormalities , 182 Abductor pollicis brevis (APB) , 186–187 upper extremity anomalies , 182, 183 ABS. See Amniotic band syndrome (ABS) visceral anomalies , 182 Achondroplasia defi nition of , 179 classifi cation/characterization , 338 description , 32, 33 defi nition of , 337–338 epidemiology of , 181 genetics , 338 genetics and embryology management , 338 molecular etiology , 180 Acrocephalosyndactyly syndrome , 32, 33, 179 prenatal diagnosis , 180–181 Acrosyndactyly repair, ABS , 300–302 molecular basis of , 180 Adactylic group IV symbrachydactyly , 129, 131 postoperative care and complications , 187 Al-Awadi syndrome , 154 treatment Amniotic band syndrome (ABS) APB release , 186–187 acrosyndactyly repair , 300–302 border digits syndactylies , 184 anesthesia concerns of fi rst web space release , 186 induction and maintenance of anesthesia , 43 patient age , 183 postoperative concerns , 43 secondary revisions , 187 preoperative preparation , 42–43 symphalangism , 184 classifi cation , 298 syndactyly ( see Syndactyly) clinical presentation thumb radial clinodactyly , 186–187 acrosyndactyly , 297–298 type II apert hand , 187–188 digital malformation , 297 Apical ectodermal ridge (AER) , 3–5 distal skeletal bones tapering , 297–298 Arthrogryposis , 210 hand deformity , 297 classic arthrogryposis , 305–306, 308 complications , 302 classifi cation , 305, 306 constriction band release defi nition of , 229, 230, 305 Upton’s technique , 299, 301 de-rotation osteotomy, shoulder , 308, 309 z-plasty , 299–300 distal , 230–231 ( see Distal arthrogryposis) diagnosis of , 296 elbow treatment digital hypoplasia reconstruction , 302 muscle transfers , 310–311 etiology of , 295–296 nonoperative management , 308 preoperative considerations , 299 posterior elbow capsular release , 309 treatment , 299 radial head dislocations , 311 Amniotic constriction band syndrome. -
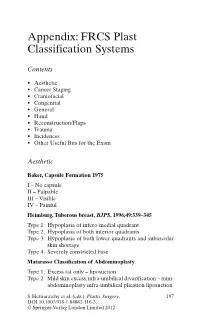
Appendix: FRCS Plast Classification Systems
Appendix: FRCS Plast Classification Systems Contents • Aesthetic • Cancer Staging • Craniofacial • Congenital • General • Hand • Reconstruction/Flaps • Trauma • Incidences • Other Useful Bits for the Exam Aesthetic Baker, Capsule Formation 1975 I – No capsule II – Palpable III – Visible IV – Painful Heimburg, Tuberous breast, BJPS , 1996;49:339–345 Type 1: Hypoplasia of infero-medial quadrant Type 2: Hypoplasia of both inferior quadrants Type 3: Hypoplasia of both lower quadrants and subareolar skin shortage Type 4: Severely constricted base Matarasso Classification of Abdominoplasty Type 1: Excess fat only – liposuction Type 2: Mild skin excess, infra-umbilical divarification – mini- abdominoplasty infra-umbilical plication liposuction S. Hettiaratchy et al. (eds.), Plastic Surgery, 197 DOI 10.1007/978-1-84882-116-3, © Springer-Verlag London Limited 2012 198 Appendix: FRCS Plast Classification Systems Type 3: Moderate skin excess, infra and superior divarifica- tion – As above Type 4: Severe skin excess – Standard abdominoplasty with plication and liposuction Paysk zones around an expander Inner zone: Fibrin layer with macrophages Central zone: Fibroblasts and myofibroblasts Transitional zone: Loose collagen Outer zone: Blood vessels and collagen Regnault classification of ptosis 1st degree: Nipples at or above IMF 2nd degree: Nipples below IMF but above most dependant portion of the breast 3rd degree: Nipples below the most dependant portion of the breast • Pseudo-ptosis – where the majority of the breast mound lies below the IMF but -

Polydactyly of the Hand
A Review Paper Polydactyly of the Hand Katherine C. Faust, MD, Tara Kimbrough, BS, Jean Evans Oakes, MD, J. Ollie Edmunds, MD, and Donald C. Faust, MD cleft lip/palate, and spina bifida. Thumb duplication occurs in Abstract 0.08 to 1.4 per 1000 live births and is more common in Ameri- Polydactyly is considered either the most or second can Indians and Asians than in other races.5,10 It occurs in a most (after syndactyly) common congenital hand ab- male-to-female ratio of 2.5 to 1 and is most often unilateral.5 normality. Polydactyly is not simply a duplication; the Postaxial polydactyly is predominant in black infants; it is most anatomy is abnormal with hypoplastic structures, ab- often inherited in an autosomal dominant fashion, if isolated, 1 normally contoured joints, and anomalous tendon and or in an autosomal recessive pattern, if syndromic. A prospec- ligament insertions. There are many ways to classify tive San Diego study of 11,161 newborns found postaxial type polydactyly, and surgical options range from simple B polydactyly in 1 per 531 live births (1 per 143 black infants, excision to complicated bone, ligament, and tendon 1 per 1339 white infants); 76% of cases were bilateral, and 3 realignments. The prevalence of polydactyly makes it 86% had a positive family history. In patients of non-African descent, it is associated with anomalies in other organs. Central important for orthopedic surgeons to understand the duplication is rare and often autosomal dominant.5,10 basic tenets of the abnormality. Genetics and Development As early as 1896, the heritability of polydactyly was noted.11 As olydactyly is the presence of extra digits. -

Treatment of Large Avulsion Injury in Perianal, Sacral, and Perineal
Hu et al. BMC Surgery (2019) 19:65 https://doi.org/10.1186/s12893-019-0529-1 RESEARCH ARTICLE Open Access Treatment of large avulsion injury in perianal, sacral, and perineal regions by island flaps or skin graft combined with vacuum assisted closure Fu Xing Hu1†, Xiao Xuan Hu2†, Xue Lin Yang1, Xing Hai Han1, Yong Bo Xu3, Kun Li3, Li Yan3*† and Hai Bo Chu3*† Abstract Background: Traumatic avulsion injuries to the anus, although uncommon, can result in serious complications and even death. Management of anal avulsion injuries remains controversial and challenging. This study aimed to investigate the clinical effects of treating large skin and subcutaneous tissue avulsion injuries in the perianal, sacral, and perineal regions with island flaps or skin graft combined with vacuum assisted closure. Methods: Island flaps or skin graft combined with vacuum assisted closure, diverting ileostomy, the rectum packed with double-lumen tubes around Vaseline gauze, negative pressure drainage with continuous distal washing, wounds with skin grafting as well as specialized treatment were performed. Results: The injuries healed in all patients. Six cases had incomplete perianal avulsion without wound infection. Wound infection was seen in four cases with annular perianal avulsion and was controlled, and the separated prowl lacuna was closed. The survival rate in 10 patients who underwent skin grafting was higher than 90%. No anal stenosis was observed after surgery, and ileostomy closure was performed at 3 months (six cases) and 6 months (four cases) after surgery, respectively. Conclusions: Covering a wound with an island flap or skin graft combined with vacuum assisted closure is successful in solving technical problems, protects the function of the anus and rapidly seals the wound at the same time. -

Extrusive Luxation and Lateral Luxation
NDR15 1/3/07 6:23 PM Page 411 15 Extrusive Luxation and Lateral Luxation F. M. Andreasen & J. O. Andreasen Definition Clinical findings Extrusive luxation (peripheral dislocation, Extrusion partial avulsion) Extruded teeth appear elongated and most often with Partial displacement of the tooth out of its socket. (Fig. lingual deviation of the crown, as the tooth is suspended 15.1) only by the palatinal gingiva (Fig. 15.1). There is always bleeding from the periodontal ligament. The percussion sound is dull. Lateral luxation Displacement of the tooth in a direction other than axially. Lateral luxation This is accompanied by comminution or fracture of the The crowns of laterally luxated teeth are in most cases dis- alveolar socket. (Fig. 15.2) placed lingually and are usually associated with fractures of the vestibular part of the socket wall (Fig. 15.2). Displace- Frequency ment of teeth after lateral luxation is normally evident by visual inspection. However, in case of marked inclination of The frequency of extrusive and lateral luxation han been maxillary teeth, it can be difficult to decide whether the found to be 7% and 11% among traumatized permanent trauma has caused minor abnormalities in tooth position. teeth examined at a major trauma center (7). In such cases, occlusion should be checked. Due to the fre- quently locked position of the tooth in the alveolus, clinical findings revealed by percussion and mobility tests are iden- Healing and pathology tical with those found in intruded teeth (see Chapter 13, Table 13.1). In these cases there is a complete rupture of the neurovas- cular supply to the pulp and severance of periodontal liga- Radiographic findings ment fibers leading to extrusion. -

Clinical and Molecular Genetic Study of Kindreds with Limbs and Neurological Anomalies
Clinical and Molecular Genetic Study of Kindreds with Limbs and Neurological Anomalies PhD Dissertation By Muhammad Afzal Human Genetics 2020 Human Genetics Lab, Department of Zoology Faculty of Biological Sciences Quaid-i-Azam University, Islamabad, Pakistan Acknowledgments I offer my humblest and sincere thanks to Almighty ALLAH, Who bestowed me with potential and ability to make a solid contribution to already existing ocean of knowledge and I also feel pleasure to offer thanks for Holy Prophet Hazrat Muhammad (PBUH), Who showed us the right path and enabled us to recognize our creator. This work would not have been possible without the support and encouragement of my teacher Dr. Sajid Malik, under whose supervision I chose this topic and began the thesis. Actually, when I registered at QAU, I was nothing but today I would able to submit this thesis. He always has been a continuous source of encouragement for me. I am grateful to Dean Faculty of Biological Sciences; Prof. Dr. Muhammad Shahab and chairman department of Animal Sciences; Assoc. Prof. Dr. Sajid Malik for providing pre-requisites for this work and thus facilitating this task. Clerical and technical assistant in scientific research is an undeniable important element. So I am righteous in thanking Syed Mujahid Hussain (Lab. assistant), Naeem Masih and Samiullah for their thorough and in time assistance. I am highly thankful to Rana Mazhar (Principal Punjab group of colleges) because he provided me the financial assistance whenever I need at any time at any occasion during the field work and compilation of thesis and he never disappointed me. -

After Intraspinal Repair of C5–T1 Brachial Plexus Avulsion Injury
Neurosurg Focus 16 (5):Article 7, 2004, Click here to return to Table of Contents Restoration of hand function and so called “breathing arm” after intraspinal repair of C5–T1 brachial plexus avulsion injury Case report THOMAS CARLSTEDT, M.D., D.M., F.R.C.S., PRAVEEN ANAND, M.D., F.R.C.P., MIN HTUT, M.R.C.P., PETER MISRA, M.D., F.R.C.P., AND MIKAEL SVENSSON, M.D., D.M. The Periphery Nerve Injury Unit, The Royal National Orthopaedic Hospital, Stanmore; Peripheral Neuropathy Unit, Imperial College, Hammersmith Hospital, London, United Kingdom; and Department of Neurosurgery, Karolinska Hospital, Stockholm, Sweden This 9-year-old boy sustained a complete right-sided C5–T1 brachial plexus avulsion injury in a motorcycle acci- dent. He underwent surgery 4 weeks after the accident. The motor-related nerve roots in all parts of the avulsed brachial plexus were reconnected to the spinal cord by reimplantation of peripheral nerve grafts. Recovery in the proximal part of the arm started 8 to 10 months later. Motor function was restored throughout the arm and also in the intrinsic mus- cles of the hand by 2 years postoperatively. The initial severe excruciating pain, typical after nerve root avulsions, dis- appeared completely with motor recovery. The authors observed good recruitment of regenerated motor units in all parts of the arm, but there were cocontractions. Transcranial magnetic stimulation produced response in all muscles, with prolonged latency and smaller amplitude compared with the intact side. There was inspiration-evoked muscle activity in proximal arm muscles—that is, the so-called “breathing arm” phenomenon.