349 D.R. Laub Jr. (Ed.), Congenital Anomalies of the Upper
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sara Aghamohammadi, M.D
Sara Aghamohammadi, M.D. Philosophy of Care It is a privilege to care for children and their families during the time of their critical illness. I strive to incorporate the science and art of medicine in my everyday practice such that each child and family receives the best medical care in a supportive and respectful environment. Having grown up in the San Joaquin Valley, I am honored to join UC Davis Children's Hospital's team and contribute to the well-being of our community's children. Clinical Interests Dr. Aghamohammadi has always had a passion for education, she enjoys teaching principles of medicine, pediatrics, and critical care to medical students, residents, and nurses alike. Her clinical interests include standardization of practice in the PICU through the use of protocols. Her team has successfully implemented a sedation and analgesia protocol in the PICU, and she helped develop the high-flow nasal cannula protocol for bronchiolitis. Additionally, she has been involved in the development of pediatric pain order sets and is part of a multi-disciplinary team to address acute and chronic pain in pediatric patients. Research/Academic Interests Dr. Aghamohammadi has been passionate about Physician Health and Well-being and heads the Wellness Committee for the Department of Pediatrics. Additionally, she is a part of the Department Wellness Champions for the UC Davis Health System and has given presentations on the importance of Physician Wellness. After completing training in Physician Health and Well-being, she now serves as a mentor for the Train-the-Trainer Physician Health and Well-being Fellowship. -

Advances in Understanding the Genetics of Syndromes Involving Congenital Upper Limb Anomalies
Review Article Page 1 of 10 Advances in understanding the genetics of syndromes involving congenital upper limb anomalies Liying Sun1#, Yingzhao Huang2,3,4#, Sen Zhao2,3,4, Wenyao Zhong1, Mao Lin2,3,4, Yang Guo1, Yuehan Yin1, Nan Wu2,3,4, Zhihong Wu2,3,5, Wen Tian1 1Hand Surgery Department, Beijing Jishuitan Hospital, Beijing 100035, China; 2Beijing Key Laboratory for Genetic Research of Skeletal Deformity, Beijing 100730, China; 3Medical Research Center of Orthopedics, Chinese Academy of Medical Sciences, Beijing 100730, China; 4Department of Orthopedic Surgery, 5Department of Central Laboratory, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing 100730, China Contributions: (I) Conception and design: W Tian, N Wu, Z Wu, S Zhong; (II) Administrative support: All authors; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: Y Huang; (V) Data analysis and interpretation: L Sun; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Wen Tian. Hand Surgery Department, Beijing Jishuitan Hospital, Beijing 100035, China. Email: [email protected]. Abstract: Congenital upper limb anomalies (CULA) are a common birth defect and a significant portion of complicated syndromic anomalies have upper limb involvement. Mostly the mortality of babies with CULA can be attributed to associated anomalies. The cause of the majority of syndromic CULA was unknown until recently. Advances in genetic and genomic technologies have unraveled the genetic basis of many syndromes- associated CULA, while at the same time highlighting the extreme heterogeneity in CULA genetics. Discoveries regarding biological pathways and syndromic CULA provide insights into the limb development and bring a better understanding of the pathogenesis of CULA. -

Genes in Eyecare Geneseyedoc 3 W.M
Genes in Eyecare geneseyedoc 3 W.M. Lyle and T.D. Williams 15 Mar 04 This information has been gathered from several sources; however, the principal source is V. A. McKusick’s Mendelian Inheritance in Man on CD-ROM. Baltimore, Johns Hopkins University Press, 1998. Other sources include McKusick’s, Mendelian Inheritance in Man. Catalogs of Human Genes and Genetic Disorders. Baltimore. Johns Hopkins University Press 1998 (12th edition). http://www.ncbi.nlm.nih.gov/Omim See also S.P.Daiger, L.S. Sullivan, and B.J.F. Rossiter Ret Net http://www.sph.uth.tmc.edu/Retnet disease.htm/. Also E.I. Traboulsi’s, Genetic Diseases of the Eye, New York, Oxford University Press, 1998. And Genetics in Primary Eyecare and Clinical Medicine by M.R. Seashore and R.S.Wappner, Appleton and Lange 1996. M. Ridley’s book Genome published in 2000 by Perennial provides additional information. Ridley estimates that we have 60,000 to 80,000 genes. See also R.M. Henig’s book The Monk in the Garden: The Lost and Found Genius of Gregor Mendel, published by Houghton Mifflin in 2001 which tells about the Father of Genetics. The 3rd edition of F. H. Roy’s book Ocular Syndromes and Systemic Diseases published by Lippincott Williams & Wilkins in 2002 facilitates differential diagnosis. Additional information is provided in D. Pavan-Langston’s Manual of Ocular Diagnosis and Therapy (5th edition) published by Lippincott Williams & Wilkins in 2002. M.A. Foote wrote Basic Human Genetics for Medical Writers in the AMWA Journal 2002;17:7-17. A compilation such as this might suggest that one gene = one disease. -

RD-Action Matchmaker – Summary of Disease Expertise Recorded Under
Summary of disease expertise recorded via RD-ACTION Matchmaker under each Thematic Grouping and EURORDIS Members’ Thematic Grouping Thematic Reported expertise of those completing the EURORDIS Member perspectives on Grouping matchmaker under each heading Grouping RD Thematically Rare Bone Achondroplasia/Hypochondroplasia Achondroplasia Amelia skeletal dysplasia’s including Achondroplasia/Growth hormone cleidocranial dysostosis, arthrogryposis deficiency/MPS/Turner Brachydactyly chondrodysplasia punctate Fibrous dysplasia of bone Collagenopathy and oncologic disease such as Fibrodysplasia ossificans progressive Li-Fraumeni syndrome Osteogenesis imperfecta Congenital hand and fore-foot conditions Sterno Costo Clavicular Hyperostosis Disorders of Sex Development Duchenne Muscular Dystrophy Ehlers –Danlos syndrome Fibrodysplasia Ossificans Progressiva Growth disorders Hypoparathyroidism Hypophosphatemic rickets & Nutritional Rickets Hypophosphatasia Jeune’s syndrome Limb reduction defects Madelung disease Metabolic Osteoporosis Multiple Hereditary Exostoses Osteogenesis imperfecta Osteoporosis Paediatric Osteoporosis Paget’s disease Phocomelia Pseudohypoparathyroidism Radial dysplasia Skeletal dysplasia Thanatophoric dwarfism Ulna dysplasia Rare Cancer and Adrenocortical tumours Acute monoblastic leukaemia Tumours Carcinoid tumours Brain tumour Craniopharyngioma Colon cancer, familial nonpolyposis Embryonal tumours of CNS Craniopharyngioma Ependymoma Desmoid disease Epithelial thymic tumours in -

Level Estimates of Maternal Smoking and Nicotine Replacement Therapy During Pregnancy
Using primary care data to assess population- level estimates of maternal smoking and nicotine replacement therapy during pregnancy Nafeesa Nooruddin Dhalwani BSc MSc Thesis submitted to the University of Nottingham for the degree of Doctor of Philosophy November 2014 ABSTRACT Background: Smoking in pregnancy is the most significant preventable cause of poor health outcomes for women and their babies and, therefore, is a major public health concern. In the UK there is a wide range of interventions and support for pregnant women who want to quit. One of these is nicotine replacement therapy (NRT) which has been widely available for retail purchase and prescribing to pregnant women since 2005. However, measures of NRT prescribing in pregnant women are scarce. These measures are vital to assess its usefulness in smoking cessation during pregnancy at a population level. Furthermore, evidence of NRT safety in pregnancy for the mother and child’s health so far is nebulous, with existing studies being small or using retrospectively reported exposures. Aims and Objectives: The main aim of this work was to assess population- level estimates of maternal smoking and NRT prescribing in pregnancy and the safety of NRT for both the mother and the child in the UK. Currently, the only population-level data on UK maternal smoking are from repeated cross-sectional surveys or routinely collected maternity data during pregnancy or at delivery. These obtain information at one point in time, and there are no population-level data on NRT use available. As a novel approach, therefore, this thesis used the routinely collected primary care data that are currently available for approximately 6% of the UK population and provide longitudinal/prospectively recorded information throughout pregnancy. -

Appendix A: Organisation of a Craniofacial Unit
Appendix A: Organisation of a Craniofacial Unit The requirements of patients with craniofacial abnormalities are very complex and demand a multidisciplinary approach. Many body systems are affected, and every detail of patient management has to be given due attention. Care begins at birth and continues until the patient and his family have been relieved of the burden of the anomaly. A team is needed, capable of delivering expert patient care, and representative of all the relevant disciplines. Data, in the form of histories, physical examinations, and special investigations, are needed in planning treatment, and such data should be used to the maximum scientific effect, to improve present methods of management, still far from satisfactory, and to expand knowledge of the biology of cranial growth and its disorders. Craniofacial Units Sporadic craniofacial procedures performed by a surgeon on an irregular basis invite disaster. Tessier (1971a) estimated that each craniofacial centre should serve a population of 10 to 20 million people, provided that the team performed only craniofacial surgery and treated at least 50 new cases annually. As a consequence of Tessier's example and teaching there are now centres of acknowledged excellence in Paris and Nancy, attracting patients not only from France but also from North Africa and elsewhere. In North America there are now important craniofacial centres in Philadelphia, New York, Boston, Toronto, and Mexico City. Munro (1975) proposed that North America should be divided into seven regions, six for the United States and one for Canada, each serving populations of 20 to 40 million people. He believed that such centres would allow a concentration of multidisciplinary skills and accumulation of experience in the treatment of craniofacial anomalies. -

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -

Hand Surgery
Plastic & reconstructive surgery د.ﻣﺤﻤﺪ ﺟﺎﺳﻢ ﻣﺤﻤﺪ Lec 2 اﺧﺗﺻﺎص اﻟﺟراﺣﺔ اﻟﺗﻘوﯾﻣﯾﺔ 5TH Stage HAND SURGERY Congenital hand abnormalities SWANSON CLASSIFICATION OF CONGENITAL UPPER LIMB ABNORMALITIES I. Failure of Formation of Parts A. Transverse: truncated limb B. Longitudinal: Radial club hand (Preaxial Deficiency) Cleft hand (Central Deficiency) Ulnar club hand(postaxial deficiency) Phocomelia (Intercalary Deficiency) II. Failure of Differentiation or Separation of Parts A. Symphalangism B. Syndactyly C. Contracture: Arthrogryposis Trigger finger Clasped thumb Camptodactyly Clinodactyly III. Duplication: Polydactyly IV. Overgrowth: Macrodactyly V. Undergrowth: Thumb hypoplasia VI. Congenital Constriction Ring Syndrome VII. Generalized Skeletal Abnormalities and Syndromes. Preaxial Deficiency: Radial Club Hand: They are typically sporadic and unilateral, more common in males, and more common on the right side Radial dysplasias are commonly associated with syndromes including Fanconi anemia, thrombocytopenia absent radius (TAR) syndrome, Holt-Oram syndrome (associated with cardiac septal defects), and VATER(vertebral abnormality, anal imperforation, tracheoesophageal fistula, radial, or renal anomalies. The clinical manifestation of radial club hand is a shortened forearm with radial deviation at the wrist. The pathology affects all structures on the preaxial side of the limb: skeleton, musculotendinous units, joints, neurovascular structures, and soft tissue. CLASSIFICATION OF RADIAL DYSPLASIA I-Short radius II- Hypoplastic radius III- Partial absence of radius IV- Total absence of radius Management Type I mild type II dysplasia may only require splinting . Centralization or radialization of wrist with tendon transfer are the treatments of choice in severe type II, and in types III and IV; repair should be performed at 6 to 12 months of age. In pt with absent thumb, pollicization should be done after 6 month from 1st operation. -

University of Washington Orthopaedics & Sports Medicine
Discoveries 2018 University of Washington Orthopaedics & Sports Medicine University of Washington Department of Orthopaedics and Sports Medicine Discoveries 2018 Department of Orthopaedics and Sports Medicine University of Washington Seattle, WA 98195 EDITOR-IN-CHIEF: Howard A. Chansky, MD [email protected] ASSISTANT EDITORS: Christopher H. Allan, MD [email protected] Stephen A. Kennedy, MD, FRCSC [email protected] Adam A. Sassoon, MD, MS [email protected] MANAGING EDITOR: Fred Westerberg [email protected] Front Cover Illustration: Angie Kennedy, MSc, is a Seattle-based mixed media artist. She specializes in custom collage pieces that use mementos and artifacts to celebrate people and special life events. She drew on her experience as a former scientific researcher to create this collage of images from the pages of the current publication. The ‘W’ in the background is a nod to the University of Washington with an overlay of the current imagery arranged in an abstract assemblage. For more information www.americanheavyweight.com A pdf of this publication is available at our website: www.orthop.washington.edu. Permission Requests: All inquiries should be directed to the Managing Editor, University of Washington, Department of Orthopaedics and Sports Medicine, 1959 NE Pacific Street, Box 356500, Seattle, WA 98195-6500, or at the email address above. Contents 1 Foreword 2 From The Assistant Editors: The Modern Art of Musculoskeletal Research, Education, and Clinical Care 3 2018 Distinguished Alumnus, David J. Belfie, MD 4 New Faculty 6 Department of Orthopaedics and Sports Medicine Faculty 12 Visiting Lecturers Validation of a Rabbit Model of Trauma-Induced 14 Brandon J. Ausk, PhD, Philippe Huber, BS, Heterotopic Ossification Ted S. -
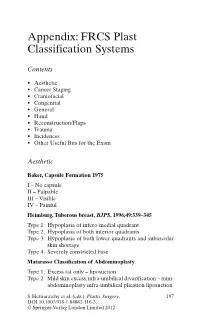
Appendix: FRCS Plast Classification Systems
Appendix: FRCS Plast Classification Systems Contents • Aesthetic • Cancer Staging • Craniofacial • Congenital • General • Hand • Reconstruction/Flaps • Trauma • Incidences • Other Useful Bits for the Exam Aesthetic Baker, Capsule Formation 1975 I – No capsule II – Palpable III – Visible IV – Painful Heimburg, Tuberous breast, BJPS , 1996;49:339–345 Type 1: Hypoplasia of infero-medial quadrant Type 2: Hypoplasia of both inferior quadrants Type 3: Hypoplasia of both lower quadrants and subareolar skin shortage Type 4: Severely constricted base Matarasso Classification of Abdominoplasty Type 1: Excess fat only – liposuction Type 2: Mild skin excess, infra-umbilical divarification – mini- abdominoplasty infra-umbilical plication liposuction S. Hettiaratchy et al. (eds.), Plastic Surgery, 197 DOI 10.1007/978-1-84882-116-3, © Springer-Verlag London Limited 2012 198 Appendix: FRCS Plast Classification Systems Type 3: Moderate skin excess, infra and superior divarifica- tion – As above Type 4: Severe skin excess – Standard abdominoplasty with plication and liposuction Paysk zones around an expander Inner zone: Fibrin layer with macrophages Central zone: Fibroblasts and myofibroblasts Transitional zone: Loose collagen Outer zone: Blood vessels and collagen Regnault classification of ptosis 1st degree: Nipples at or above IMF 2nd degree: Nipples below IMF but above most dependant portion of the breast 3rd degree: Nipples below the most dependant portion of the breast • Pseudo-ptosis – where the majority of the breast mound lies below the IMF but -

Polydactyly of the Hand
A Review Paper Polydactyly of the Hand Katherine C. Faust, MD, Tara Kimbrough, BS, Jean Evans Oakes, MD, J. Ollie Edmunds, MD, and Donald C. Faust, MD cleft lip/palate, and spina bifida. Thumb duplication occurs in Abstract 0.08 to 1.4 per 1000 live births and is more common in Ameri- Polydactyly is considered either the most or second can Indians and Asians than in other races.5,10 It occurs in a most (after syndactyly) common congenital hand ab- male-to-female ratio of 2.5 to 1 and is most often unilateral.5 normality. Polydactyly is not simply a duplication; the Postaxial polydactyly is predominant in black infants; it is most anatomy is abnormal with hypoplastic structures, ab- often inherited in an autosomal dominant fashion, if isolated, 1 normally contoured joints, and anomalous tendon and or in an autosomal recessive pattern, if syndromic. A prospec- ligament insertions. There are many ways to classify tive San Diego study of 11,161 newborns found postaxial type polydactyly, and surgical options range from simple B polydactyly in 1 per 531 live births (1 per 143 black infants, excision to complicated bone, ligament, and tendon 1 per 1339 white infants); 76% of cases were bilateral, and 3 realignments. The prevalence of polydactyly makes it 86% had a positive family history. In patients of non-African descent, it is associated with anomalies in other organs. Central important for orthopedic surgeons to understand the duplication is rare and often autosomal dominant.5,10 basic tenets of the abnormality. Genetics and Development As early as 1896, the heritability of polydactyly was noted.11 As olydactyly is the presence of extra digits. -

Hemimegalencephaly with Bannayan-Riley-Ruvalcaba Syndrome
Journal Identification = EPD Article Identification = 0954 Date: February 15, 2018 Time: 10:35 am Original article Epileptic Disord 2018; 20 (1): 30-4 Hemimegalencephaly with Bannayan-Riley-Ruvalcaba syndrome Ryan Ghusayni 1, Monisha Sachdev 1, William Gallentine 1, Mohamad A Mikati 1,a, Marie T McDonald 2,a 1 Division of Pediatric Neurology, Department of Pediatrics, Duke University, Durham 2 Division of Medical Genetics, Department of Pediatrics, Duke University, Durham, USA a Authors contributed equally Received August 30, 2017; Accepted January 09, 2018 ABSTRACT – Hemimegalencephaly is known to occur in Proteus syn- drome, but has not been reported, to our knowledge, in the other PTEN mutation-related syndrome of Bannayan-Riley-Ruvalcaba. Here, we report a patient with Bannayan-Riley-Ruvalcaba syndrome who also had hemimegalencephaly and in whom the hemimegalencephaly was evident well before presentation of the characteristic manifestations of Bannayan- Riley-Ruvalcaba syndrome. An 11-year-old boy developed drug-resistant focal seizures on the fifth day of life. MRI revealed left hemimegalencephaly. He later showed macrocephaly,developmental delay,athetotic quadriplegic cerebral palsy, and neuromuscular scoliosis. Freckling of the penis, which is characteristic of Bannayan-Riley-Ruvalcaba syndrome, was not present at birth but was observed at 9 years of age. Gene analysis revealed a c.510 T>G PTEN mutation. This patient and his other affected family members, his father and two siblings, were started on the tumour screening procedures recommended for patients with PTEN mutations. This case highlights the importance of early screening for PTEN mutations in cases of hemimegalen- cephaly not otherwise explained by another disorder, even in the absence of signs of Proteus syndrome or the full manifestations of Bannayan-Riley Ruvalcaba syndrome.