Medical Physiology Learning Objectives
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Focusing on the Re-Emergence of Primitive Reflexes Following Acquired Brain Injuries
33 Focusing on The Re-Emergence of Primitive Reflexes Following Acquired Brain Injuries Resiliency Through Reconnections - Reflex Integration Following Brain Injury Alex Andrich, OD, FCOVD Scottsdale, Arizona Patti Andrich, MA, OTR/L, COVT, CINPP September 19, 2019 Alex Andrich, OD, FCOVD Patti Andrich, MA, OTR/L, COVT, CINPP © 2019 Sensory Focus No Pictures or Videos of Patients The contents of this presentation are the property of Sensory Focus / The VISION Development Team and may not be reproduced or shared in any format without express written permission. Disclosure: BINOVI The patients shown today have given us permission to use their pictures and videos for educational purposes only. They would not want their images/videos distributed or shared. We are not receiving any financial compensation for mentioning any other device, equipment, or services that are mentioned during this presentation. Objectives – Advanced Course Objectives Detail what primitive reflexes (PR) are Learn how to effectively screen for the presence of PRs Why they re-emerge following a brain injury Learn how to reintegrate these reflexes to improve patient How they affect sensory-motor integration outcomes How integration techniques can be used in the treatment Current research regarding PR integration and brain of brain injuries injuries will be highlighted Cases will be presented Pioneers to Present Day Leaders Getting Back to Life After Brain Injury (BI) Descartes (1596-1650) What is Vision? Neuro-Optometric Testing Vision writes spatial equations -

VTPP 423 Syllabus General
VTPP 423 BIOMEDICAL PHYSIOLOGY I COURSE INFORMATION Description: Biomedical Physiology I. (3-2). Credit 4. Physiological principles, review of cellular physiology, and development of an understanding of the nervous system and muscle, cardiovascular, and respiratory physiology; clinical applications related to organ systems. Prerequisites: VIBS 305; junior or senior classification. Discussions: MWF: 9:10 a.m. – 10:00 a.m. (Room 309, VICI) Lab Sessions: 501: Tuesdays : 12:40 - 2:30 p.m. (Room 320, VICI) 504: Fridays : 12:40 - 2:30 p.m. (Room 320, VICI) Instructor: J.D. Herman Office Hours: MWF 10:00 – 11:00 or by appointment Office Room # 316 VIDI Phone: 979/862-7765 [email protected] Teaching TBA Assistant: Required Lauralee Sherwood: Human Physiology: from cells to systems, 8th edition, Brooks/Cole Cengage Resources: Learning, ISBN: 978-1-111-57743-8 iClicker 2 Web-sites: htt p://ecampus.tamu.edu/ Course Goal: To understand the physiological significance of cells, organs and organ systems in maintaining homeostasis of the mammalian organism. (To develop critical thinking, problem solving and self- learning skills in preparation for a career in medicine/science.) Learning Outcomes: By the end of the course, the student will: • investigate and solve mathematical calculations commonly used in physiology • articulate an understanding of homeostatic control mechanisms of the: ▪ central nervous system ▪ muscular system ▪ cardiovascular system ▪ respiratory system ▪ renal system • collect and analyze physiologic data related to the ▪ central nervous system ▪ muscular system ▪ cardiovascular system ▪ respiratory system ▪ renal system • evaluate the relationship between physiology and disease ▪ including insight into critical thinking in the clinical setting ▪ including goals and mechanisms of some pharmacologic agents Course Grading: A total of 400 points are possible in the course. -

Neurophysiology (Revised 2012)
The American Physiological Society Medical Curriculum Objectives Project Complete curriculum objectives available at: http://www.the-aps.org/medphysobj Neurophysiology (revised 2012) Cellular Neurophysiology, Blood Brain Barrier, Cerebrovascular Physiology A. Physiology of the Neuron NEU 1. Define, and identify on a diagram of a motor neuron, the following regions: dendrites, axon, axon hillock, soma, and an axodendritic synapse. NEU 2. Define, and identify on a diagram of a primary sensory neuron, the following regions: receptor membrane, peripheral axon process, central axon process, soma, sensory ganglia. NEU 3. Write the Nernst equation, and explain the effects of altering the intracellular or extracellular Na+, K+, Cl-, or Ca2+ concentration on the equilibrium potential for that ion. NEU 4. Describe the normal distribution of Na+, K+, and Cl- across the cell membrane, and using the chord conductance (Goldman) equation, explain how the relative permeabilities of these ions create a resting membrane potential. NEU 5. Describe ionic basis of an action potential. NEU 6. Distinguish the effects of hyperkalemia, hypercalcemia, and hypoxia on the resting membrane and action potential. NEU 7. Explain how the abnormal function of ion channels (channelopathies) can alter the resting membrane and action potential and cause paralysis, ataxia, or night blindness. NEU 8. Describe the ionic basis of each of the following local graded potentials: excitatory post synaptic potential (EPSP), inhibitory post synaptic potential (IPSP), end plate potential (EPP) and a receptor (generator) potential. NEU 9. Contrast the generation and conduction of graded potentials (EPSP and IPSP) with those of action potentials. NEU 10. On a diagram of a motor neuron, indicate where you would most likely find IPSP, EPSP, action potential trigger point, and release of neurotransmitter. -

The Phenomenon of Multiple Stretch Reflexes
Henry Ford Hospital Medical Journal Volume 34 Number 1 Article 6 3-1986 The Phenomenon of Multiple Stretch Reflexes Robert D. Teasdall Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Recommended Citation Teasdall, Robert D. (1986) "The Phenomenon of Multiple Stretch Reflexes," Henry Ford Hospital Medical Journal : Vol. 34 : No. 1 , 31-36. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol34/iss1/6 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. The Phenomenon of Multiple Stretch Reflexes Robert D. Teasdall, MD* Multiple stretch reflexes occur in muscles adjacent to or remote from the tap. The response may be ipsilateral or bilateral. These reflexes are encountered not only in normal subjects with brisk stretch reflexes but particularly in patients with lesions of the upper motor neuron. The concussion obtained by the blow is conducted along bone to muscle. Muscle spindles are stimulated, and in this manner independent stretch reflexes are produced in these muscles. This mechanism is responsible for the phenomenon of multiple stretch reflexes. The thorax and pelvis play important roles in the contralateral responses by transmitting these mechanical events across the midline. (Henry FordHosp Med J 1986;34:31-6) ontraction of muscles remote from the site of f)ercussion is Head and neck Cencountered in patients with brisk stretch reflexes. -

Human Physiology (Biology 4) Laboratory Exercises
Human Physiology (Biology 4) Laboratory Exercises Instructor: Rebecca Bailey 1 Laboratory Exercises Lab 1: The Microscope and Overview of Organ Systems..................page 3 Lab 2: Cells & Tissues (See Supplement)........................................page 15 Lab 3: Transport 1 & 2 (See Supplement for Part 2)........................page 16 Labs 4 and 5: Nervous System (ADAM)...........................................page 19 Lab 6: Reflexes & Senses………………...........................................page 20 Lab 7: Muscular System (ADAM).....................................................page 31 Lab 7a: Whole Muscle Function (See Supplement).........................page 32 ---this lab is not done every semester, check your schedule--- Lab 8: ECG and Cardiovascular System…......................................page 33 Lab 9: Cardiovascular System (See Supplement, ADAM)...............page 41 Lab 10: Blood……….........................................................................page 42 Lab 11: Blood Slides and Respiratory System (ADAM)....................page 46 Lab 12: Respiratory System.............................................................page 49 Lab 13: Urinary System....................................................................page 54 Lab 14: Digestive System and Acid/Base Demo..............................page 60 At the end of each lab, you should be able to understand the concepts and processes learned and answer any of the questions investigated in the activity. You are expected to identify microscopic tissues/organs -

The Plantar Reflex
THE PLANTAR REFLEX a historical, clinical and electromyographic study From the Department of Neurology, Academic Hospital 'Dijkzigt', Rotterdam, The Netherlands THE PLANTAR REFLEX A HISTORICAL, CLINICAL AND ELECTROMYOGRAPHIC STUDY PROEFSCHRIFT TER VERKRIJGING VAN DE GRAAD VAN DOCTOR IN DE GENEESKUNDE AAN DE ERASMUS UNIVERSITEIT TE ROTTERDAM OP GEZAG VAN DE RECTOR MAGNIFICUS PROF. DR. B. LEIJNSE EN VOLGENS BESLU!T VAN HET COLLEGE VAN DEKANEN. DE OPENBARE VERDED!GING ZAL PLAATS VINDEN OP WOENSDAG 16 NOVEMBER 1977 DES NAMIDDAGS TE 4.15 UUR PREC!ES DOOR JAN VAN GIJN GEBOREN TE GELDERMALSEN 1977 KRIPS REPRO - MEPPEL PROMOTOR: DR. H. VAN CREVEL CO-PROMOTOR: PROF. DR. A. STAAL CO-REFERENTEN: PROF. DR. H. G. ]. M. KUYPERS PROF. DR. P. E. VOORHOEVE Aan mijn ouders Aan Carien, Maarten en Willem CONTENTS page GENERAL INTRODUCTION 15 CHAPTER I HISTORY OF THE PLANTAR REFLEX AS A CLINICAL SIGN DISCOVERY - the plantar reflex before Babinski 19 - the toe phenomenon . 21 - Joseph Babinski and his work 24 ACCEPTANCE - the pyramidal syndrome before the toe reflex 26 - confirmation . 26 - a curious eponym in Holland 28 - false positive findings? 29 - false negative findings 29 FLEXION AND EXTENSION SYNERGIES - the Babinski sign as part of a flexion synergy . 31 - opposition from Babinski and others . 33 - ipsilateral limb extension with downgoing toes versus the normal plantar response . 36 - crossed toe responses . 36 - tonic plantar flexion of the toes in hemiplegia 37 RIVAL SIGNS - confusion . 39 - different sites of excitation 39 - stretch reflexes of the toe muscles 41 - spontaneous or associated dorsiflexion of the great toe 42 - effects other than in the toes after plantar stimulation 42 THE PLANTAR RESPONSE IN INFANTS - contradictory findings 43 - the grasp reflex of the foot . -
Neuropsychiatry Block Spinal Cord Functions and Reflexes
NeuroPsychiatry Block Spinal Cord Functions and Reflexes By Laiche Djouhri, PhD Dept. of Physiology Email: [email protected] Ext:71044 NeuroPsychiatry Block/Week 1 Motor Functions of the Spinal Cord, The cord Reflexes Chapter 55 (Guyton & Hall) 2 Objectives By the end of this session students are expected to: . Appreciate the two-way traffic along the spinal cord . Describe some characteristics of spinal neuronal circuits . Classify reflexes and appreciate their clinical importance . Describe neuronal mechanisms of the 10withdrawal/6/2016 reflex & crossed extensor reflex3 The Spinal Cord (SC) . It is about 45 cm long and 2 cm in diameter 8 Cervical . It is composed of about 100 million neurons and even more neuroglia 12 Thoracic . It is continuous with the brain and together they make up the Lumbar CNS 5 Sacral 5 . 31 pairs of spinal nerves are connected to it 1 10/6/2016 Coccygeal 4 The Spinal Nerves . Each spinal nerve has a ventral root and a dorsal root . The dorsal (posterior) root contains afferent (sensory) nerve fibers, and their cell bodies are located in dorsal root ganglion (DRG). The ventral (anterior) root carries efferent (motor) fibers, and their cells bodies are located in the ventral horn of the spinal cord. Afferent fiber Efferent fiber (DRG) Each DRG has 1000s of cell bodies Spinal Cord Organization: 1. The Grey Matter . The structural organization of the SC can best be studied in a cross section of the cord which reveals: • An outer band of white matter surrounding • An inner core of grey matter (H shaped) which can be divided into 3 functional zones: 1. -
The Spinal Cord, Spinal Nerves, and Spinal Reflexes
12 The Spinal Cord, Spinal Nerves, and Spinal Reflexes Lecture Presentation by Lori Garrett © 2018 Pearson Education, Inc. Section 1: Functional Organization of the Spinal Cord Learning Outcomes 12.1 Describe how the spinal cord can function without input from the brain. 12.2 Discuss the anatomical features of the spinal cord. 12.3 Describe the three meningeal layers that surround the spinal cord. 12.4 Explain the roles of gray matter and white matter in processing and relaying sensory information and motor commands. © 2018 Pearson Education, Inc. Section 1: Functional Organization of the Spinal Cord Learning Outcomes (continued) 12.5 Describe the major components of a spinal nerve. 12.6 Describe the rami associated with spinal nerves. 12.7 Relate the distribution pattern of spinal nerves to the region they innervate. 12.8 Describe the cervical plexus. 12.9 Relate the distribution pattern of the brachial plexus to its function. 12.10 Relate the distribution patterns of the lumbar plexus and sacral plexus to their functions. © 2018 Pearson Education, Inc. Module 12.1: The spinal cord can function independently from the brain © 2018 Pearson Education, Inc. Module 12.1: The brain and spinal cord Both the brain and the spinal cord: . Receive sensory input from receptors . Contain reflex centers . Send motor output to effectors Reflex . Rapid, automatic response triggered by specific stimuli Spinal reflexes . Controlled in the spinal cord . Function without input from the brain © 2018 Pearson Education, Inc. Module 12.1: Review A. Describe the direction of sensory input and motor commands relative to the spinal cord. B. -

Questions for Exam 2012
BIOLOGICAL PSYCHOLOGY I (2012 sec 003) MIDTERM EXAM 3A (Thursday, Nov. 12, 2009) Mark the ONE BEST letter choice (either A, B, C, D, or E) on the computer-graded sheet in NUMBER TWO PENCIL. If you need to erase, do so completely! You MUST use the answer sheet provided by us inside your exam packet. No other answer sheet will be allowed. TAKE A DEEP BREATH – TAKE YOUR TIME, READ ALL QUESTIONS AND ANSWERS CAREFULLY - GOOD LUCK!!! 1. The calcium necessary for the interaction between actin and myosin filaments during muscle contraction is released from: a) the motor neurons presynaptic terminals. b) the sarcoplasmic reticulum. c) the actin filaments. d) myosin filaments. e) the synaptic vesicles. 2. In the early pioneering studies of sleep, which region, when electrically stimulated with a small electrode, would wake sleeping cats? a) the frontal cortex. b) the hippocampus. c) the basal ganglia. d) the ascending reticular activating system. e) medial forebrain bundle. 3. What is the correct sequence of the different stages of sleep experienced through the night, beginning when you fall asleep (numbers are the different stages of non-REM sleep)? a) 1, 2, 3, 4, REM, 4, 3, 2, 1 . b) REM, 1, 2, 3, 4 . c) 4, 3, 2, 1, 2, 3, 4, REM . d) 1, 2, 3, 4, 3, 2, 1, REM . e) 4, 3, 2, 1, REM, 1, 2, 3, 4 . 4. As part of a science-fair project in 1965, how long did Randy Gardner stay awake during his sleep deprivation experiment? a) 2 days. b) 5 days. -

Deep Tendon Reflexes
Reflex Physiology Dr. Ali Ebneshahidi © 2009 Ebneshahidi Reflex Physiology . Reflexes are automatic, subconscious response to changes within or outside the body. a. Reflexes maintain homeostasis (autonomic reflexes) – heart rate, breathing rate, blood pressure, and digestion. b. Reflexes also carry out the automatic action of swallowing, sneezing, coughing, and vomiting. c. Reflexes maintain balance & posture. ex. Spinal reflexes – control trunk and limb muscles. d. Brain reflexes – involve reflex center in brain stem. ex. Reflexes for eye movement. © 2009 Ebneshahidi Reflex Arc The reflex arc governs the operation of reflexes. Nerve impulses follow nerve pathways as they travel through the nervous system. The simplest of these pathways, including a few neurons, constitutes a reflex arc. Reflexes whose arc pass through the spinal cord are called spinal reflexes. © 2009 Ebneshahidi Parts of Reflex Arc . 1. Receptor – detects the stimulus. a) Description: the receptor end of a particular dendrite or a specialized receptor cell in a sensory organ. b) function: sensitive to a specific type of internal or external change. 2. sensory neuron – conveys the sensory info. to brain or spinal cord. a. Description: Dendrite, cell body, and axon of a sensory neuron. b. Function: transmit nerve impulses from the receptor into the brain or spinal cord. © 2009 Ebneshahidi Reflex Arc . 3. Interneuron: relay neurons. a. Description: dendrite, cell body, and axon of a neuron within the brain or spinal cord. b. function: serves as processing center, conducts nerve impulses from the sensory neuron to a motor neuron. 4. Motor neuron: conduct motor output to the periphery. a. Description: Dendrite, cell body, and axon of a motor neuron. -

I Order Neurons: Are Axons of Post
www.examrace.com1 Re www.examrace.com2 rcaiEI'Iセᄋ@ セエ@ www.examrace.com3 Reflex Action • Definition : It is an involuntary response to a peripheral stimulation • Sensory impulse is automatically converted into a motor effect • It forms the functional unit of nervous system • It depends on integrity of reflex arc www.examrace.com4 Reflex Arc Following components • An Afferent from a receptor • Synapse, may be one or many • An Efferent to effector organ www.examrace.com5 Receptors skin -Afferent neuron Efferent neuron Effector (muscle) www.examrace.com6 Classification: A: Clinical classification • Superficial • Deep or Tendon reflexes • Visceral: at least one part of reflex arc is formed by autonomic nerve eg. Pupillary reflex, carotid sinus reflex • Pathological eg. Babinski’s sign www.examrace.com7 B: Anatomical cl. • Segmental Reflexes: end of afferent & beginning of efferent neuron are in the same seg. of spinal cord • Intersegmental Reflex : here the end & beginning are in different seg. • Suprasegmental Reflex: centre for such reflex lies above the spinal cord www.examrace.com8 C: Inborn or Acquired • Conditioned or Acquired: are acquired after learning or training eg. Reflex salivation • Unconditioned or Inborn: present since birth eg. Salivation when an object is placed in mouth. www.examrace.com9 D: depending upon no. of Synapses • Monosynaptic • Bisynaptic • Polysynaptic E : physiological classification • Flexor reflex • Extensor re. www.examrace.com10 Monosynaptic Reflex Stretch Reflex or Myotatic Reflex Reflex Arc • Stimulus—Stretch to muscle • Receptor– Muscle spindle (gpIa & II fib) • Central conn.—On alpha motor neuron • Response—Contraction of same muscle • Central delay— 0.5 ms. ( one synapse) www.examrace.com11 Afferent Muscle nerve ceptor Motor neuron www.examrace.com12 Structure of receptor • Muscles have two types of fibers • Extrafusal fib.----contractile fib. -
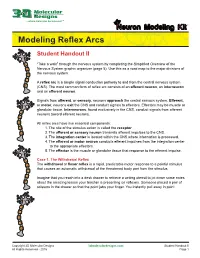
Modeling Reflex Arcs
Contents List ...where molecules become real TM euron Modeling Kit© Modeling Reflex Arcs Student Handout II “Take a walk” through the nervous system by completing the Simplified Overview of the Nervous System graphic organizer (page 5). Use this as a road map to the major divisions of the nervous system. A reflex arc is a simple signal conduction pathway to and from the central nervous system (CNS). The most common form of reflex arc consists of anafferent neuron, an interneuron and an efferent neuron. Signals from afferent, or sensory, neurons approach the central nervous system. Efferent, or motor, neurons exit the CNS and conduct signals to effectors. Effectors may be muscle or glandular tissue. Interneurons, found exclusively in the CNS, conduct signals from afferent neurons toward efferent neurons. All reflex arcs have five essential components: 1. The site of the stimulus action is called the receptor. 2. The afferent or sensory neuron transmits afferent impulses to the CNS. 3. The integration center is located within the CNS where information is processed. 4. The efferent or motor neuron conducts efferent impulses from the integration center to the appropriate effectors. 5. The effector is the muscle or glandular tissue that response to the efferent impulse. Case 1. The Withdrawal Reflex The withdrawal or flexor reflex is a rapid, predictable motor response to a painful stimulus that causes an automatic withdrawal of the threatened body part from the stimulus. Imagine that you reach into a desk drawer to retrieve a writing utensil to jot down some notes about the amazing lesson your teacher is presenting on reflexes.