Actionable Targets by Tumor Genomic Profiling in Patients with Cholangiocarcinoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer
diagnostics Review Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer Shunsuke Kato Department of Clinical Oncology, Juntendo University Graduate School of Medicine, 2-1-1, Hongo, Bunkyo-ku, Tokyo 113-8421, Japan; [email protected]; Tel.: +81-3-5802-1543 Abstract: The prognosis of patients with solid tumours has remarkably improved with the develop- ment of molecular-targeted drugs and immune checkpoint inhibitors. However, the improvements in the prognosis of pancreatic cancer and biliary tract cancer is delayed compared to other carcinomas, and the 5-year survival rates of distal-stage disease are approximately 10 and 20%, respectively. How- ever, a comprehensive analysis of tumour cells using The Cancer Genome Atlas (TCGA) project has led to the identification of various driver mutations. Evidently, few mutations exist across organs, and basket trials targeting driver mutations regardless of the primary organ are being actively conducted. Such basket trials not only focus on the gate keeper-type oncogene mutations, such as HER2 and BRAF, but also focus on the caretaker-type tumour suppressor genes, such as BRCA1/2, mismatch repair-related genes, which cause hereditary cancer syndrome. As oncogene panel testing is a vital approach in routine practice, clinicians should devise a strategy for improved understanding of the cancer genome. Here, the gene mutation profiles of pancreatic cancer and biliary tract cancer have been outlined and the current status of tumour-agnostic therapy in these cancers has been reported. Keywords: pancreatic cancer; biliary tract cancer; targeted therapy; solid tumours; driver mutations; agonist therapy Citation: Kato, S. Tumour-Agnostic Therapy for Pancreatic Cancer and 1. -
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
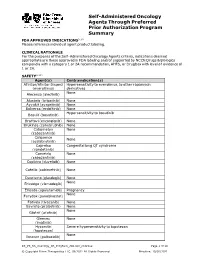
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

Pharmacy Pre-Authorization Criteria
PHARMACY PRE-AUTHORIZATION CRITERIA DRUG (S) Oncology Medications: Sprycel (dasatinib) Afinitor (everolimus) Stivarga (regorafenib) Caprelsa (vandetanib) Sutent (sunitinib) Gilotrif (afatinib dimaleate) Tarceva (erlotinob) Gleevec (imatinib mesylate) Temodar (temozolomide) Ibrance (palbociclib) Tepadina (thiotepa) Idhifa (enasidenib) Thalomid (thalidomide) Iressa (gefitinib) Vantas (histrelin acetate) Kisqali (ribociclib) Venclexta (venetoclax) Lenvima (lenvatinib) Verzenio (abemaciclib) Nerlynx (neratinib) Vidaza (azacitidine) Nexavar (sorafenib) Votrient (pazopanib) Ninlaro (ixazomib) Xalkori (crizotinib) Odomzo (sonidegib) Xeloda (capecitabine) Zydelig (idelalisib) Zykadia (certinib) Zytiga (abiraterone acetate) PHARMACY PRE-AUTHORIZATION CRITERIA POLICY # 21107 CRITERIA The above medications are covered when the following criteria are met: 1. Ordered by an oncologist or hematologist AND 2. All FDA Approved Indications OR 3. Chemo agent is listed in an accepted Compendia for treatment of cancer type, OR - National Comprehensive Cancer Network (NCCN) Drugs and Biologics Compendium, level of evidence 1, 2A, or 2B - Thomson Micromedex DrugDex - Chemo agent is recommended for cancer type in formal clinical studies published in at least 2 peer reviewed professional medical journals, published in the United States or Great Britain Coverage Duration: Initial: 3 months Continuation: 6 months. Afinitor, Gilotrif, Gleevec, Ibrance, Idhifa, Iressa, Kisqali, Lenvima, Nexavar, Ninlaro, Odomzo, Sprycel, Stivarga, Sutent, Tarceva, Temodar, Thalomid, -

Targeted Therapies in Advanced Cholangiocarcinoma: a Focus on FGFR Inhibitors
medicina Review Targeted Therapies in Advanced Cholangiocarcinoma: A Focus on FGFR Inhibitors Alessandro Rizzo Department of Experimental, Diagnostic and Specialty Medicine, S. Orsola-Malpighi University Hospital, 40138 Bologna, Italy; [email protected] Abstract: Despite advanced diseases continuing to be associated with grim prognoses, the past decade has witnessed the advent of several novel treatment options for cholangiocarcinoma (CCA) patients. In fact, CCA has emerged as a heterogeneous group of malignancies harboring potentially druggable mutations in approximately 50% of cases, and thus, molecularly targeted therapies have been actively explored in this setting. Among these, fibroblast growth factor receptor (FGFR) inhibitors have reported important results, as witnessed by the FDA approval of pemigatinib in previously treated metastatic CCA patients harboring FGFR2 fusion or other rearrangements. Herein, we provide an overview of available evidence on FGFR inhibitors in CCA, especially focusing on the development, pitfalls and challenges of emerging treatments in this setting. Keywords: FGFR; cholangiocarcinoma; targeted therapies; intrahepatic cholangiocarcinoma; pemi- gatinib 1. Introduction Citation: Rizzo, A. Targeted Cholangiocarcinoma (CCA) encompasses a group of heterogeneous, rare and aggres- Therapies in Advanced sive malignancies, including intrahepatic cholangiocarcinoma (iCCA) and extrahepatic Cholangiocarcinoma: A Focus on cholangiocarcinoma (eCCA), with the latter further subclassified into perihilar (pCCA) FGFR Inhibitors. Medicina 2021, 57, and distal (dCCA) cholangiocarcinoma [1–3]. CCAs account for approximately 3% of 458. https://doi.org/10.3390/ all gastrointestinal cancers worldwide and 10–15% of all primary liver tumors [4–6]. As medicina57050458 suggested by several studies, these subgroups of hepatobiliary tumors not only develop from different anatomical locations, but vary widely in terms of epidemiology, biology, Academic Editor: Zygmunt Warzecha prognosis, and etiology [7–9]. -

211192Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 211192Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 211192 PDUFA Goal Date August 21, 2018 OSE RCM # 2017-2612; 2017-2614 Reviewer Name(s) Till Olickal, Ph.D., Pharm.D. Team Leader Elizabeth Everhart, MSN, RN, ACNP Division Director Cynthia LaCivita, Pharm.D. Review Completion Date June 6, 2018 Subject Review to determine if a REMS is necessary Established Name Ivosidenib Trade Name Tibsovo Name of Applicant Agios Pharmaceuticals, Inc. Therapeutic Class Isocitrate dehydrogenase-1 inhibitor Formulation(s) 250 mg tablet Dosing Regimen 500 mg orally once daily until disease progression or unacceptable toxicity. 1 Reference ID: 4273770 Table of Contents EXECUTIVE SUMMARY ......................................................................................................................................................... 3 1 Introduction ..................................................................................................................................................................... 3 2 Background ...................................................................................................................................................................... 3 2.1 Product Information .......................................................................................................................................... -

New Horizons for Precision Medicine in Biliary Tract Cancers
Published OnlineFirst August 17, 2017; DOI: 10.1158/2159-8290.CD-17-0245 REVIEW New Horizons for Precision Medicine in Biliary Tract Cancers Juan W. Valle1,2, Angela Lamarca1, Lipika Goyal3, Jorge Barriuso1,4, and Andrew X. Zhu3 ABSTRACT Biliary tract cancers (BTC), including cholangiocarcinoma and gallbladder cancer, are poor-prognosis and low-incidence cancers, although the incidence of intrahe- patic cholangiocarcinoma is rising. A minority of patients present with resectable disease but relapse rates are high; benefit from adjuvant capecitabine chemotherapy has been demonstrated.Cisplatin/ gemcitabine combination chemotherapy has emerged as the reference first-line treatment regimen; there is no standard second-line therapy. Selected patients may be suitable for liver-directed therapy (e.g., radioembolization or external beam radiation), pending confirmation of benefit in randomized studies. Initial trials targeting the epithelial growth factor receptor and angiogenesis pathways have failed to deliver new treatments. Emerging data from next-generation sequencing analyses have iden- tified actionable mutations (e.g.,FGFR fusion rearrangements and IDH1 and IDH2 mutations), with several targeted drugs entering clinical development with encouraging results. The role of systemic therapies, including targeted therapies and immunotherapy for BTC, is rapidly evolving and is the sub- ject of this review. Significance: The authors address genetic drivers and molecular biology from a translational per- spective, in an intent to offer a clear view of the recent past, present, and future of BTC. The review describes a state-of-the-art update of the current status and future directions of research and therapy in advanced BTC. Cancer Discov; 7(9); 1–20. -

Horizon Scanning Status Report June 2019
Statement of Funding and Purpose This report incorporates data collected during implementation of the Patient-Centered Outcomes Research Institute (PCORI) Health Care Horizon Scanning System, operated by ECRI Institute under contract to PCORI, Washington, DC (Contract No. MSA-HORIZSCAN-ECRI-ENG- 2018.7.12). The findings and conclusions in this document are those of the authors, who are responsible for its content. No statement in this report should be construed as an official position of PCORI. An intervention that potentially meets inclusion criteria might not appear in this report simply because the horizon scanning system has not yet detected it or it does not yet meet inclusion criteria outlined in the PCORI Health Care Horizon Scanning System: Horizon Scanning Protocol and Operations Manual. Inclusion or absence of interventions in the horizon scanning reports will change over time as new information is collected; therefore, inclusion or absence should not be construed as either an endorsement or rejection of specific interventions. A representative from PCORI served as a contracting officer’s technical representative and provided input during the implementation of the horizon scanning system. PCORI does not directly participate in horizon scanning or assessing leads or topics and did not provide opinions regarding potential impact of interventions. Financial Disclosure Statement None of the individuals compiling this information have any affiliations or financial involvement that conflicts with the material presented in this report. Public Domain Notice This document is in the public domain and may be used and reprinted without special permission. Citation of the source is appreciated. All statements, findings, and conclusions in this publication are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI) or its Board of Governors. -

209606Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209606Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA Multidisciplinary Review and Evaluation Application Number(s) NDA 209606 Application Type Original 505(b)(1) Priority or Standard Priority Submit Date(s) December 30, 2016 Received Date(s) December 30, 2016 PDUFA Goal Date August 30, 2017 Division/Office DHP/OHOP Review Completion Date July 28, 2017 Applicant Celgene Corporation Established Name Enasidenib (Proposed) Trade Name IDHIFA® Pharmacologic Class Isocitrate dehydrogenase 2 inhibitor Formulation(s) Tablets, 50mg and 100mg Dosing Regimen 100 mg once daily Applicant Proposed IDHIFA is indicated for the treatment of patients with relapsed or Indication(s)/Population(s) refractory acute myeloid leukemia with an IDH2 mutation Recommendation on Regular approval Regulatory Action Recommended IDHIFA is an isocitrate dehydrogenase-2 inhibitor indicated for the Indication(s)/Population(s) treatment of adult patients with relapsed or refractory acute myeloid leukemia with an isocitrate dehydrogenase-2 mutation as detected by an FDA-approved test. Reference ID: 4131433 Multidisciplinary Review and Evaluation NDA 209606 IDHIFA® (enasidenib) Table of Contents Table of Contents ........................................................................................................................... 2 Table of Tables .............................................................................................................................. -

Enasidenib Drives Human Erythroid Differentiation Independently of Isocitrate Dehydrogenase 2
The Journal of Clinical Investigation CONCISE COMMUNICATION Enasidenib drives human erythroid differentiation independently of isocitrate dehydrogenase 2 Ritika Dutta,1,2 Tian Yi Zhang,1,2 Thomas Köhnke,1 Daniel Thomas,1 Miles Linde,1 Eric Gars,1 Melissa Stafford,1 Satinder Kaur,1 Yusuke Nakauchi,1 Raymond Yin,1 Armon Azizi,1 Anupama Narla,3 and Ravindra Majeti1,2 1Department of Medicine, Division of Hematology, Cancer Institute, and Institute for Stem Cell Biology and Regenerative Medicine, Stanford University, Stanford, California, USA. 2Stanford School of Medicine, Stanford, California, USA. 3Department of Pediatrics, Division of Hematology/Oncology, Stanford University, Stanford, California, USA. Cancer-related anemia is present in more than 60% of newly diagnosed cancer patients and is associated with substantial morbidity and high medical costs. Drugs that enhance erythropoiesis are urgently required to decrease transfusion rates and improve quality of life. Clinical studies have observed an unexpected improvement in hemoglobin and RBC transfusion- independence in patients with acute myeloid leukemia (AML) treated with the isocitrate dehydrogenase 2 (IDH2) mutant- specific inhibitor enasidenib, leading to improved quality of life without a reduction in AML disease burden. Here, we demonstrate that enasidenib enhanced human erythroid differentiation of hematopoietic progenitors. The phenomenon was not observed with other IDH1/2 inhibitors and occurred in IDH2-deficient CRISPR-engineered progenitors independently of D-2-hydroxyglutarate. The effect of enasidenib on hematopoietic progenitors was mediated by protoporphyrin accumulation, driving heme production and erythroid differentiation in committed CD71+ progenitors rather than hematopoietic stem cells. Our results position enasidenib as a promising therapeutic agent for improvement of anemia and provide the basis for a clinical trial using enasidenib to decrease transfusion dependence in a wide array of clinical contexts. -

Current and Novel Therapeutic Opportunities for Systemic Therapy in Biliary Cancer
www.nature.com/bjc REVIEW ARTICLE Current and novel therapeutic opportunities for systemic therapy in biliary cancer José J. G. Marin1,2, Maria Giuseppina Prete3,4, Angela Lamarca5,6, Simona Tavolari7, Ana Landa-Magdalena8, Giovanni Brandi9, Oreste Segatto10, Arndt Vogel11, Rocío I. R. Macias1,2, Pedro M. Rodrigues8, Adelaida La Casta8, Joachim Mertens12, Cecilia M. P. Rodrigues13, Maite G. Fernandez-Barrena14, Ana Da Silva Ruivo15, Marco Marzioni16, Giulia Mentrasti16, Pilar Acedo17, Patricia Munoz-Garrido18, Vincenzo Cardinale19, Jesus M. Banales2,8,20, Juan W. Valle 5,6, John Bridgewater 21, Chiara Braconi 3, on behalf of the working group 6 of the COST-action 18122 (Euro-Cholangio-NET) as part of the European Network for the study of Cholangiocarcinoma (ENSCCA) Biliary tract cancers (BTCs) are a group of rare and aggressive malignancies that arise in the biliary tree within and outside the liver. Beyond surgical resection, which is beneficial for only a small proportion of patients, current strategies for treating patients with BTCs include chemotherapy, as a single agent or combination regimens, in the adjuvant and palliative setting. Increased characterisation of the molecular landscape of these tumours has facilitated the identification of molecular vulnerabilities, such as IDH mutations and FGFR fusions, that can be exploited for the treatment of BTC patients. Beyond targeted therapies, active research avenues explore the development of novel therapeutics that target the crosstalk between cancer and stroma, the cellular pathways involved in the regulation of cell death, the chemoresistance phenotype and the dysregulation of RNA. In this review, we discuss the therapeutic opportunities currently available in the management of BTC patients, and explore the strategies that can support the implementation of precision oncology in BTCs, including novel molecular targets, liquid biopsies and patient-derived predictive tools. -
A Phase II Study of Infigratinib (BGJ398)
A phase II study of infigratinib (BGJ398), an FGFR-selective tyrosine kinase inhibitor (TKI), in patients with previously-treated advanced cholangiocarcinoma containing FGFR2 fusions Javle M,1 Kelley RK,2 Roychowdhury S,3 Weiss K-H,4 Abou-Alfa GK,5 Macarulla T,6 Sadeghi S,7 Waldschmidt D,8 Zhu A,9 Goyal L,9 Borad M,10 Yong WP,11 Borbath I,12 El-Khoueiry A,13 Philip P,14 Moran S,15 Ye Y,15 Ising M,16 Lewis N,17 Bekaii-Saab T10 1MD Anderson Cancer Center, Houston, TX, USA; 2University of California, San Francisco, CA, USA; 3Ohio State Comprehensive Cancer Center/James Cancer Hospital, Columbus, OH, USA; 4University Hospital Heidelberg, Germany; 5Memorial Sloan Kettering Cancer Center, New York, NY, USA; 6Hospital Vall d’Hebron, Barcelona, Spain; 7University of California, Los Angeles, CA, USA; 8Klinikum de Universität zu Köln, Cologne, Germany; 9Massachusetts General Hospital, Boston, MA, USA; 10Mayo Clinic Arizona, Scottsdale, AZ, USA; 11National University Cancer Institute, Singapore; 12Cliniques Universitaires St Luc Bruxelles, Brussels, Belgium; 13USC/Kenneth Norris Comprehensive Cancer Center, Los Angeles, CA, USA; 14Karmanos Cancer Institute, Detroit, MI, USA; 15QED Therapeutics, San Francisco, CA, USA; 16Novartis, Florham Park, NJ, USA; 17Novartis Pharmaceutical Corporation, East Hanover, NJ, USA #LBA28 Background Treatment Figure 2. Open-label, phase II study design Figure 3. Efficacy of infigratinib in FGFR2 fusion-positive Table 4. Infigratinib safety profile: any grade AEs ≥20% cholangiocarcinoma Number of patients (%) Any grade Grade 3/4 ■ Patients received infigratinib 125 mg once daily for 21 days followed 100 Hyperphosphatemia 52 (73.2) 9 (12.7) ■ Cholangiocarcinomas are often diagnosed at an advanced FGFR2 Amplification + Fusion by 7 days off in 28-day cycles. -

Revised 11/25/2019 GEORGIA MEDICAID FEE-FOR-SERVICE
GEORGIA MEDICAID FEE-FOR-SERVICE ONCOLOGY, ORAL - HEMATOLOGIC PA SUMMARY Preferred Non-Preferred Bosulif (bosutinib) Purixan (mercaptopurine suspension) Calquence (acalabrutinib) Farydak (panobinostat) Iclusig (ponatinib) Idhifa (enasidenib) Imbruvica (ibrutinib) Mercaptopurine tablets generic* Ninlaro (ixazomib) Pomalyst (pomalidomide) Revlimid (lenalidomide)* Rydapt (midostaurin) Sprycel (dasatinib) Tasigna (nilotinib) Thalomid (thalidomide)* Venclexta (venetoclax) Xpovio (selinexor) Zolinza (vorinosta) Zydelig (idelalisib) *PA not required LENGTH OF AUTHORIZATION: 1 Year NOTES: ▪ Mercaptopurine generic, Revlimid and Thalomid do not require prior authorization. ▪ Special consideration taken for members with stage IV advanced metastatic cancer. PA CRITERIA: Bosulif ❖ Approvable for members with a diagnosis of chronic-phase Philadelphia chromosome- positive (Ph+) chronic myelogenous leukemia (CML). ❖ Approvable for members with a diagnosis of accelerated- or blast-phase Ph+ CML who are resistant or intolerant to imatinib (Gleevec), dasatinib (Sprycel) or nilotinib (Tasigna). ❖ Approvable for members with a diagnosis of Ph+ acute lymphoblastic leukemia (ALL) who are resistant or intolerant to imatinib (Gleevec), dasatinib (Sprycel) or nilotinib (Tasigna). Calquence ❖ Approvable for members with a diagnosis of mantle cell lymphoma (MCL) who have received at least one prior therapy. Farydak ❖ Approvable for members with a diagnosis of multiple myeloma who have been previously treated with at least 2 prior therapies, including bortezomib (Velcade) and an Revised 11/25/2019 immunomodulatory agent (lenalidomide [Revlimid], thalidomide [Thalomid], pomalidomide [Pomalyst]) ❖ Farydak must be given in combination with bortezomib (Velcade) and dexamethasone, with lenalidomide (Revlimid) and dexamethasone or with carfilzomib [Kyprolis]. Iclusig ❖ Approvable for members with a diagnosis of chronic (not newly diagnosed), accelerated or blast-phase CML who are resistant or intolerant to imatinib (Gleevec), bosutinib (Bosulif), dasatinib (Sprycel) and nilotinib (Tasigna).