Revised 11/25/2019 GEORGIA MEDICAID FEE-FOR-SERVICE
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer
diagnostics Review Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer Shunsuke Kato Department of Clinical Oncology, Juntendo University Graduate School of Medicine, 2-1-1, Hongo, Bunkyo-ku, Tokyo 113-8421, Japan; [email protected]; Tel.: +81-3-5802-1543 Abstract: The prognosis of patients with solid tumours has remarkably improved with the develop- ment of molecular-targeted drugs and immune checkpoint inhibitors. However, the improvements in the prognosis of pancreatic cancer and biliary tract cancer is delayed compared to other carcinomas, and the 5-year survival rates of distal-stage disease are approximately 10 and 20%, respectively. How- ever, a comprehensive analysis of tumour cells using The Cancer Genome Atlas (TCGA) project has led to the identification of various driver mutations. Evidently, few mutations exist across organs, and basket trials targeting driver mutations regardless of the primary organ are being actively conducted. Such basket trials not only focus on the gate keeper-type oncogene mutations, such as HER2 and BRAF, but also focus on the caretaker-type tumour suppressor genes, such as BRCA1/2, mismatch repair-related genes, which cause hereditary cancer syndrome. As oncogene panel testing is a vital approach in routine practice, clinicians should devise a strategy for improved understanding of the cancer genome. Here, the gene mutation profiles of pancreatic cancer and biliary tract cancer have been outlined and the current status of tumour-agnostic therapy in these cancers has been reported. Keywords: pancreatic cancer; biliary tract cancer; targeted therapy; solid tumours; driver mutations; agonist therapy Citation: Kato, S. Tumour-Agnostic Therapy for Pancreatic Cancer and 1. -
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
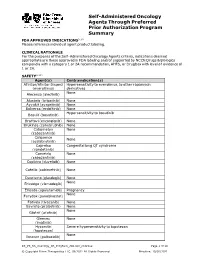
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

Pharmacy Pre-Authorization Criteria
PHARMACY PRE-AUTHORIZATION CRITERIA DRUG (S) Oncology Medications: Sprycel (dasatinib) Afinitor (everolimus) Stivarga (regorafenib) Caprelsa (vandetanib) Sutent (sunitinib) Gilotrif (afatinib dimaleate) Tarceva (erlotinob) Gleevec (imatinib mesylate) Temodar (temozolomide) Ibrance (palbociclib) Tepadina (thiotepa) Idhifa (enasidenib) Thalomid (thalidomide) Iressa (gefitinib) Vantas (histrelin acetate) Kisqali (ribociclib) Venclexta (venetoclax) Lenvima (lenvatinib) Verzenio (abemaciclib) Nerlynx (neratinib) Vidaza (azacitidine) Nexavar (sorafenib) Votrient (pazopanib) Ninlaro (ixazomib) Xalkori (crizotinib) Odomzo (sonidegib) Xeloda (capecitabine) Zydelig (idelalisib) Zykadia (certinib) Zytiga (abiraterone acetate) PHARMACY PRE-AUTHORIZATION CRITERIA POLICY # 21107 CRITERIA The above medications are covered when the following criteria are met: 1. Ordered by an oncologist or hematologist AND 2. All FDA Approved Indications OR 3. Chemo agent is listed in an accepted Compendia for treatment of cancer type, OR - National Comprehensive Cancer Network (NCCN) Drugs and Biologics Compendium, level of evidence 1, 2A, or 2B - Thomson Micromedex DrugDex - Chemo agent is recommended for cancer type in formal clinical studies published in at least 2 peer reviewed professional medical journals, published in the United States or Great Britain Coverage Duration: Initial: 3 months Continuation: 6 months. Afinitor, Gilotrif, Gleevec, Ibrance, Idhifa, Iressa, Kisqali, Lenvima, Nexavar, Ninlaro, Odomzo, Sprycel, Stivarga, Sutent, Tarceva, Temodar, Thalomid, -

211192Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 211192Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 211192 PDUFA Goal Date August 21, 2018 OSE RCM # 2017-2612; 2017-2614 Reviewer Name(s) Till Olickal, Ph.D., Pharm.D. Team Leader Elizabeth Everhart, MSN, RN, ACNP Division Director Cynthia LaCivita, Pharm.D. Review Completion Date June 6, 2018 Subject Review to determine if a REMS is necessary Established Name Ivosidenib Trade Name Tibsovo Name of Applicant Agios Pharmaceuticals, Inc. Therapeutic Class Isocitrate dehydrogenase-1 inhibitor Formulation(s) 250 mg tablet Dosing Regimen 500 mg orally once daily until disease progression or unacceptable toxicity. 1 Reference ID: 4273770 Table of Contents EXECUTIVE SUMMARY ......................................................................................................................................................... 3 1 Introduction ..................................................................................................................................................................... 3 2 Background ...................................................................................................................................................................... 3 2.1 Product Information .......................................................................................................................................... -

Horizon Scanning Status Report June 2019
Statement of Funding and Purpose This report incorporates data collected during implementation of the Patient-Centered Outcomes Research Institute (PCORI) Health Care Horizon Scanning System, operated by ECRI Institute under contract to PCORI, Washington, DC (Contract No. MSA-HORIZSCAN-ECRI-ENG- 2018.7.12). The findings and conclusions in this document are those of the authors, who are responsible for its content. No statement in this report should be construed as an official position of PCORI. An intervention that potentially meets inclusion criteria might not appear in this report simply because the horizon scanning system has not yet detected it or it does not yet meet inclusion criteria outlined in the PCORI Health Care Horizon Scanning System: Horizon Scanning Protocol and Operations Manual. Inclusion or absence of interventions in the horizon scanning reports will change over time as new information is collected; therefore, inclusion or absence should not be construed as either an endorsement or rejection of specific interventions. A representative from PCORI served as a contracting officer’s technical representative and provided input during the implementation of the horizon scanning system. PCORI does not directly participate in horizon scanning or assessing leads or topics and did not provide opinions regarding potential impact of interventions. Financial Disclosure Statement None of the individuals compiling this information have any affiliations or financial involvement that conflicts with the material presented in this report. Public Domain Notice This document is in the public domain and may be used and reprinted without special permission. Citation of the source is appreciated. All statements, findings, and conclusions in this publication are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI) or its Board of Governors. -

209606Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209606Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA Multidisciplinary Review and Evaluation Application Number(s) NDA 209606 Application Type Original 505(b)(1) Priority or Standard Priority Submit Date(s) December 30, 2016 Received Date(s) December 30, 2016 PDUFA Goal Date August 30, 2017 Division/Office DHP/OHOP Review Completion Date July 28, 2017 Applicant Celgene Corporation Established Name Enasidenib (Proposed) Trade Name IDHIFA® Pharmacologic Class Isocitrate dehydrogenase 2 inhibitor Formulation(s) Tablets, 50mg and 100mg Dosing Regimen 100 mg once daily Applicant Proposed IDHIFA is indicated for the treatment of patients with relapsed or Indication(s)/Population(s) refractory acute myeloid leukemia with an IDH2 mutation Recommendation on Regular approval Regulatory Action Recommended IDHIFA is an isocitrate dehydrogenase-2 inhibitor indicated for the Indication(s)/Population(s) treatment of adult patients with relapsed or refractory acute myeloid leukemia with an isocitrate dehydrogenase-2 mutation as detected by an FDA-approved test. Reference ID: 4131433 Multidisciplinary Review and Evaluation NDA 209606 IDHIFA® (enasidenib) Table of Contents Table of Contents ........................................................................................................................... 2 Table of Tables .............................................................................................................................. -

Enasidenib Drives Human Erythroid Differentiation Independently of Isocitrate Dehydrogenase 2
The Journal of Clinical Investigation CONCISE COMMUNICATION Enasidenib drives human erythroid differentiation independently of isocitrate dehydrogenase 2 Ritika Dutta,1,2 Tian Yi Zhang,1,2 Thomas Köhnke,1 Daniel Thomas,1 Miles Linde,1 Eric Gars,1 Melissa Stafford,1 Satinder Kaur,1 Yusuke Nakauchi,1 Raymond Yin,1 Armon Azizi,1 Anupama Narla,3 and Ravindra Majeti1,2 1Department of Medicine, Division of Hematology, Cancer Institute, and Institute for Stem Cell Biology and Regenerative Medicine, Stanford University, Stanford, California, USA. 2Stanford School of Medicine, Stanford, California, USA. 3Department of Pediatrics, Division of Hematology/Oncology, Stanford University, Stanford, California, USA. Cancer-related anemia is present in more than 60% of newly diagnosed cancer patients and is associated with substantial morbidity and high medical costs. Drugs that enhance erythropoiesis are urgently required to decrease transfusion rates and improve quality of life. Clinical studies have observed an unexpected improvement in hemoglobin and RBC transfusion- independence in patients with acute myeloid leukemia (AML) treated with the isocitrate dehydrogenase 2 (IDH2) mutant- specific inhibitor enasidenib, leading to improved quality of life without a reduction in AML disease burden. Here, we demonstrate that enasidenib enhanced human erythroid differentiation of hematopoietic progenitors. The phenomenon was not observed with other IDH1/2 inhibitors and occurred in IDH2-deficient CRISPR-engineered progenitors independently of D-2-hydroxyglutarate. The effect of enasidenib on hematopoietic progenitors was mediated by protoporphyrin accumulation, driving heme production and erythroid differentiation in committed CD71+ progenitors rather than hematopoietic stem cells. Our results position enasidenib as a promising therapeutic agent for improvement of anemia and provide the basis for a clinical trial using enasidenib to decrease transfusion dependence in a wide array of clinical contexts. -

Genetic Testing for Acute Myeloid Leukemia AHS-M2062
Corporate Medical Policy Genetic Testing for Acute Myeloid Leukemia AHS-M2062 File Name: genetic_testing_for_acute_myeloid_leukemia Origination: 1/1/2019 Last CAP Review: 8/2021 Next CAP Review: 8/2022 Last Review: 8/2021 Description of Procedure or Service Acute myeloid leukemia (AML) is characterized by large numbers of abnormal, immature myeloid cells in the bone marrow and peripheral blood resulting from genetic changes in hematopoietic precursor cells which disrupt normal hematopoietic growth and differentiation (Stock, 2020). Related Policies: Genetic Cancer Susceptibility Using Next Generation Sequencing AHS-M2066 Molecular Panel Testing of Cancers to Identify Targeted Therapy AHS-M2109 Serum Tumor Markers for Malignancies AHS-G2124 Minimal Residual Disease (MRD) AHS- M2175 ***Note: This Medical Policy is complex and technical. For questions concerning the technical language and/or specific clinical indications for its use, please consult your physician. Policy BCBSNC will provide coverage for genetic testing for acute myeloid leukemia when it is determined to be medically necessary because the medical criteria and guidelines shown below are met. Benefits Application This medical policy relates only to the services or supplies described herein. Please refer to the Member's Benefit Booklet for availability of benefits. Member's benefits may vary according to benefit design; therefore member benefit language should be reviewed before applying the terms of this medical policy. When Genetic Testing for Acute Myeloid Leukemia is covered The use of genetic testing for acute myeloid leukemia is considered medically necessary for the following: A. Genetic testing for FLT3 internal tandem duplication and tyrosine kinase domain mutations (ITD and TKD), IDH1, IDH2, TET2, WT1, DNMT3A, ASXL1 and/or TP53 in adult and pediatric patients with suspected or confirmed AML of any type for prognostic and/or therapeutic purposes. -

Nanocarriers As Magic Bullets in the Treatment of Leukemia
nanomaterials Review Nanocarriers as Magic Bullets in the Treatment of Leukemia 1, 2, 1 2 Mohammad Houshmand y , Francesca Garello y , Paola Circosta , Rachele Stefania , Silvio Aime 2, Giuseppe Saglio 1 and Claudia Giachino 1,* 1 Department of Clinical and Biological Sciences, University of Torino, 10043 Torino, Italy; [email protected] (M.H.); [email protected] (P.C.); [email protected] (G.S.) 2 Molecular and Preclinical Imaging Centres, Department of Molecular Biotechnology and Health Sciences, University of Torino, 10126 Torino, Italy; [email protected] (F.G.); [email protected] (R.S.); [email protected] (S.A.) * Correspondence: [email protected] These authors contributed equally to this work. y Received: 23 December 2019; Accepted: 1 February 2020; Published: 6 February 2020 Abstract: Leukemia is a type of hematopoietic stem/progenitor cell malignancy characterized by the accumulation of immature cells in the blood and bone marrow. Treatment strategies mainly rely on the administration of chemotherapeutic agents, which, unfortunately, are known for their high toxicity and side effects. The concept of targeted therapy as magic bullet was introduced by Paul Erlich about 100 years ago, to inspire new therapies able to tackle the disadvantages of chemotherapeutic agents. Currently, nanoparticles are considered viable options in the treatment of different types of cancer, including leukemia. The main advantages associated with the use of these nanocarriers summarized as follows: i) they may be designed to target leukemic cells selectively; ii) they invariably enhance bioavailability and blood circulation half-life; iii) their mode of action is expected to reduce side effects. -

Estimation of the Percentage of US Patients with Cancer Who Benefit from Genome‐Driven Oncology
Supplementary Online Content Marquart J, Chen EY, Prasad V. Estimation of the percentage of US patients with cancer who benefit from genome‐driven oncology. JAMA Oncology. Published online April 17, 2018. doi:10.1001/jamaoncol.2018.1660 eAppendix 1. Yearly Cancer Statistics eAppendix 2. Data Sources by Malignancy eAppendix 3. Pie Charts Estimating Patients Eligible for Genomically Targeted Therapy eAppendix 4. Pie Charts Estimating Patients Who Could Benefit from Genomically Targeted Therapy eAppendix 5. Pie Charts Estimating Patients Eligible for Genomically Informed Therapy eAppendix 6. Pie Charts Estimating Patients Who Could Benefit from Genomically Informed Therapy eAppendix 7. Pie Charts Estimating Patients Eligible for and who could Benefit from Adjuvant Therapy eFigure 1. Percent of US metastatic Cancer Patients Who May be Eligible for and Benefit from Genomically Informed Treatment eFigure 2. Growth of Genome Targeted and Informed Therapy Over Time With Fitted Linear Regression This supplementary material has been provided by the authors to give readers additional information about their work. 1 © 2018 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/27/2021 eAppendix 1. Cancer Statistics by Year: 2006: https://www.ncbi.nlm.nih.gov/pubmed/16514137 2007: https://www-ncbi-nlm-nih-gov/pubmed/17237035 2008: https://www-ncbi-nlm-nih-gov/pubmed/18287387 2009: https://www-ncbi-nlm-nih-gov/pubmed/19474385 2010: https://www-ncbi-nlm-nih-gov/pubmed/20610543 2011: https://www.ncbi.nlm.nih.gov/pubmed/21685461 2012: https://www.ncbi.nlm.nih.gov/pubmed/22237781 2013: https://www.ncbi.nlm.nih.gov/pubmed/23335087 2014: https://www.ncbi.nlm.nih.gov/pubmed/24890451 2015: https://www.ncbi.nlm.nih.gov/pubmed/25559415 2016: https://www.ncbi.nlm.nih.gov/pubmed/26742998 2017: https://www.ncbi.nlm.nih.gov/pubmed/28055103 2018: https://www.ncbi.nlm.nih.gov/pubmed/29313949 eAppendix 2. -

Advances in the Treatment of Acute Myeloid Leukemia: New Drugs and New Challenges
Published OnlineFirst February 3, 2020; DOI: 10.1158/2159-8290.CD-19-1011 REVIEW Advances in the Treatment of Acute Myeloid Leukemia: New Drugs and New Challenges Nicholas J. Short , Marina Konopleva , Tapan M. Kadia , Gautam Borthakur , Farhad Ravandi , Courtney D. DiNardo , and Naval Daver ABSTRACT The therapeutic armamentarium of acute myeloid leukemia (AML) has rapidly expanded in the past few years, driven largely by translational research into its genomic landscape and an improved understanding of mechanisms of resistance to conventional thera- pies. However, primary and secondary drug resistance remains a substantial problem for most patients. Research into the mechanisms of resistance to these new agents is informing the development of the next class of AML drugs and the design of combination regimens aimed at optimally exploiting thera- peutic vulnerabilities, with the ultimate goal of eradicating all subclones of the disease and increasing cure rates in AML. Signifi cance: AML is a heterogeneous disease, characterized by a broad spectrum of molecular altera- tions that infl uence clinical outcomes and also provide potential targets for drug development. This review discusses the current and emerging therapeutic landscape of AML, highlighting novel classes of drugs and how our expanding knowledge of mechanisms of resistance are informing future therapies and providing new opportunities for effective combination strategies. INTRODUCTION importance of the apoptotic machinery in chemotherapy resistance and AML propagation has also led to the devel- Driven by intense basic and translational research, the opment of apoptosis-inducing therapies that appear to be past 10 to 15 years have greatly improved our understanding effi cacious irrespective of the presence or absence of targeta- of the pathobiology and genetic diversity of acute myeloid ble genetic mutations ( 6, 7 ). -

Manufacturer Patient Assistance Programs
Manufacturer Patient Assistance Programs * Provisional Bridging Programs August 2021 highlighted below in blue For medications currently not funded per the BC Cancer Benefit Drug List - http://www.bccancer.bc.ca/systemic-therapy-site/documents/policy%20and%20forms/benefit%20drug%20list.pdf Disclaimer: BC Cancer intends to keep the information on this document as up to date as possible but cannot guarantee that the programs are all available as listed. Contact your local Drug Access Navigator (DAN) for more information UPDATES: New MPAP/Compassionate Access Open: Abiraterone-JAMP, Abiraterone-Sandoz, Everolimus-Sandoz, Gefitinib-JAMP, Gefinitib-Sandoz, Imatinib-JAMP, Encorafenib (Braftovi), Binimetinib (Mektovi), Pralsetinib (Gavreto), Trastuzumab Deruxtecan (Enhertu) Provisional Bridging/Compassionate Access Closed: MPAP Closed: Additional Updates: Drug Manufacturer / PAP Name Contact Information Support Offered Route Strength DIN Abemaciclib (Verzenio) Lilly Phone 1.855.545.5922 Compassionate supply may be available PO 50mg 02487098 * Provisional Bridging Program Lilly Patient Support Program Fax 1.844.503.7749 Financial assistance for patients with or without private insurance may be available PO 100mg 02487101 Email [email protected] PO 150mg 02487128 Web PO 200mg 02487136 Abiraterone (Zytiga) Janssen Phone 1.844.511.2616 Compassionate supply may be available PO 250mg 02371065 * Provisional Bridging Program Janssen BioAdvance Patient Assistance Program Fax 1.855.629.7100 Financial assistance for patients with or without private