AGING and AMPUTATION Harold W
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neonatal Orthopaedics
NEONATAL ORTHOPAEDICS NEONATAL ORTHOPAEDICS Second Edition N De Mazumder MBBS MS Ex-Professor and Head Department of Orthopaedics Ramakrishna Mission Seva Pratishthan Vivekananda Institute of Medical Sciences Kolkata, West Bengal, India Visiting Surgeon Department of Orthopaedics Chittaranjan Sishu Sadan Kolkata, West Bengal, India Ex-President West Bengal Orthopaedic Association (A Chapter of Indian Orthopaedic Association) Kolkata, West Bengal, India Consultant Orthopaedic Surgeon Park Children’s Centre Kolkata, West Bengal, India Foreword AK Das ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD. New Delhi • London • Philadelphia • Panama (021)66485438 66485457 www.ketabpezeshki.com ® Jaypee Brothers Medical Publishers (P) Ltd. Headquarters Jaypee Brothers Medical Publishers (P) Ltd. 4838/24, Ansari Road, Daryaganj New Delhi 110 002, India Phone: +91-11-43574357 Fax: +91-11-43574314 Email: [email protected] Overseas Offices J.P. Medical Ltd. Jaypee-Highlights Medical Publishers Inc. Jaypee Brothers Medical Publishers Ltd. 83, Victoria Street, London City of Knowledge, Bld. 237, Clayton The Bourse SW1H 0HW (UK) Panama City, Panama 111, South Independence Mall East Phone: +44-2031708910 Phone: +507-301-0496 Suite 835, Philadelphia, PA 19106, USA Fax: +02-03-0086180 Fax: +507-301-0499 Phone: +267-519-9789 Email: [email protected] Email: [email protected] Email: [email protected] Jaypee Brothers Medical Publishers (P) Ltd. Jaypee Brothers Medical Publishers (P) Ltd. 17/1-B, Babar Road, Block-B, Shaymali Shorakhute, Kathmandu Mohammadpur, Dhaka-1207 Nepal Bangladesh Phone: +00977-9841528578 Mobile: +08801912003485 Email: [email protected] Email: [email protected] Website: www.jaypeebrothers.com Website: www.jaypeedigital.com © 2013, Jaypee Brothers Medical Publishers All rights reserved. No part of this book may be reproduced in any form or by any means without the prior permission of the publisher. -

Biological Research in the Evolution of Cancer Surgery: a Personal Perspective Bernard Fisher
AACR Centennial Series Biological Research in the Evolution of Cancer Surgery: A Personal Perspective Bernard Fisher University of Pittsburgh, Pittsburgh, Pennsylvania Abstract Introduction During the 19th, and for most of the 20th century, malignant It is of historic interest that the American Association for Cancer tumors were removed by mutilating radical anatomic dissec- Research (AACR) was founded by four surgeons, five pathologists, tion. Advances such as anesthesia, asepsis, and blood one chemist, and a biochemist at the 25th meeting of the American transfusion made possible increasingly more radical oper- Surgical Association in Washington, DC, on May 7, 1907. The aim of ations. There was no scientific rationale for the operations the newly formed organization was to improve cancer research and being performed. Surgery in the 20th century was dominated treatment of cancer and to promote prevention. In recognition of by the principles of William S. Halsted, who contended that the 100th anniversary of the AACR, this article will examine the the bloodstream was of little significance as a route of tumor role biological research has played in the evolution of cancer cell dissemination; a tumor was autonomous of its host; and surgery. cancer was a local-regional disease that spread in an orderly Four principal aspects with regard to biological research will be fashion based on mechanical considerations. Halsted believed addressed:( a) whether research played a part in instigating surgical that both the extent and nuances of an operation influenced advances that occurred during the 19th and the first half of the patient outcome and that inadequate surgical skill was 20th centuries; (b) whether research formed the basis for the responsible for the failure to cure. -

Genetic Causes of Congenital Malformation in India
International Journal of Human Genetics ISSN: 0972-3757 (Print) (Online) Journal homepage: http://www.tandfonline.com/loi/rhug20 Genetic Causes of Congenital Malformation in India Geeta Talukder & Archana Sharma To cite this article: Geeta Talukder & Archana Sharma (2006) Genetic Causes of Congenital Malformation in India, International Journal of Human Genetics, 6:1, 15-25, DOI: 10.1080/09723757.2006.11885942 To link to this article: https://doi.org/10.1080/09723757.2006.11885942 Published online: 04 Sep 2017. Submit your article to this journal Article views: 2 View related articles Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=rhug20 © Kamla-Raj 2006 Int J Hum Genet, 6(1): 15-25 (2006) Genetic Causes of Congenital Malformation in India Geeta Talukder1 and Archana Sharma2 1. Vivekananda Institute of Medical Sciences, 99 Sarat Bose Road, Kolkata 700 026, West Bengal, India E-mail: geetatalukdar @hotmail.com 2. CAS in Cell & Chromosome Research, Department of Botany, University College of Science, 35 Ballygunj Circular Road, Kolkata 700 019, West Bengal, India KEYWORDS Congenital malformations; neonates; stillbirths; prenatal detection; prevention ABSTRACT Congenital malformations are a major cause of death of neonates in India where prenatal detection and treatment are not adequate in many hospitals and health centers. Incidence is specially high in stillbirths. It is not realized that genetic causes - chromosomal, single gene and polygenic - are the main causes of many congenital defects and early detection and prevention should be essential to make the small family norm a success. INTRODUCTION Recently Patel and Adhia (2005) detected major malformations in 7.92% of 17653 births and Phenotypic changes of genetic diseases at were able to attribute chromosomal cause to birth include congenital malformations in 4%,polygenic to 45.1% and total genetic chromosomes and single gene defects. -

Congenital Transverse Defects of Limbs and Digits* ('Intrauterine Amputation') by H
Arch Dis Child: first published as 10.1136/adc.37.193.263 on 1 June 1962. Downloaded from CONGENITAL TRANSVERSE DEFECTS OF LIMBS AND DIGITS* ('INTRAUTERINE AMPUTATION') BY H. G. KOHLER From the Department ofPathology, Birmingham Maternity Hospital (RECEIVED FOR PUBLICATION OCTOBER 23, 1961) Intrauterine amputation of the extremities is an Thomas Bartholin of Copenhagen (1616-1680) uncommon and peculiar congenital deformity which is said to be the first to mention a congenitally is characterized by the absence of one or more distal deficient extremity. He lived at the very threshold limb portions. Termination of the proximal part of the modern scientific era and belonged to a family is usually abrupt and bears no apparent relation to well known for their contributions to medicine and anatomical boundaries. The term 'amputation' biology: Thomas Bartholin's son, Caspar Secundus, suggests separation, by mechanical force, of a limb was the first to describe the vestibulo-vaginal glands. already formed rather than a failure of develop- Thomas was a man of great learning and wide ment, but such a view of the pathogenesis of this interests (Rhodes, 1957). His textbook on anatomy abnormality is far from universally accepted. It was translated into English and used widely for a would probably be better to use a neutral term such long time. Bartholin's descriptions of monsters, as 'transverse defects', but for the conservatism of however, tend to be more imaginative than factual medical nomenclature. (Hendry and Kohler, 1956). The essay which copyright. Circular grooves around the digits or limbs, and contains a reference to limb defects bears the title similar soft tissue defects, also known as ring con- 'Gravidarum Imaginatio' and there, in passing, he strictions, are seen usually in association with 'intra- tells us of a deformed male infant with only one uterine amputation', but also on their own. -

GUIDE to ADAPTED SWIMMING CLASSIFICATIONS Swimming Is
GUIDE TO ADAPTED SWIMMING CLASSIFICATIONS Swimming is the only sport that combines the conditions of limb loss, cerebral palsy (coordination and movement restrictions), spinal cord injury (weakness or paralysis involving any combination of the limbs) and other disabilities (such as Dwarfism (little people); major joint restriction conditions) across classes. Classes 1-10 – are allocated to swimmers with a physical disability Classes 11-13 – are allocated to swimmers with a visual disability Class 14 – is allocated to swimmers with an intellectual disability The Prefix S to the Class denotes the class for Freestyle, Backstroke and Butterfly The Prefix SB to the class denotes the class for Breaststroke The Prefix SM to the class denotes the class for Individual Medley. The range is from the swimmers with severe disability (S1, SB1, SM1) to those with the minimal disability (S10, SB9, SM10) In any one class some swimmers may start with a dive or in the water depending on their condition. This is factored in when classifying the athlete. The examples are only a guide – some conditions not mentioned may also fit the following classes. Locomotor Impaired (S1-S10): S1: Generally persons with complete spinal cord injuries below C4-C5 or cerebral palsy characterized by severe quadriplegia. Unable to catch the water. Severely limited propulsion from the arms due to muscle weakness, restricted range of motion or uncoordinated movements. No trunk control. No functional leg movements and significant leg drag. Assisted water start. Ordinarily uses the backstroke because of an inability to turn the head to breathe when swimming freestyle. S2: Generally persons with complete spinal cord injuries below C6-C7 or similar musculoskeletal impairment or cerebral palsy characterized by severe quadriplegia. -

County of Ventura Public Health Services Notice of Changes To
County of Ventura Notice of Changes to Policy Manual Emergency Medical Services Public Health Services Policies and Procedures To: ALL VENTURA COUNTY EMS POLICY MANUAL HOLDERS Change No.: 2 DATE: December 1, 2012 Policy Status Policy # Title/New Title Notes Replace Table of Contents Replace 105 PSC Operating Guidelines Review Only 106 Development of Proposed Policies/Procedures Replace 112 Ambulance Rates Replace 410 ALS Base Hospital Approval Process Replace 420 Receiving Hospital Standards Review Only 440 Code STEMI Interfacility Transfer New 450 Acute Stroke Center (ASC) Standards New 451 Stroke System Triage and Destination Replace 500 Ventura County EMS Services Provider Agencies Withholding or Termination of Resuscitation and Replace 606 Determination of Death Replace 627 Fireline Medic Replace 705.00 General Patient Guidelines Replace 705.01 Trauma Treatment Guidelines Review Only 705.02 Allergic/Adverse Reaction and Anaphylaxis Replace 705.03 Altered Neurological Function Review Only 705.04 Behavioral Emergencies Review Only 705.05 Bites and Stings Review Only 705.06 Burns Replace 705.07 Cardiac Arrest/Asystole & PEA Replace 705.08 Cardiac Arrest VF/FT Review Only 705.11 Crush Injury/Syndrome Replace 705.12 Heat Emergencies Replace 705.13 Hypothermia Replace 705.14 Hypovolemic/Septic Shock Replace 705.18 Overdose/Poisoning Replace 705.19 Pain Control Review Only 705.20 Seizures County of Ventura Notice of Changes to Policy Manual Emergency Medical Services Public Health Services Policies and Procedures Policy Status Policy # Title/New -

The Spine, Trauma and Infection
Develop. Med. Child Neurol. 1982, 24. 202-218 Review Article Robert N. Hensinger Eric T. Jones Developmental Orthopaedics. 11: The Spine, Trauma and Infection Torticollis Congenital muscular torticollis is Torticollis, or wryneck, is a common believed to result from local trauma to the clinical sign in a wide variety of childhood soft tissues of the neck during delivery. illnesses. When recognized at or soon after Birth records of these children birth, the usual cause is congenital demonstrate a preponderance of breech or muscular torticollis. However, difficult forceps deliveries, or primiparous roentgenograms of the cervical spine births', '. A common misconception is that should be obtained to exclude other less the neck is contused during delivery and common congenital conditions, such as the the resultant hematoma leads to fibrosis fixed or bony torticollis associated with and contracture. However, experimental Klippel-Feil syndrome and/or anomalies of the atlanto-axial articulation (Table I). TABLE I Congenital muscular torticollis is Differential diagnosis of torticollis usually discovered in the first six to eight weeks of life. If the infant is examined Congenital Congenital muscular torticollis within the first month of life, commonly a Klippel-Feil syndrome mass or 'tumor' is palpable in the neck' Basilar impressions Atlanto-occipital fusion (Fig. 1). Generally there is a non-tender, Pterygium colli (skin webs) soft enlargement which is mobile beneath Odontoid anomalies the skin and attached to or located within Neurological the body of the sternocleidomastoid Ocular dysfunction muscle. The mass obtains maximum size Syringomyelia Spinal-cord or cerebellar tumors (posterior within the first month and then gradually fossa) regresses. -

Appendix 3.1 Birth Defects Descriptions for NBDPN Core, Recommended, and Extended Conditions Updated March 2017
Appendix 3.1 Birth Defects Descriptions for NBDPN Core, Recommended, and Extended Conditions Updated March 2017 Participating members of the Birth Defects Definitions Group: Lorenzo Botto (UT) John Carey (UT) Cynthia Cassell (CDC) Tiffany Colarusso (CDC) Janet Cragan (CDC) Marcia Feldkamp (UT) Jamie Frias (CDC) Angela Lin (MA) Cara Mai (CDC) Richard Olney (CDC) Carol Stanton (CO) Csaba Siffel (GA) Table of Contents LIST OF BIRTH DEFECTS ................................................................................................................................................. I DETAILED DESCRIPTIONS OF BIRTH DEFECTS ...................................................................................................... 1 FORMAT FOR BIRTH DEFECT DESCRIPTIONS ................................................................................................................................. 1 CENTRAL NERVOUS SYSTEM ....................................................................................................................................... 2 ANENCEPHALY ........................................................................................................................................................................ 2 ENCEPHALOCELE ..................................................................................................................................................................... 3 HOLOPROSENCEPHALY............................................................................................................................................................. -

Congenital Hand Differences
Congenital Hand Differences in the Media JENNA GODFREY, MD SLOCUM CENTER FOR ORTHOPEDICS AND SPORTS MEDICINE https://www.youtube.com/watch?v=CM2QJO2IDFo Reactions to the videos No No’s Hand Arm Anatomy Embryology Limb buds: mesoderm covered in ectoderm Mesoderm: “Means to get around” aka skeletal, cardiovascular Ectoderm: “Attractoderm” aka skin hair nails brain Endoderm: “Endernal-organs” NOT INCLUDED HERE Upper limb bud: WEEK 6 Hand plate: WEEK 8 Limb axis formation: Proximodistal axis, dorsoventral axis, anteroposterior axis Are congenital hand differences common? 1982 study Lamb et al.: 11/10,000 births Most common: syndactyly, polydactyly, camptodactyly Classification of Congenital Hand Differences AmeliaAmelia: congenitalcongenital amputationamputation of upper extremityextremity Hemimelia: absence of part of limb, eg forearm https://www.youtube.com/watch?v=kbHXIN6EzWo Achiria: absent wrist Peromelia: absent hand Ametacarapia: absent metacarpals Aphalangia: absent finger Phocomelia: segmental failure of limb growth Greek for “seal limb” Thalidomide: Drug used for morning sickness in pregnant women 1960s 3 types I: Hand attached to scapula II: Forearm attached to scapula III: Absent forearm with hand attached to humerus Syndactyly: fusion of adjacent fingers Partial v Complete Simple v Complex v “Complicated” Brachy: short, eg brachymetacarpia, brachydactyly http://www.cc.com/video- clips/7ynwra/tosh-0-megan-fox-s- toe-thumbs • Symbrachydact yly: Nubbins Puckered skin 4 types **they have fingernails Amniotic Constriction -
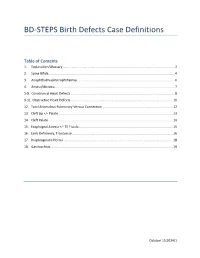
BD-STEPS Birth Defects Case Definitions
BD-STEPS Birth Defects Case Definitions Table of Contents 1. Explanation/Glossary ............................................................................................................................ 2 2. Spina Bifida............................................................................................................................................ 4 3. Anophthalmia/microphthalmia ............................................................................................................ 6 4. Anotia/Microtia ..................................................................................................................................... 7 5-8. Conotruncal Heart Defects ................................................................................................................... 8 9-11. Obstructive Heart Defects ................................................................................................................. 10 12. Total Anomalous Pulmonary Venous Connection .............................................................................. 12 13. Cleft Lip +/- Palate ............................................................................................................................... 13 14. Cleft Palate .......................................................................................................................................... 14 15. Esophageal Atresia +/- TE Fistula ........................................................................................................ 15 16. Limb -
![Half Man, Half Prosthesis: the Rehabilitation of People with Hemicorporectomy – Case Series [Version 1; Peer Review: Awaiting Peer Review]](https://docslib.b-cdn.net/cover/6424/half-man-half-prosthesis-the-rehabilitation-of-people-with-hemicorporectomy-case-series-version-1-peer-review-awaiting-peer-review-2526424.webp)
Half Man, Half Prosthesis: the Rehabilitation of People with Hemicorporectomy – Case Series [Version 1; Peer Review: Awaiting Peer Review]
F1000Research 2021, 10:298 Last updated: 27 JUL 2021 CLINICAL PRACTICE ARTICLE Half man, half prosthesis: the rehabilitation of people with hemicorporectomy – case series [version 1; peer review: awaiting peer review] André Tadeu Sugawara, Milton Seigui Oshiro, Eduardo Inglez Yamanaka, Ronaldo Meneghetti, Dayrin Vanessa Tarazona Carvajal , Leandro Ryuchi Iuamoto , Linamara Rizzo Battistella Instituto de Medicina Fisica e Reabilitacao, Hospital das Clinicas da Faculdade de Medicina da Universidade de Sao Paulo, Sao Paulo, Sao Paulo, 04101-300, Brazil v1 First published: 19 Apr 2021, 10:298 Open Peer Review https://doi.org/10.12688/f1000research.51636.1 Latest published: 19 Apr 2021, 10:298 https://doi.org/10.12688/f1000research.51636.1 Reviewer Status AWAITING PEER REVIEW Any reports and responses or comments on the Abstract article can be found at the end of the article. Hemicorporectomy is a procedure where the lumbar spine and spinal cord, pelvic bones and contents, lower extremities and external genitalia are surgically removed. The rehabilitation process, in addition to being prolonged and costly, is challenging. This article reports the rehabilitation process for hemicorporectomy and shows the innovative solutions for mobility for this disability for two cases of paraplegic patients: case 1 due to traumatic spinal cord injury due to firearm injury and case 2 due to lumbosacral myelomeningocele. They presented chronic pressure ulcer which evolved to neoplastic transformation. (squamous cell carcinoma - Marjolin's ulcer). The cases were submitted to L4 hemicorporectomy and were rehabilitated to ensure the right to mobility independence for activities of daily living; social inclusion; prevention of comorbidities and pluralization of disabilities. -

EUROCAT Syndrome Guide
JRC - Central Registry european surveillance of congenital anomalies EUROCAT Syndrome Guide Definition and Coding of Syndromes Version July 2017 Revised in 2016 by Ingeborg Barisic, approved by the Coding & Classification Committee in 2017: Ester Garne, Diana Wellesley, David Tucker, Jorieke Bergman and Ingeborg Barisic Revised 2008 by Ingeborg Barisic, Helen Dolk and Ester Garne and discussed and approved by the Coding & Classification Committee 2008: Elisa Calzolari, Diana Wellesley, David Tucker, Ingeborg Barisic, Ester Garne The list of syndromes contained in the previous EUROCAT “Guide to the Coding of Eponyms and Syndromes” (Josephine Weatherall, 1979) was revised by Ingeborg Barisic, Helen Dolk, Ester Garne, Claude Stoll and Diana Wellesley at a meeting in London in November 2003. Approved by the members EUROCAT Coding & Classification Committee 2004: Ingeborg Barisic, Elisa Calzolari, Ester Garne, Annukka Ritvanen, Claude Stoll, Diana Wellesley 1 TABLE OF CONTENTS Introduction and Definitions 6 Coding Notes and Explanation of Guide 10 List of conditions to be coded in the syndrome field 13 List of conditions which should not be coded as syndromes 14 Syndromes – monogenic or unknown etiology Aarskog syndrome 18 Acrocephalopolysyndactyly (all types) 19 Alagille syndrome 20 Alport syndrome 21 Angelman syndrome 22 Aniridia-Wilms tumor syndrome, WAGR 23 Apert syndrome 24 Bardet-Biedl syndrome 25 Beckwith-Wiedemann syndrome (EMG syndrome) 26 Blepharophimosis-ptosis syndrome 28 Branchiootorenal syndrome (Melnick-Fraser syndrome) 29 CHARGE