Nanocarriers As Magic Bullets in the Treatment of Leukemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Phase II Study of the Novel Proteasome Inhibitor Bortezomib In
Memorial Sloan-Kettering Cance r Center IRB Protocol IRB#: 05-103 A(14) A Phase II Study of the Novel Proteas ome Inhibitor Bortezomib in Combination with Rituximab, Cyclophosphamide and Prednisone in Patients with Relapsed/Refractory I Indolent B-cell Lymphoproliferative Disorders and Mantle Cell Lymphoma (MCL) MSKCC THERAPEUTIC/DIAGNOSTIC PROTOCOL Principal Investigator: John Gerecitano, M.D., Ph.D. Co-Principal Carol Portlock, M.D. Investigator(s): IFormerly: A Phase I/II Study of the Nove l Proteasome Inhibitor Bortezomib in Combinati on with Rituximab, Cyclophosphamide and Prednisone in Patients with Relapsed/Refractory Indolent B-cell Lymphoproliferative Disorders and Mantle Cell Lymphoma (MCL) Amended: 07/25/12 Memorial Sloan-Kettering Cance r Center IRB Protocol IRB#: 05-103 A(14) Investigator(s): Paul Hamlin, M.D. Commack, NY Steven B. Horwitz, M.D. Philip Schulman, M.D. Alison Moskowitz, M.D. Stuart Lichtman, M.D Craig H. Moskowitz, M.D. Stefan Berger, M.D. Ariela Noy, M.D. Julie Fasano, M.D. M. Lia Palomba, M.D., Ph.D. John Fiore, M.D. Jonathan Schatz, M.D. Steven Sugarman, M.D David Straus, M.D. Frank Y. Tsai, M.D. Andrew D. Zelenetz, M.D., Ph.D. Matthew Matasar, M.D Rockville Center, NY Mark L. Heaney, M.D., Ph.D. Pamela Drullinksy, M.D Nicole Lamanna, M.D. Arlyn Apollo, M.D. Zoe Goldberg, M.D. Radiology Kenneth Ng, M.D. Otilia Dumitrescu, M.D. Tiffany Troso-Sandoval, M.D. Andrei Holodny, M.D. Sleepy Hollow, NY Nuclear Medicine Philip Caron, M.D. Heiko Schoder, M.D. Michelle Boyar, M.D. -

(12) United States Patent (10) Patent No.: US 8,580,814 B2 Adelman Et Al
USOO858O814B2 (12) United States Patent (10) Patent No.: US 8,580,814 B2 Adelman et al. (45) Date of Patent: *Nov. 12, 2013 (54) METHODS OF USING 5,528,823. A 6/1996 Rudy, Jr. et al. (+)-1,4-DIHYDRO-7-(3S4S)-3-METHOXY-4- 3.43wk A E. E. St.Ola tala (METHYLAMINO)-1-PYRROLIDINYL-4- 6,171,857 B1 1/2001 Hendrickson OXO-1-(2-THIAZOLYL)-1.8- 6,291643 B1 9/2001 Zou et al. NAPHTHYRIDNE-3-CARBOXYLIC ACID 6,570,002 B1 5/2003 Hardwicket al. FORTREATMENT OF CANCER 6,641,810 B2 11/2003 Gold 6,641,833 B2 * 1 1/2003 Dang ............................ 424/426 (75) Inventors: Daniel CAdelman, Redwood City, CA 6,696,4836,670,144 B2B1 12/20032/2004 CraigSingh et al. (US); Jeffrey A. Silverman, 6,723,734 B2 4/2004 Kim et al. Burlingame, CA (US) 7,211,562 B2 5/2007 Rosen et al. 7.989,468 B2 * 8/2011 Adelman et al. .............. 514,300 (73) Assignee: Sunesis Pharmaceuticals, Inc., South 3.9. A. S. idaran-Ghera Gh et al.1 San Francisco, CA (US) 2003/0232334 A1* 12/2003 Morris et al. ..................... 435/6 c - r 2004/0106605 A1 6/2004 Carboni et al. .... 514/226.8 (*) Notice: Subject to any disclaimer, the term of this 2004/0132825 A1* 7/2004 Bacopoulos et al. ......... 514/575 patent is extended or adjusted under 35 2005/0203120 A1 9, 2005 Adelman et al. U.S.C. 154(b) by 201 days. 2005/0215583 A1 9, 2005 Arkin et al. 2006, OO25437 A1 2/2006 Adelman et al. -

Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer
diagnostics Review Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer Shunsuke Kato Department of Clinical Oncology, Juntendo University Graduate School of Medicine, 2-1-1, Hongo, Bunkyo-ku, Tokyo 113-8421, Japan; [email protected]; Tel.: +81-3-5802-1543 Abstract: The prognosis of patients with solid tumours has remarkably improved with the develop- ment of molecular-targeted drugs and immune checkpoint inhibitors. However, the improvements in the prognosis of pancreatic cancer and biliary tract cancer is delayed compared to other carcinomas, and the 5-year survival rates of distal-stage disease are approximately 10 and 20%, respectively. How- ever, a comprehensive analysis of tumour cells using The Cancer Genome Atlas (TCGA) project has led to the identification of various driver mutations. Evidently, few mutations exist across organs, and basket trials targeting driver mutations regardless of the primary organ are being actively conducted. Such basket trials not only focus on the gate keeper-type oncogene mutations, such as HER2 and BRAF, but also focus on the caretaker-type tumour suppressor genes, such as BRCA1/2, mismatch repair-related genes, which cause hereditary cancer syndrome. As oncogene panel testing is a vital approach in routine practice, clinicians should devise a strategy for improved understanding of the cancer genome. Here, the gene mutation profiles of pancreatic cancer and biliary tract cancer have been outlined and the current status of tumour-agnostic therapy in these cancers has been reported. Keywords: pancreatic cancer; biliary tract cancer; targeted therapy; solid tumours; driver mutations; agonist therapy Citation: Kato, S. Tumour-Agnostic Therapy for Pancreatic Cancer and 1. -
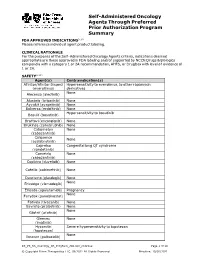
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

Pharmacy Pre-Authorization Criteria
PHARMACY PRE-AUTHORIZATION CRITERIA DRUG (S) Oncology Medications: Sprycel (dasatinib) Afinitor (everolimus) Stivarga (regorafenib) Caprelsa (vandetanib) Sutent (sunitinib) Gilotrif (afatinib dimaleate) Tarceva (erlotinob) Gleevec (imatinib mesylate) Temodar (temozolomide) Ibrance (palbociclib) Tepadina (thiotepa) Idhifa (enasidenib) Thalomid (thalidomide) Iressa (gefitinib) Vantas (histrelin acetate) Kisqali (ribociclib) Venclexta (venetoclax) Lenvima (lenvatinib) Verzenio (abemaciclib) Nerlynx (neratinib) Vidaza (azacitidine) Nexavar (sorafenib) Votrient (pazopanib) Ninlaro (ixazomib) Xalkori (crizotinib) Odomzo (sonidegib) Xeloda (capecitabine) Zydelig (idelalisib) Zykadia (certinib) Zytiga (abiraterone acetate) PHARMACY PRE-AUTHORIZATION CRITERIA POLICY # 21107 CRITERIA The above medications are covered when the following criteria are met: 1. Ordered by an oncologist or hematologist AND 2. All FDA Approved Indications OR 3. Chemo agent is listed in an accepted Compendia for treatment of cancer type, OR - National Comprehensive Cancer Network (NCCN) Drugs and Biologics Compendium, level of evidence 1, 2A, or 2B - Thomson Micromedex DrugDex - Chemo agent is recommended for cancer type in formal clinical studies published in at least 2 peer reviewed professional medical journals, published in the United States or Great Britain Coverage Duration: Initial: 3 months Continuation: 6 months. Afinitor, Gilotrif, Gleevec, Ibrance, Idhifa, Iressa, Kisqali, Lenvima, Nexavar, Ninlaro, Odomzo, Sprycel, Stivarga, Sutent, Tarceva, Temodar, Thalomid, -

211192Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 211192Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 211192 PDUFA Goal Date August 21, 2018 OSE RCM # 2017-2612; 2017-2614 Reviewer Name(s) Till Olickal, Ph.D., Pharm.D. Team Leader Elizabeth Everhart, MSN, RN, ACNP Division Director Cynthia LaCivita, Pharm.D. Review Completion Date June 6, 2018 Subject Review to determine if a REMS is necessary Established Name Ivosidenib Trade Name Tibsovo Name of Applicant Agios Pharmaceuticals, Inc. Therapeutic Class Isocitrate dehydrogenase-1 inhibitor Formulation(s) 250 mg tablet Dosing Regimen 500 mg orally once daily until disease progression or unacceptable toxicity. 1 Reference ID: 4273770 Table of Contents EXECUTIVE SUMMARY ......................................................................................................................................................... 3 1 Introduction ..................................................................................................................................................................... 3 2 Background ...................................................................................................................................................................... 3 2.1 Product Information .......................................................................................................................................... -

Preclinical Pharmacologic Evaluation of Pralatrexate and Romidepsin
Published OnlineFirst February 12, 2015; DOI: 10.1158/1078-0432.CCR-14-2249 Cancer Therapy: Preclinical Clinical Cancer Research Preclinical Pharmacologic Evaluation of Pralatrexate and Romidepsin Confirms Potent Synergy of the Combination in a Murine Model of Human T-cell Lymphoma Salvia Jain1, Xavier Jirau-Serrano2, Kelly M. Zullo2, Luigi Scotto2, Carmine F. Palermo3,4, Stephen A. Sastra3,4,5, Kenneth P. Olive3,4,5, Serge Cremers3, Tiffany Thomas3,YingWei6, Yuan Zhang6, Govind Bhagat3, Jennifer E. Amengual2, Changchun Deng2, Charles Karan8, Ronald Realubit8, Susan E. Bates9, and Owen A. O'Connor2 Abstract Purpose: T-cell lymphomas (TCL) are aggressive diseases, NOG mouse model of TCL were used to explore the in vitro and in which carry a poor prognosis. The emergence of new drugs for vivo activity of pralatrexate and romidepsin in combination. TCL has created a need to survey these agents in a rapid and Corresponding mass spectrometry–based pharmacokinetic and reproducible fashion, to prioritize combinations which should be immunohistochemistry-based pharmacodynamic analyses of prioritized for clinical study. Mouse models of TCL that can be xenograft tumors were performed to better understand a mech- used for screening novel agents and their combinations are anistic basis for the drug:drug interaction. lacking. Developments in noninvasive imaging modalities, such Results: In vitro, pralatrexate and romidepsin exhibited con- as surface bioluminescence (SBL) and three-dimensional ultra- centration-dependent synergism in combination against a panel sound (3D-US), are challenging conventional approaches in of TCL cell lines. In a NOG murine model of TCL, the combination xenograft modeling relying on caliper measurements. The recent of pralatrexate and romidepsin exhibited enhanced efficacy com- approval of pralatrexate and romidepsin creates an obvious pared with either drug alone across a spectrum of tumors using combination that could produce meaningful activity in TCL, complementary imaging modalities, such as SBL and 3D-US. -

ASTRO Bone Metastases Guideline-Full Version
1 Palliative Radiotherapy for Bone Metastases: An ASTRO Evidence-Based Guideline Stephen T. Lutz, M.D.,* Lawrence B. Berk, M.D., Ph.D.,† Eric L. Chang, M.D.,‡ Edward Chow, M.B.B.S.,§ Carol A. Hahn, M.D.,║ Peter J. Hoskin, M.D.,¶ David D. Howell, M.D.,# Andre A. Konski, M.D.,** Lisa A. Kachnic, M.D.,†† Simon S. Lo, M.B. ChB,§§ Arjun Sahgal, M.D.,║║ Larry N. Silverman, M.D.,¶¶ Charles von Gunten, M.D., Ph.D., FACP,## Ehud Mendel, M.D., FACS,*** Andrew D. Vassil, M.D.,††† Deborah Watkins Bruner, R.N., Ph.D.,‡‡‡ and William F. Hartsell, M.D.§§§ * Department of Radiation Oncology, Blanchard Valley Regional Cancer Center, Findlay, Ohio; † Department of Radiation Oncology, Moffitt Cancer Center, Tampa, Florida; ‡ Department of Radiation Oncology, The University of Texas MD Anderson Cancer Center, Houston, Texas; § Department of Radiation Oncology, Sunnybrook Odette Cancer Center, University of Toronto, Toronto, Ontario, Canada; ║ Department of Radiation Oncology, Duke University, Durham, North Carolina; ¶ Mount Vernon Centre for Cancer Treatment, Middlesex, UK; # Department of Radiation Oncology, University of Michigan, Mt. Pleasant, Michigan; ** Department of Radiation Oncology, Wayne State University, Detroit, Michigan; †† Department of Radiation Oncology, Boston Medical Center, Boston, Massachusetts; §§ Department of Radiation Oncology, Ohio State University, Columbus, Ohio; ║║ Department of Radiation Oncology, Sunnybrook Odette Cancer Center and the Princess Margaret Hospital, University of Toronto, Toronto, Ontario, Canada; ¶¶ 21st Century Oncology, Sarasota, Florida; ## The Institute for Palliative Medicine, San Diego Hospice, San Diego, California; *** Neurological Surgery, Ohio State University, Columbus, Ohio; ††† Department of Radiation Oncology, The Cleveland Clinic 2 Foundation, Cleveland, Ohio; ‡‡‡ School of Nursing, University of Pennsylvania, Philadelphia, Pennsylvania; §§§ Department of Radiation Oncology, Good Samaritan Cancer Center, Downers Grove, Illinois Reprint requests to: Stephen Lutz, M.D., 15990 Medical Drive South, Findlay, OH 45840. -

Cstone Pharmaceuticals 基石藥業
Hong Kong Exchanges and Clearing Limited and The Stock Exchange of Hong Kong Limited take no responsibility for the contents of this announcement, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this announcement. The forward-looking statements made in this announcement relate only to the events or information as of the date on which the statements are made in this announcement. Except as required by law, we undertake no obligation to update or revise publicly any forward-looking statements, whether as a result of new information, future events or otherwise, after the date on which the statements are made or to reflect the occurrence of unanticipated events. You should read this announcement completely and with the understanding that our actual future results or performance may be materially different from what we expect. In this announcement, statements of, or references to, our intentions or those of any of our directors and/or our Company are made as of the date of this announcement. Any of these intentions may alter in light of future development. CStone Pharmaceuticals 基 石 藥 業 (Incorporated in the Cayman Islands with limited liability) (Stock Code: 2616) VOLUNTARY ANNOUNCEMENT CSTONE SUCCESSFULLY HOSTED THE FIRST U.S. R&D DAY IN NEW YORK CStone Pharmaceuticals (the “Company” or “CStone”) announces that it successfully hosted its 2020 U.S. R&D Day in New York City, the United States on January 21, 2020. -

Horizon Scanning Status Report June 2019
Statement of Funding and Purpose This report incorporates data collected during implementation of the Patient-Centered Outcomes Research Institute (PCORI) Health Care Horizon Scanning System, operated by ECRI Institute under contract to PCORI, Washington, DC (Contract No. MSA-HORIZSCAN-ECRI-ENG- 2018.7.12). The findings and conclusions in this document are those of the authors, who are responsible for its content. No statement in this report should be construed as an official position of PCORI. An intervention that potentially meets inclusion criteria might not appear in this report simply because the horizon scanning system has not yet detected it or it does not yet meet inclusion criteria outlined in the PCORI Health Care Horizon Scanning System: Horizon Scanning Protocol and Operations Manual. Inclusion or absence of interventions in the horizon scanning reports will change over time as new information is collected; therefore, inclusion or absence should not be construed as either an endorsement or rejection of specific interventions. A representative from PCORI served as a contracting officer’s technical representative and provided input during the implementation of the horizon scanning system. PCORI does not directly participate in horizon scanning or assessing leads or topics and did not provide opinions regarding potential impact of interventions. Financial Disclosure Statement None of the individuals compiling this information have any affiliations or financial involvement that conflicts with the material presented in this report. Public Domain Notice This document is in the public domain and may be used and reprinted without special permission. Citation of the source is appreciated. All statements, findings, and conclusions in this publication are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI) or its Board of Governors. -

ESMO 2019 Update
ESMO 2019 Update Axel Grothey Director, GI Oncology Research West Cancer Center Research Institute Encorafenib plus Cetuximab With or Without Binimetinib for BRAF V600E–Mutant Metastatic Colorectal Cancer: Expanded Results from a Randomized, 3-Arm, Phase 3 Study vs. the Choice of Either Irinotecan or FOLFIRI plus Cetuximab (BEACON CRC) Josep Tabernero, Axel Grothey, Eric Van Cutsem, Rona Yaeger, Harpreet Wasan, Takayuki Yoshino, Jayesh Desai, Fortunato Ciardiello, Fotios Loupakis, Yong Sang Hong, Neeltje Steeghs, Tormod Kyrre Guren, Hendrik-Tobias Arkenau, Pilar Garcia-Alfonso, Ashwin Gollerkeri, Michael Pickard, Kati Maharry, Janna Christy-Bittel, Lisa Anderson, and Scott Kopetz BEACON CRC: Binimetinib, Encorafenib, And Cetuximab COmbiNed to Treat BRAF-mutant ColoRectal Cancer 2 Study Design Patients with BRAFV600E mCRC with disease progression after 1 or 2 prior regimens; ECOG PS of 0 or 1; and no prior treatment with any RAF inhibitor, MEK inhibitor, or EGFR inhibitor Phase 3 Primary Endpoints: Safety Lead-in ENCORAFENIB + Triplet therapy BINIMETINIB + ENCORAFENIB + BINIMETINIB + CETUXIMAB Triplet vs Control n = 205 CETUXIMAB N = 30 OS R Doublet therapy (All randomized Pts) Encorafenib 300 mg PO daily 1:1:1 ENCORAFENIB + CETUXIMAB Binimetinib 45 mg PO bid n = 205 Cetuximab standard weekly ORR – dosing Blinded Central Control arm Review FOLFIRI + CETUXIMAB, or (1st 331 randomized Pts) irinotecan + CETUXIMAB n = 205 Randomization was stratified by ECOG PS (0 vs. 1), prior use of irinotecan (yes vs. no), and cetuximab source (US-licensed vs. EU-approved) Secondary Endpoints: Doublet vs Control and Triplet vs Doublet - OS & ORR, PFS, Safety QOL Assessments: EORTC QOL Questionnaire (QLQ C30), Functional Assessment of Cancer Therapy Colon Cancer, EuroQol 5D5L, and Patient Global Impression of Change). -

Cancer Treatment and Survivorship Facts & Figures 2019-2021
Cancer Treatment & Survivorship Facts & Figures 2019-2021 Estimated Numbers of Cancer Survivors by State as of January 1, 2019 WA 386,540 NH MT VT 84,080 ME ND 95,540 59,970 38,430 34,360 OR MN 213,620 300,980 MA ID 434,230 77,860 SD WI NY 42,810 313,370 1,105,550 WY MI 33,310 RI 570,760 67,900 IA PA NE CT 243,410 NV 185,720 771,120 108,500 OH 132,950 NJ 543,190 UT IL IN 581,350 115,840 651,810 296,940 DE 55,460 CA CO WV 225,470 1,888,480 KS 117,070 VA MO MD 275,420 151,950 408,060 300,200 KY 254,780 DC 18,750 NC TN 470,120 AZ OK 326,530 NM 207,260 AR 392,530 111,620 SC 143,320 280,890 GA AL MS 446,900 135,260 244,320 TX 1,140,170 LA 232,100 AK 36,550 FL 1,482,090 US 16,920,370 HI 84,960 States estimates do not sum to US total due to rounding. Source: Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute. Contents Introduction 1 Long-term Survivorship 24 Who Are Cancer Survivors? 1 Quality of Life 24 How Many People Have a History of Cancer? 2 Financial Hardship among Cancer Survivors 26 Cancer Treatment and Common Side Effects 4 Regaining and Improving Health through Healthy Behaviors 26 Cancer Survival and Access to Care 5 Concerns of Caregivers and Families 28 Selected Cancers 6 The Future of Cancer Survivorship in Breast (Female) 6 the United States 28 Cancers in Children and Adolescents 9 The American Cancer Society 30 Colon and Rectum 10 How the American Cancer Society Saves Lives 30 Leukemia and Lymphoma 12 Research 34 Lung and Bronchus 15 Advocacy 34 Melanoma of the Skin 16 Prostate 16 Sources of Statistics 36 Testis 17 References 37 Thyroid 19 Acknowledgments 45 Urinary Bladder 19 Uterine Corpus 21 Navigating the Cancer Experience: Treatment and Supportive Care 22 Making Decisions about Cancer Care 22 Cancer Rehabilitation 22 Psychosocial Care 23 Palliative Care 23 Transitioning to Long-term Survivorship 23 This publication attempts to summarize current scientific information about Global Headquarters: American Cancer Society Inc.