The Autonomic Nervous System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Neuroanatomy of Female Pelvic Pain
Chapter 2 The Neuroanatomy of Female Pelvic Pain Frank H. Willard and Mark D. Schuenke Introduction The female pelvis is innervated through primary afferent fi bers that course in nerves related to both the somatic and autonomic nervous systems. The somatic pelvis includes the bony pelvis, its ligaments, and its surrounding skeletal muscle of the urogenital and anal triangles, whereas the visceral pelvis includes the endopelvic fascial lining of the levator ani and the organ systems that it surrounds such as the rectum, reproductive organs, and urinary bladder. Uncovering the origin of pelvic pain patterns created by the convergence of these two separate primary afferent fi ber systems – somatic and visceral – on common neuronal circuitry in the sacral and thoracolumbar spinal cord can be a very dif fi cult process. Diagnosing these blended somatovisceral pelvic pain patterns in the female is further complicated by the strong descending signals from the cerebrum and brainstem to the dorsal horn neurons that can signi fi cantly modulate the perception of pain. These descending systems are themselves signi fi cantly in fl uenced by both the physiological (such as hormonal) and psychological (such as emotional) states of the individual further distorting the intensity, quality, and localization of pain from the pelvis. The interpretation of pelvic pain patterns requires a sound knowledge of the innervation of somatic and visceral pelvic structures coupled with an understand- ing of the interactions occurring in the dorsal horn of the lower spinal cord as well as in the brainstem and forebrain. This review will examine the somatic and vis- ceral innervation of the major structures and organ systems in and around the female pelvis. -

Thoracic Anatomy Autonomic Nervous System
Thoracic anatomy Autonomic nervous system Thoracic Anatomy 3.G.1.1 James Mitchell (December 24, 2003) Autonomic nervous system Division by direction Visceral efferent Preganglionic myelinated, postganglionic unmyelinated Synapse in ganglia Visceral afferent Similar to somatic afferent Cell body in CNS, peripheral processes travel with autonomic and somatic fibres Division by outflow Sympathetic Thoracolumbar outflow: T1-L3 Synapse in sympathetic trunk ganglia or other ganglia near CNS Preganglionic cholinergic, postganglionic predominantly noradrenergic (also adrenergic, cholinergic sudomotor and purinergic) Parasympathetic Craniosacral outflow: III, VII, IX, X, S2-4 Synapse adjacent to end-organs Cranial nerve parasympathetic ganglia are traversed by other fibres but contain only parasympathetic synapses Parasympathetic anatomy III Edinger-Westphal nuclei → oculomotor n. → n. to inferior oblique → ciliary ganglion → short ciliary nn. → ciliary muscle and sphincter pupillae VII Superior salivatory nucleus → nervus intermedius → facial n. → chorda tympani → lingual n. → submandibular ganglion → submandibular and sublingual glands Geniculate ganglion → greater petrosal n. → pterygopalatine ganglion → zygomatic and lacrimal nerves to lacrimal gland and nasal and palatine branches to nasal mucosa XI Inferior salivatory nucleus → glossopharyngeal nerve → tympanic plexus → lesser petrosal n. → otic ganglion → auriculotemporal n. → parotid gland and oral mucosa X Dorsal nucleus of vagus → vagus n. → minute ganglia in respiratory tract, heart, -

Sympathetic Tales: Subdivisons of the Autonomic Nervous System and the Impact of Developmental Studies Uwe Ernsberger* and Hermann Rohrer
Ernsberger and Rohrer Neural Development (2018) 13:20 https://doi.org/10.1186/s13064-018-0117-6 REVIEW Open Access Sympathetic tales: subdivisons of the autonomic nervous system and the impact of developmental studies Uwe Ernsberger* and Hermann Rohrer Abstract Remarkable progress in a range of biomedical disciplines has promoted the understanding of the cellular components of the autonomic nervous system and their differentiation during development to a critical level. Characterization of the gene expression fingerprints of individual neurons and identification of the key regulators of autonomic neuron differentiation enables us to comprehend the development of different sets of autonomic neurons. Their individual functional properties emerge as a consequence of differential gene expression initiated by the action of specific developmental regulators. In this review, we delineate the anatomical and physiological observations that led to the subdivision into sympathetic and parasympathetic domains and analyze how the recent molecular insights melt into and challenge the classical description of the autonomic nervous system. Keywords: Sympathetic, Parasympathetic, Transcription factor, Preganglionic, Postganglionic, Autonomic nervous system, Sacral, Pelvic ganglion, Heart Background interplay of nervous and hormonal control in particular The “great sympathetic”... “was the principal means of mediated by the sympathetic nervous system and the ad- bringing about the sympathies of the body”. With these renal gland in adapting the internal -

Morphology of Sympathetic Chain in Saguinus Niger
Anais da Academia Brasileira de Ciências (2013) 85(1): 365-370 (Annals of the Brazilian Academy of Sciences) Printed version ISSN 0001-3765 / Online version ISSN 1678-2690 www.scielo.br/aabc Morphology of sympathetic chain in Saguinus niger MARINA P.E. PINTO1, ÉRIKA BRANCO1, EMERSON T. FIORETTO2, LUIZA C. PEREIRA3 and ANA R. LIMA1 1Universidade Federal Rural da Amazônia (UFRA), Instituto de Saúde e Produção Animal – ISPA, Faculdade de Medicina Veterinária, Avenida Perimetral, 2501, Belém, PA, Brasil 2 Universidade Federal de Sergipe (UFS), Cidade Universitária Professor José Aloísio de Campos, Avenida Marechal Rondon, s/n, Jardim Rosa Elze, São Cristovão, Aracajú, SE, Brasil 3 Empresa Hydro LTDA, Mina de Bauxita – Paragominas, PA, Brasil Manuscript received on March 20, 2012; accepted for publication on October 2, 2012 ABSTRACT Saguinus niger popularly known as Sauim, is a Brazilian North primate. Sympathetic chain investigation would support traumatic and/or cancer diagnosis which are little described in wild animals. The aim of this study was to describe the morphology and distribution of sympathetic chain in order to supply knowledge for neurocomparative research. Three female young animals that came death by natural causes were investigated. Animals were fixed in formaldehyde 10% and dissected along the sympathetic chain in neck, thorax and abdomen. Cranial cervical ganglion was located at the level of carotid bifurcation, related to carotid internal artery. In neck basis the vagosympathetic trunk divides into the sympathetic trunk and the parasympathetic vagal nerve. Sympathetic trunk ran in dorsal position and originated the stellate ganglia, formed by the fusion of caudal cervical and first thoracic ganglia. -

The Intrinsic Cardiac Nervous System and Its Role in Cardiac Pacemaking and Conduction
Journal of Cardiovascular Development and Disease Review The Intrinsic Cardiac Nervous System and Its Role in Cardiac Pacemaking and Conduction Laura Fedele * and Thomas Brand * Developmental Dynamics, National Heart and Lung Institute (NHLI), Imperial College, London W12 0NN, UK * Correspondence: [email protected] (L.F.); [email protected] (T.B.); Tel.: +44-(0)-207-594-6531 (L.F.); +44-(0)-207-594-8744 (T.B.) Received: 17 August 2020; Accepted: 20 November 2020; Published: 24 November 2020 Abstract: The cardiac autonomic nervous system (CANS) plays a key role for the regulation of cardiac activity with its dysregulation being involved in various heart diseases, such as cardiac arrhythmias. The CANS comprises the extrinsic and intrinsic innervation of the heart. The intrinsic cardiac nervous system (ICNS) includes the network of the intracardiac ganglia and interconnecting neurons. The cardiac ganglia contribute to the tight modulation of cardiac electrophysiology, working as a local hub integrating the inputs of the extrinsic innervation and the ICNS. A better understanding of the role of the ICNS for the modulation of the cardiac conduction system will be crucial for targeted therapies of various arrhythmias. We describe the embryonic development, anatomy, and physiology of the ICNS. By correlating the topography of the intracardiac neurons with what is known regarding their biophysical and neurochemical properties, we outline their physiological role in the control of pacemaker activity of the sinoatrial and atrioventricular nodes. We conclude by highlighting cardiac disorders with a putative involvement of the ICNS and outline open questions that need to be addressed in order to better understand the physiology and pathophysiology of the ICNS. -

THE ANATOMY of the SYMPATHETHIC TRUNKS in MAN by MARTIN WRETE Histological Department, the University of Uppsala, Sweden
[ 448 ] THE ANATOMY OF THE SYMPATHETHIC TRUNKS IN MAN BY MARTIN WRETE Histological Department, The University of Uppsala, Sweden INTRODUCTION Even a cursory study of the anatomical descriptions of the cervical parts of the sympathetic trunks given in modern text-books or articles discloses that, now as earlier, great confusion exists with respect to terminology. This applies even to monographs and more specialized presentations. The primary cause of this confusion is the very marked variability of the trunks in the neck region, which gives wide scope for arbitrary interpretations of the arrangement; some uncertainty about the terminology and notation of other parts of the trunks also persists. It is true that the terms to be used for the sympathetic nervous system were fixed by the International Anatomical Nomenclature Committee (Nomina Anatomica, Paris, 1955). This does not, however, prevent some of the individual terms being used to denote different anatomical units, and for practical reasons (such as limiting printing costs) comprehensive explanations could not always be given in the annota- tions to the Parisian Nomina Anatomica. As one of the three members of the Sub- Committee responsible for the nomenclature of the peripheral nervous system, I wish to define more exactly my views on the terminology adopted for the sympathetic trunks. I also take this opportunity of revising a few terms I used in certain papers published some twenty years ago. In Nomina Anatomica the term truncus sympathicus is followed by the names of its ganglia, ganglia trunci sympathici, as well as of its connecting rami interganglio- nares. But, also under the heading ganglia trunci sympathici, the term ganglia intermedia is used to denote ganglia on the rami communicantes and certain ganglia on the trunks in the rami interganglionares between the other ganglia-namely the ganglion cervicale superius, ganglion cervicale medium, ganglion cervicothoracicum (s. -

Autonomic Nervous System
NERVOUS SYSTEM OUTLINE 18.1 Comparison of the Somatic and Autonomic Nervous Systems 540 18.2 Overview of the Autonomic Nervous System 542 18 18.3 Parasympathetic Division 545 18.3a Cranial Nerves 545 18.3b Sacral Spinal Nerves 545 18.3c Effects and General Functions of the Parasympathetic Division 545 Autonomic 18.4 Sympathetic Division 547 18.4a Organization and Anatomy of the Sympathetic Division 547 18.4b Sympathetic Pathways 550 Nervous 18.4c Effects and General Functions of the Sympathetic Division 550 18.5 Other Features of the Autonomic Nervous System 552 System 18.5a Autonomic Plexuses 552 18.5b Neurotransmitters and Receptors 553 18.5c Dual Innervation 554 18.5d Autonomic Reflexes 555 18.6 CNS Control of Autonomic Function 556 18.7 Development of the Autonomic Nervous System 557 MODULE 7: NERVOUS SYSTEM mck78097_ch18_539-560.indd 539 2/14/11 3:46 PM 540 Chapter Eighteen Autonomic Nervous System n a twisting downhill slope, an Olympic skier is concentrat- Recall from figure 14.2 (page 417) that the somatic nervous O ing on controlling his body to negotiate the course faster than system and the autonomic nervous system are part of both the anyone else in the world. Compared to the spectators in the viewing central nervous system and the peripheral nervous system. The areas, his pupils are more dilated, and his heart is beating faster SNS operates under our conscious control, as exemplified by vol- and pumping more blood to his skeletal muscles. At the same time, untary activities such as getting out of a chair, picking up a ball, organ system functions not needed in the race are practically shut walking outside, and throwing the ball for the dog to chase. -

Hadeel Abdullah Nadeen AL-Falooji Dena Kofahi Mohammad Hesham
Hadeel Abdullah Nadeen AL-Falooji Dena Kofahi Mohammad Hesham 0 | P a g e Nerves ON THE POSTERIOR ABDOMINAL WALL The Lumbar Plexus The lumbar plexus, which is one of the main nervous pathways supplying the lower limb, is formed in the psoas major muscle -in the abdomen- from the anterior rami of the upper four lumbar spinal nerves (L1-L4). Its branches emerge from the lateral₁ and medial₂ borders of the muscle and from its anterior₃ surface. Branches of the Lumbar Plexus - The iLiohypogastric nerve₁, iLioinguinal nerve₂, Lateral cutaneous nerve of the thigh₃, and femoraL nerve₄ emerge from the Lateral border of the psoas, in that order from above downward. - The obturator nerve₁ and lumbosacral trunk₂ emerge from the medial border of the psoas major. - The genitofemoral₁ nerve emerges from the anterior surface of the psoas major. The lumbosacral trunk: It is formed from the L4 (from the lumbar plexus) and L5 (from the sacral plexus) nerve roots (i.e. the fourth lumbar nerve gives off branches to the sacral plexus forming the lumbosacral trunk). - The ventral (anterior) rami of L1 form the iliohypogastric₁ and ilioinguinal₂ nerves which run between the transversus abdominis muscle and abdominal internal oblique muscle. Then: 1. The iliohypogastric nerve (L1) gives off several motor branches to abdominal muscles and a sensory branch to the skin of the lower part of the anterior abdominal wall above the pubic symphysis. 2. The ilioinguinal nerve (L1) pierces the posterior wall of the inguinal canal and runs along with the spermatic cord (through the canal) to supply the skin of the groin and the scrotum or labium majus. -

The Parasympathetic System
DR MOUIN ABBOUD PR OF ANATOMY In faculity of medecin ( Damascus and Sham uneversities ) Specialist in respiratory diseases الدكتور معين عبود استاذ التشريح في كلية الطب البشري في جامعة دمشق وجامعة الشام الخاصة اختصاصي في أمراض جهاز التنفس DR MOUIN ABBOUD Abdominal viscera Innervation The Innervation Abdominal viscera are innervated by both : extrinsic ) visceral innervation ( involves : . receiving motor impulses from the central nervous system . and sending sensory information to, the central nervous system; and intrinsic components of the nervous system: involves the regulation of digestive tract activities by a generally self-sufficient network of sensory and motor neurons (the enteric nervous system). Visceral innervation The visceral innervation is transmited by Autonomic Plexuses )prevertebral plexus ). By which : these viscera send sensory information back to the central nervous system through visceral afferent fibers and receive motor impulses from the central nervous system through visceral efferent fibers. prevertebral plexus The abdominal prevertebral plexus receives: preganglionic parasympathetic and visceral afferent fibers from the vagus nerves [X]; preganglionic sympathetic and visceral afferent fibers from the thoracic and lumbar splanchnic nerves; preganglionic parasympathetic fibers from the pelvic splanchnic nerves. The Sympathetic Division The sympathetic division consists of the following: Preganglionic fibers in the lateral grey column of the thoracic and upper two lumbar segments of the spinal cord. Ganglionic neurons in : . Sympathetic chain ganglia, also called paravertebral, or lateral ganglia . Collateral ganglia, also known as prevertebral ganglia . Specialized neurons in the interior of the suprarenal gland Postganglionic fibers : to target organs Sectional Organization of the Spinal Cord The parasympathetic system The parasympathetic system is less neatly defined Preganglionic fibers . -

Autonomic Nervous System of the Pelvis — General Overview
FOLIA MEDICA CRACOVIENSIA Vol. LVIII, 2, 2018: 21–44 PL ISSN 0015-5616 DOI: 10.24425/fmc.2018.124656 Autonomic nervous system of the pelvis — general overview Justyna Sienkiewicz-Zawilińska1, Jarosław Zawiliński1, Lourdes Niroya Kaythampillai1, Marcin Jakiel1, Jacenty Urbaniak1, Tomasz Bereza1, Wojciech Kowalski2, Marios Loukas3, Jerzy Walocha1 1Department of Anatomy, Jagiellonian University Medical College, Kraków, Poland 2Gabinety Lekarskie Wojciech Kowalski, Kraków, Poland 3Department of Anatomy, St. George’s University, Grenada Corresponding author: Jerzy A. Walocha, MD, PhD Department of Anatomy, Jagiellonian University Medical College ul. Kopernika 12, 31-034 Kraków, Poland Phone: +48 12 422 95 11; E-mail: [email protected] Abstract: Autonomic nervous system of the pelvis is still poorly understood. Every year more and more pelvic procedures are carried out on patients suff ering from diff erent pelvic disorders what leads to numerous pelvic dysfunctions. Authors tried to review, starting from historical and clinical background, the most important reports on anatomy of the pelvic autonomic plexuses. We also pay attention to complete lack of knowledge of students of medicine on the autonomic nervous structures in the area studied. We present anatomical description of the pelvic plexuses including their visceral branches and anatomy of surrounding pelvic tissues which still remains unclear. More and more attention is paid to the topography of the plexuses specially because of new pain releasing techniques — neurolysies. Key words: autonomic nervous system, inferior hypogastric plexus, anatomy, nerve sparing, pelvis. 22 Justyna Sienkiewicz-Zawilińska, Jarosław Zawiliński, et al. Introduction Th e innervation of human pelvis was a subject of numerous studies and reports of the scientists who studied both fresh and embalmed cadavers (Hunter, Lee, Beck, Frankenhäuser, Davis, Labate, Krantz, Quinn). -

CHAPTER 2 Organization of the Peripheral Nervous System
15 CHAPTER 2 Organization of the Peripheral Nervous System SOME FUNDAMENTAL DICHOTOMIES The Paravertebral Ganglia and Their Primary DEFINED Role in Innervating Visceral Motor Structures of Central Versus Peripheral Nervous System the Body Wall Motor Versus Sensory Portions of the Nervous Preganglionic Input to Paravertebral Ganglia System The Sympathetic Chain Visceral Versus Somatic Neurons Sympathetic Innervation of Internal Organs Summary of the Sympathetic System DEVELOPMENT AND INNERVATION OF THE The Parasympathetic Nervous System BODY WALL Somites and Their Dermomyotomes THE VISCERAL SENSORY SYSTEM Segmentation of the Neural Tube Referred Pain Formation of the Spinal Nerve INTERESTING SIDELIGHTS VISCERAL MOTOR STRUCTURES AND THE Visceral Sensory Axons in the Ventral Roots of AUTONOMIC NERVOUS SYSTEM Spinal Nerves The Subdivisions of the Autonomic Nervous Enteric Nervous System System--Sympathetic and Parasympathetic Possible Roles for Sympathetic Neurons in Other The Sympathetic Nervous System Than Visceral Motor Functions SOME FUNDAMENTAL DICHOTOMIES DEFINED Central Versus Peripheral Nervous System The brain and spinal cord compose the central nervous system (CNS). All the nerves that emanate from the CNS, their branches, and interconnections constitute the peripheral nervous system (PNS). Nerves that exit directly from the brain are said to be cranial nerves. The rest of the PNS consists of the spinal nerves (with their branches) and that part of the autonomic nervous system (see further on) associated with spinal nerves. A detailed consideration of brain and spinal cord structure is the province of neuro-anatomists. Gross anatomists are concerned with the PNS. An understanding of the innervation of specific organs is one of the most clinically important tasks facing a student of medicine. -
Sympathetic Chain – Cervical Part
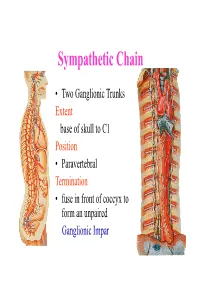
Sympathetic Chain • Two Ganglionic Trunks Extent base of skull to C1 Position • Paravertebral Termination • fuse in front of coccyx to form an unpaired Ganglionic Impar Sympathetic Chain •3 Ganglia in cervical part •11Ganglia in thoracic Part •4 lumbar Ganglia •4 Sacral ganglia Sympathetic Chain-cervical part • lie Behind Carotid Sheath and • in front of Longus colli & Longus Capitis muscles • Initially no. of Sympathetic ganglia correspond to no. of Spinal Nerves • Later • Superior formed by fusion of upper 4 cervical Ganglia • Middle by 5th and 6th •Inferiorby joining of 7th and 8th cervical ganglia Sympathetic Chain – Cervical Part • Cervical Part Ganglia Superior Cervical ganglia Middle Cervical Ganglia Inferior Cervical ganglia Sometimes Inferior cervical and first Thoracic fuse to form a Cervico-Thoracic or Stellate Ganglia Sympathetic Chain – Cervical Part • Do not receive white rami communicantes from cervical spinal segments • LAT. HORN CELLS OF T1-T5 PROVIDE PRE- GANGLIONIC FIBRES • Gives grey rami communicantes to all 8 cervical nerves Sympathetic Chain – Cervical Part • GANGLION • Contains-multipolar post ganglionic neurons & few interneurons (chromaffin or SIF cells*) • *modulate activities of post ganglionic neurons by dopamine • SYMPATHETIC TRUNK conveys pre & post ganglionic motor & sensory fibres between ganglia SUPERIOR CERVICAL GANGLION • Largest ,fusiform, 2.5cm length • Fuses upper four cervical ganglia • Situation- opposite C2 &C3 Vertebrae behind ICA& infont of l. capitis • Receives pre ganglionic fibres mostly from upper three thracic segments • BRANCHES (all convey post ganglionic fibres & some sensory fibres) SUPERIOR CERVICAL GANGLION • BRANCHES • Lateral-grey rami comm. to C1- C4 nerves &(C5-C8) • Medial-laryngo-pharyngeal - cardiac(no pain fibr.) Anterior-ramify around CCA,ECA & its branches Ascending-INTERNAL CAROTID NERVE -carotido-tympanic -deep petrosal -communicating(v,iii,iv,v,&vi) -nervus conarii (pineal gland) Term.communicating(ant.