Congenital Differences of the Upper Extremity: Classifi Cation and Treatment Principles Moon Sang Chung, MD
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sara Aghamohammadi, M.D
Sara Aghamohammadi, M.D. Philosophy of Care It is a privilege to care for children and their families during the time of their critical illness. I strive to incorporate the science and art of medicine in my everyday practice such that each child and family receives the best medical care in a supportive and respectful environment. Having grown up in the San Joaquin Valley, I am honored to join UC Davis Children's Hospital's team and contribute to the well-being of our community's children. Clinical Interests Dr. Aghamohammadi has always had a passion for education, she enjoys teaching principles of medicine, pediatrics, and critical care to medical students, residents, and nurses alike. Her clinical interests include standardization of practice in the PICU through the use of protocols. Her team has successfully implemented a sedation and analgesia protocol in the PICU, and she helped develop the high-flow nasal cannula protocol for bronchiolitis. Additionally, she has been involved in the development of pediatric pain order sets and is part of a multi-disciplinary team to address acute and chronic pain in pediatric patients. Research/Academic Interests Dr. Aghamohammadi has been passionate about Physician Health and Well-being and heads the Wellness Committee for the Department of Pediatrics. Additionally, she is a part of the Department Wellness Champions for the UC Davis Health System and has given presentations on the importance of Physician Wellness. After completing training in Physician Health and Well-being, she now serves as a mentor for the Train-the-Trainer Physician Health and Well-being Fellowship. -

Neonatal Orthopaedics
NEONATAL ORTHOPAEDICS NEONATAL ORTHOPAEDICS Second Edition N De Mazumder MBBS MS Ex-Professor and Head Department of Orthopaedics Ramakrishna Mission Seva Pratishthan Vivekananda Institute of Medical Sciences Kolkata, West Bengal, India Visiting Surgeon Department of Orthopaedics Chittaranjan Sishu Sadan Kolkata, West Bengal, India Ex-President West Bengal Orthopaedic Association (A Chapter of Indian Orthopaedic Association) Kolkata, West Bengal, India Consultant Orthopaedic Surgeon Park Children’s Centre Kolkata, West Bengal, India Foreword AK Das ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD. New Delhi • London • Philadelphia • Panama (021)66485438 66485457 www.ketabpezeshki.com ® Jaypee Brothers Medical Publishers (P) Ltd. Headquarters Jaypee Brothers Medical Publishers (P) Ltd. 4838/24, Ansari Road, Daryaganj New Delhi 110 002, India Phone: +91-11-43574357 Fax: +91-11-43574314 Email: [email protected] Overseas Offices J.P. Medical Ltd. Jaypee-Highlights Medical Publishers Inc. Jaypee Brothers Medical Publishers Ltd. 83, Victoria Street, London City of Knowledge, Bld. 237, Clayton The Bourse SW1H 0HW (UK) Panama City, Panama 111, South Independence Mall East Phone: +44-2031708910 Phone: +507-301-0496 Suite 835, Philadelphia, PA 19106, USA Fax: +02-03-0086180 Fax: +507-301-0499 Phone: +267-519-9789 Email: [email protected] Email: [email protected] Email: [email protected] Jaypee Brothers Medical Publishers (P) Ltd. Jaypee Brothers Medical Publishers (P) Ltd. 17/1-B, Babar Road, Block-B, Shaymali Shorakhute, Kathmandu Mohammadpur, Dhaka-1207 Nepal Bangladesh Phone: +00977-9841528578 Mobile: +08801912003485 Email: [email protected] Email: [email protected] Website: www.jaypeebrothers.com Website: www.jaypeedigital.com © 2013, Jaypee Brothers Medical Publishers All rights reserved. No part of this book may be reproduced in any form or by any means without the prior permission of the publisher. -

Genetic Causes of Congenital Malformation in India
International Journal of Human Genetics ISSN: 0972-3757 (Print) (Online) Journal homepage: http://www.tandfonline.com/loi/rhug20 Genetic Causes of Congenital Malformation in India Geeta Talukder & Archana Sharma To cite this article: Geeta Talukder & Archana Sharma (2006) Genetic Causes of Congenital Malformation in India, International Journal of Human Genetics, 6:1, 15-25, DOI: 10.1080/09723757.2006.11885942 To link to this article: https://doi.org/10.1080/09723757.2006.11885942 Published online: 04 Sep 2017. Submit your article to this journal Article views: 2 View related articles Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=rhug20 © Kamla-Raj 2006 Int J Hum Genet, 6(1): 15-25 (2006) Genetic Causes of Congenital Malformation in India Geeta Talukder1 and Archana Sharma2 1. Vivekananda Institute of Medical Sciences, 99 Sarat Bose Road, Kolkata 700 026, West Bengal, India E-mail: geetatalukdar @hotmail.com 2. CAS in Cell & Chromosome Research, Department of Botany, University College of Science, 35 Ballygunj Circular Road, Kolkata 700 019, West Bengal, India KEYWORDS Congenital malformations; neonates; stillbirths; prenatal detection; prevention ABSTRACT Congenital malformations are a major cause of death of neonates in India where prenatal detection and treatment are not adequate in many hospitals and health centers. Incidence is specially high in stillbirths. It is not realized that genetic causes - chromosomal, single gene and polygenic - are the main causes of many congenital defects and early detection and prevention should be essential to make the small family norm a success. INTRODUCTION Recently Patel and Adhia (2005) detected major malformations in 7.92% of 17653 births and Phenotypic changes of genetic diseases at were able to attribute chromosomal cause to birth include congenital malformations in 4%,polygenic to 45.1% and total genetic chromosomes and single gene defects. -

Congenital Transverse Defects of Limbs and Digits* ('Intrauterine Amputation') by H
Arch Dis Child: first published as 10.1136/adc.37.193.263 on 1 June 1962. Downloaded from CONGENITAL TRANSVERSE DEFECTS OF LIMBS AND DIGITS* ('INTRAUTERINE AMPUTATION') BY H. G. KOHLER From the Department ofPathology, Birmingham Maternity Hospital (RECEIVED FOR PUBLICATION OCTOBER 23, 1961) Intrauterine amputation of the extremities is an Thomas Bartholin of Copenhagen (1616-1680) uncommon and peculiar congenital deformity which is said to be the first to mention a congenitally is characterized by the absence of one or more distal deficient extremity. He lived at the very threshold limb portions. Termination of the proximal part of the modern scientific era and belonged to a family is usually abrupt and bears no apparent relation to well known for their contributions to medicine and anatomical boundaries. The term 'amputation' biology: Thomas Bartholin's son, Caspar Secundus, suggests separation, by mechanical force, of a limb was the first to describe the vestibulo-vaginal glands. already formed rather than a failure of develop- Thomas was a man of great learning and wide ment, but such a view of the pathogenesis of this interests (Rhodes, 1957). His textbook on anatomy abnormality is far from universally accepted. It was translated into English and used widely for a would probably be better to use a neutral term such long time. Bartholin's descriptions of monsters, as 'transverse defects', but for the conservatism of however, tend to be more imaginative than factual medical nomenclature. (Hendry and Kohler, 1956). The essay which copyright. Circular grooves around the digits or limbs, and contains a reference to limb defects bears the title similar soft tissue defects, also known as ring con- 'Gravidarum Imaginatio' and there, in passing, he strictions, are seen usually in association with 'intra- tells us of a deformed male infant with only one uterine amputation', but also on their own. -

Hand Surgery
Plastic & reconstructive surgery د.ﻣﺤﻤﺪ ﺟﺎﺳﻢ ﻣﺤﻤﺪ Lec 2 اﺧﺗﺻﺎص اﻟﺟراﺣﺔ اﻟﺗﻘوﯾﻣﯾﺔ 5TH Stage HAND SURGERY Congenital hand abnormalities SWANSON CLASSIFICATION OF CONGENITAL UPPER LIMB ABNORMALITIES I. Failure of Formation of Parts A. Transverse: truncated limb B. Longitudinal: Radial club hand (Preaxial Deficiency) Cleft hand (Central Deficiency) Ulnar club hand(postaxial deficiency) Phocomelia (Intercalary Deficiency) II. Failure of Differentiation or Separation of Parts A. Symphalangism B. Syndactyly C. Contracture: Arthrogryposis Trigger finger Clasped thumb Camptodactyly Clinodactyly III. Duplication: Polydactyly IV. Overgrowth: Macrodactyly V. Undergrowth: Thumb hypoplasia VI. Congenital Constriction Ring Syndrome VII. Generalized Skeletal Abnormalities and Syndromes. Preaxial Deficiency: Radial Club Hand: They are typically sporadic and unilateral, more common in males, and more common on the right side Radial dysplasias are commonly associated with syndromes including Fanconi anemia, thrombocytopenia absent radius (TAR) syndrome, Holt-Oram syndrome (associated with cardiac septal defects), and VATER(vertebral abnormality, anal imperforation, tracheoesophageal fistula, radial, or renal anomalies. The clinical manifestation of radial club hand is a shortened forearm with radial deviation at the wrist. The pathology affects all structures on the preaxial side of the limb: skeleton, musculotendinous units, joints, neurovascular structures, and soft tissue. CLASSIFICATION OF RADIAL DYSPLASIA I-Short radius II- Hypoplastic radius III- Partial absence of radius IV- Total absence of radius Management Type I mild type II dysplasia may only require splinting . Centralization or radialization of wrist with tendon transfer are the treatments of choice in severe type II, and in types III and IV; repair should be performed at 6 to 12 months of age. In pt with absent thumb, pollicization should be done after 6 month from 1st operation. -

GUIDE to ADAPTED SWIMMING CLASSIFICATIONS Swimming Is
GUIDE TO ADAPTED SWIMMING CLASSIFICATIONS Swimming is the only sport that combines the conditions of limb loss, cerebral palsy (coordination and movement restrictions), spinal cord injury (weakness or paralysis involving any combination of the limbs) and other disabilities (such as Dwarfism (little people); major joint restriction conditions) across classes. Classes 1-10 – are allocated to swimmers with a physical disability Classes 11-13 – are allocated to swimmers with a visual disability Class 14 – is allocated to swimmers with an intellectual disability The Prefix S to the Class denotes the class for Freestyle, Backstroke and Butterfly The Prefix SB to the class denotes the class for Breaststroke The Prefix SM to the class denotes the class for Individual Medley. The range is from the swimmers with severe disability (S1, SB1, SM1) to those with the minimal disability (S10, SB9, SM10) In any one class some swimmers may start with a dive or in the water depending on their condition. This is factored in when classifying the athlete. The examples are only a guide – some conditions not mentioned may also fit the following classes. Locomotor Impaired (S1-S10): S1: Generally persons with complete spinal cord injuries below C4-C5 or cerebral palsy characterized by severe quadriplegia. Unable to catch the water. Severely limited propulsion from the arms due to muscle weakness, restricted range of motion or uncoordinated movements. No trunk control. No functional leg movements and significant leg drag. Assisted water start. Ordinarily uses the backstroke because of an inability to turn the head to breathe when swimming freestyle. S2: Generally persons with complete spinal cord injuries below C6-C7 or similar musculoskeletal impairment or cerebral palsy characterized by severe quadriplegia. -

University of Washington Orthopaedics & Sports Medicine
Discoveries 2018 University of Washington Orthopaedics & Sports Medicine University of Washington Department of Orthopaedics and Sports Medicine Discoveries 2018 Department of Orthopaedics and Sports Medicine University of Washington Seattle, WA 98195 EDITOR-IN-CHIEF: Howard A. Chansky, MD [email protected] ASSISTANT EDITORS: Christopher H. Allan, MD [email protected] Stephen A. Kennedy, MD, FRCSC [email protected] Adam A. Sassoon, MD, MS [email protected] MANAGING EDITOR: Fred Westerberg [email protected] Front Cover Illustration: Angie Kennedy, MSc, is a Seattle-based mixed media artist. She specializes in custom collage pieces that use mementos and artifacts to celebrate people and special life events. She drew on her experience as a former scientific researcher to create this collage of images from the pages of the current publication. The ‘W’ in the background is a nod to the University of Washington with an overlay of the current imagery arranged in an abstract assemblage. For more information www.americanheavyweight.com A pdf of this publication is available at our website: www.orthop.washington.edu. Permission Requests: All inquiries should be directed to the Managing Editor, University of Washington, Department of Orthopaedics and Sports Medicine, 1959 NE Pacific Street, Box 356500, Seattle, WA 98195-6500, or at the email address above. Contents 1 Foreword 2 From The Assistant Editors: The Modern Art of Musculoskeletal Research, Education, and Clinical Care 3 2018 Distinguished Alumnus, David J. Belfie, MD 4 New Faculty 6 Department of Orthopaedics and Sports Medicine Faculty 12 Visiting Lecturers Validation of a Rabbit Model of Trauma-Induced 14 Brandon J. Ausk, PhD, Philippe Huber, BS, Heterotopic Ossification Ted S. -

349 D.R. Laub Jr. (Ed.), Congenital Anomalies of the Upper
Index A dermatological anomalies , 182 Abductor digiti minimi (ADM) transfer , 102–103 skeletal abnormalities , 182 Abductor pollicis brevis (APB) , 186–187 upper extremity anomalies , 182, 183 ABS. See Amniotic band syndrome (ABS) visceral anomalies , 182 Achondroplasia defi nition of , 179 classifi cation/characterization , 338 description , 32, 33 defi nition of , 337–338 epidemiology of , 181 genetics , 338 genetics and embryology management , 338 molecular etiology , 180 Acrocephalosyndactyly syndrome , 32, 33, 179 prenatal diagnosis , 180–181 Acrosyndactyly repair, ABS , 300–302 molecular basis of , 180 Adactylic group IV symbrachydactyly , 129, 131 postoperative care and complications , 187 Al-Awadi syndrome , 154 treatment Amniotic band syndrome (ABS) APB release , 186–187 acrosyndactyly repair , 300–302 border digits syndactylies , 184 anesthesia concerns of fi rst web space release , 186 induction and maintenance of anesthesia , 43 patient age , 183 postoperative concerns , 43 secondary revisions , 187 preoperative preparation , 42–43 symphalangism , 184 classifi cation , 298 syndactyly ( see Syndactyly) clinical presentation thumb radial clinodactyly , 186–187 acrosyndactyly , 297–298 type II apert hand , 187–188 digital malformation , 297 Apical ectodermal ridge (AER) , 3–5 distal skeletal bones tapering , 297–298 Arthrogryposis , 210 hand deformity , 297 classic arthrogryposis , 305–306, 308 complications , 302 classifi cation , 305, 306 constriction band release defi nition of , 229, 230, 305 Upton’s technique , 299, 301 de-rotation osteotomy, shoulder , 308, 309 z-plasty , 299–300 distal , 230–231 ( see Distal arthrogryposis) diagnosis of , 296 elbow treatment digital hypoplasia reconstruction , 302 muscle transfers , 310–311 etiology of , 295–296 nonoperative management , 308 preoperative considerations , 299 posterior elbow capsular release , 309 treatment , 299 radial head dislocations , 311 Amniotic constriction band syndrome. -
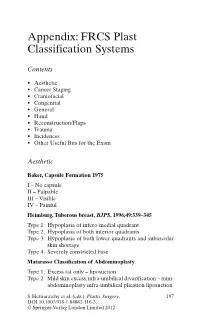
Appendix: FRCS Plast Classification Systems
Appendix: FRCS Plast Classification Systems Contents • Aesthetic • Cancer Staging • Craniofacial • Congenital • General • Hand • Reconstruction/Flaps • Trauma • Incidences • Other Useful Bits for the Exam Aesthetic Baker, Capsule Formation 1975 I – No capsule II – Palpable III – Visible IV – Painful Heimburg, Tuberous breast, BJPS , 1996;49:339–345 Type 1: Hypoplasia of infero-medial quadrant Type 2: Hypoplasia of both inferior quadrants Type 3: Hypoplasia of both lower quadrants and subareolar skin shortage Type 4: Severely constricted base Matarasso Classification of Abdominoplasty Type 1: Excess fat only – liposuction Type 2: Mild skin excess, infra-umbilical divarification – mini- abdominoplasty infra-umbilical plication liposuction S. Hettiaratchy et al. (eds.), Plastic Surgery, 197 DOI 10.1007/978-1-84882-116-3, © Springer-Verlag London Limited 2012 198 Appendix: FRCS Plast Classification Systems Type 3: Moderate skin excess, infra and superior divarifica- tion – As above Type 4: Severe skin excess – Standard abdominoplasty with plication and liposuction Paysk zones around an expander Inner zone: Fibrin layer with macrophages Central zone: Fibroblasts and myofibroblasts Transitional zone: Loose collagen Outer zone: Blood vessels and collagen Regnault classification of ptosis 1st degree: Nipples at or above IMF 2nd degree: Nipples below IMF but above most dependant portion of the breast 3rd degree: Nipples below the most dependant portion of the breast • Pseudo-ptosis – where the majority of the breast mound lies below the IMF but -

Polydactyly of the Hand
A Review Paper Polydactyly of the Hand Katherine C. Faust, MD, Tara Kimbrough, BS, Jean Evans Oakes, MD, J. Ollie Edmunds, MD, and Donald C. Faust, MD cleft lip/palate, and spina bifida. Thumb duplication occurs in Abstract 0.08 to 1.4 per 1000 live births and is more common in Ameri- Polydactyly is considered either the most or second can Indians and Asians than in other races.5,10 It occurs in a most (after syndactyly) common congenital hand ab- male-to-female ratio of 2.5 to 1 and is most often unilateral.5 normality. Polydactyly is not simply a duplication; the Postaxial polydactyly is predominant in black infants; it is most anatomy is abnormal with hypoplastic structures, ab- often inherited in an autosomal dominant fashion, if isolated, 1 normally contoured joints, and anomalous tendon and or in an autosomal recessive pattern, if syndromic. A prospec- ligament insertions. There are many ways to classify tive San Diego study of 11,161 newborns found postaxial type polydactyly, and surgical options range from simple B polydactyly in 1 per 531 live births (1 per 143 black infants, excision to complicated bone, ligament, and tendon 1 per 1339 white infants); 76% of cases were bilateral, and 3 realignments. The prevalence of polydactyly makes it 86% had a positive family history. In patients of non-African descent, it is associated with anomalies in other organs. Central important for orthopedic surgeons to understand the duplication is rare and often autosomal dominant.5,10 basic tenets of the abnormality. Genetics and Development As early as 1896, the heritability of polydactyly was noted.11 As olydactyly is the presence of extra digits. -

The Spine, Trauma and Infection
Develop. Med. Child Neurol. 1982, 24. 202-218 Review Article Robert N. Hensinger Eric T. Jones Developmental Orthopaedics. 11: The Spine, Trauma and Infection Torticollis Congenital muscular torticollis is Torticollis, or wryneck, is a common believed to result from local trauma to the clinical sign in a wide variety of childhood soft tissues of the neck during delivery. illnesses. When recognized at or soon after Birth records of these children birth, the usual cause is congenital demonstrate a preponderance of breech or muscular torticollis. However, difficult forceps deliveries, or primiparous roentgenograms of the cervical spine births', '. A common misconception is that should be obtained to exclude other less the neck is contused during delivery and common congenital conditions, such as the the resultant hematoma leads to fibrosis fixed or bony torticollis associated with and contracture. However, experimental Klippel-Feil syndrome and/or anomalies of the atlanto-axial articulation (Table I). TABLE I Congenital muscular torticollis is Differential diagnosis of torticollis usually discovered in the first six to eight weeks of life. If the infant is examined Congenital Congenital muscular torticollis within the first month of life, commonly a Klippel-Feil syndrome mass or 'tumor' is palpable in the neck' Basilar impressions Atlanto-occipital fusion (Fig. 1). Generally there is a non-tender, Pterygium colli (skin webs) soft enlargement which is mobile beneath Odontoid anomalies the skin and attached to or located within Neurological the body of the sternocleidomastoid Ocular dysfunction muscle. The mass obtains maximum size Syringomyelia Spinal-cord or cerebellar tumors (posterior within the first month and then gradually fossa) regresses. -

Appendix 3.1 Birth Defects Descriptions for NBDPN Core, Recommended, and Extended Conditions Updated March 2017
Appendix 3.1 Birth Defects Descriptions for NBDPN Core, Recommended, and Extended Conditions Updated March 2017 Participating members of the Birth Defects Definitions Group: Lorenzo Botto (UT) John Carey (UT) Cynthia Cassell (CDC) Tiffany Colarusso (CDC) Janet Cragan (CDC) Marcia Feldkamp (UT) Jamie Frias (CDC) Angela Lin (MA) Cara Mai (CDC) Richard Olney (CDC) Carol Stanton (CO) Csaba Siffel (GA) Table of Contents LIST OF BIRTH DEFECTS ................................................................................................................................................. I DETAILED DESCRIPTIONS OF BIRTH DEFECTS ...................................................................................................... 1 FORMAT FOR BIRTH DEFECT DESCRIPTIONS ................................................................................................................................. 1 CENTRAL NERVOUS SYSTEM ....................................................................................................................................... 2 ANENCEPHALY ........................................................................................................................................................................ 2 ENCEPHALOCELE ..................................................................................................................................................................... 3 HOLOPROSENCEPHALY.............................................................................................................................................................