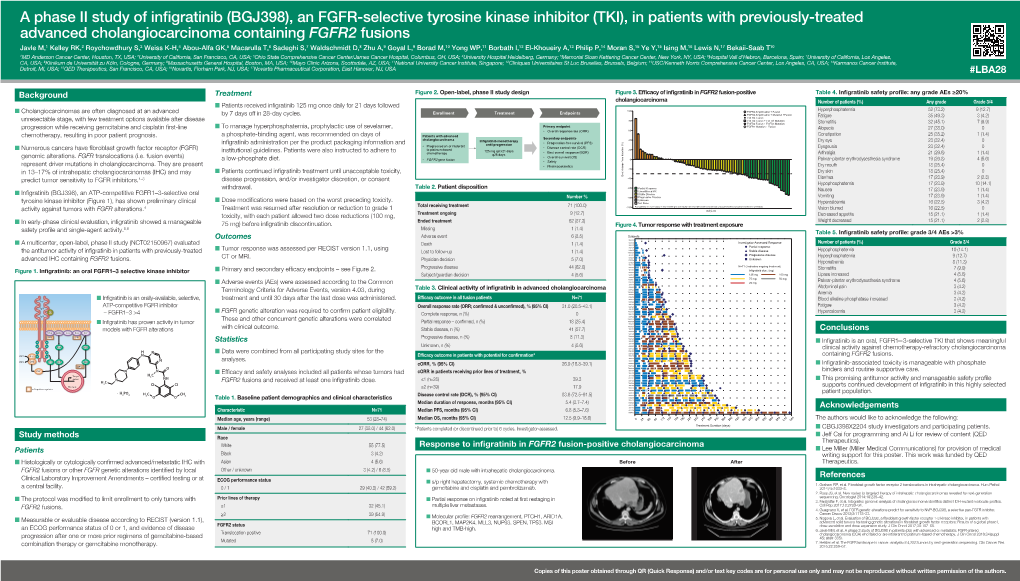
A Phase II Study of Infigratinib (BGJ398)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Targeted Therapies in Advanced Cholangiocarcinoma: a Focus on FGFR Inhibitors
medicina Review Targeted Therapies in Advanced Cholangiocarcinoma: A Focus on FGFR Inhibitors Alessandro Rizzo Department of Experimental, Diagnostic and Specialty Medicine, S. Orsola-Malpighi University Hospital, 40138 Bologna, Italy; [email protected] Abstract: Despite advanced diseases continuing to be associated with grim prognoses, the past decade has witnessed the advent of several novel treatment options for cholangiocarcinoma (CCA) patients. In fact, CCA has emerged as a heterogeneous group of malignancies harboring potentially druggable mutations in approximately 50% of cases, and thus, molecularly targeted therapies have been actively explored in this setting. Among these, fibroblast growth factor receptor (FGFR) inhibitors have reported important results, as witnessed by the FDA approval of pemigatinib in previously treated metastatic CCA patients harboring FGFR2 fusion or other rearrangements. Herein, we provide an overview of available evidence on FGFR inhibitors in CCA, especially focusing on the development, pitfalls and challenges of emerging treatments in this setting. Keywords: FGFR; cholangiocarcinoma; targeted therapies; intrahepatic cholangiocarcinoma; pemi- gatinib 1. Introduction Citation: Rizzo, A. Targeted Cholangiocarcinoma (CCA) encompasses a group of heterogeneous, rare and aggres- Therapies in Advanced sive malignancies, including intrahepatic cholangiocarcinoma (iCCA) and extrahepatic Cholangiocarcinoma: A Focus on cholangiocarcinoma (eCCA), with the latter further subclassified into perihilar (pCCA) FGFR Inhibitors. Medicina 2021, 57, and distal (dCCA) cholangiocarcinoma [1–3]. CCAs account for approximately 3% of 458. https://doi.org/10.3390/ all gastrointestinal cancers worldwide and 10–15% of all primary liver tumors [4–6]. As medicina57050458 suggested by several studies, these subgroups of hepatobiliary tumors not only develop from different anatomical locations, but vary widely in terms of epidemiology, biology, Academic Editor: Zygmunt Warzecha prognosis, and etiology [7–9]. -

New Horizons for Precision Medicine in Biliary Tract Cancers
Published OnlineFirst August 17, 2017; DOI: 10.1158/2159-8290.CD-17-0245 REVIEW New Horizons for Precision Medicine in Biliary Tract Cancers Juan W. Valle1,2, Angela Lamarca1, Lipika Goyal3, Jorge Barriuso1,4, and Andrew X. Zhu3 ABSTRACT Biliary tract cancers (BTC), including cholangiocarcinoma and gallbladder cancer, are poor-prognosis and low-incidence cancers, although the incidence of intrahe- patic cholangiocarcinoma is rising. A minority of patients present with resectable disease but relapse rates are high; benefit from adjuvant capecitabine chemotherapy has been demonstrated.Cisplatin/ gemcitabine combination chemotherapy has emerged as the reference first-line treatment regimen; there is no standard second-line therapy. Selected patients may be suitable for liver-directed therapy (e.g., radioembolization or external beam radiation), pending confirmation of benefit in randomized studies. Initial trials targeting the epithelial growth factor receptor and angiogenesis pathways have failed to deliver new treatments. Emerging data from next-generation sequencing analyses have iden- tified actionable mutations (e.g.,FGFR fusion rearrangements and IDH1 and IDH2 mutations), with several targeted drugs entering clinical development with encouraging results. The role of systemic therapies, including targeted therapies and immunotherapy for BTC, is rapidly evolving and is the sub- ject of this review. Significance: The authors address genetic drivers and molecular biology from a translational per- spective, in an intent to offer a clear view of the recent past, present, and future of BTC. The review describes a state-of-the-art update of the current status and future directions of research and therapy in advanced BTC. Cancer Discov; 7(9); 1–20. -

Current and Novel Therapeutic Opportunities for Systemic Therapy in Biliary Cancer
www.nature.com/bjc REVIEW ARTICLE Current and novel therapeutic opportunities for systemic therapy in biliary cancer José J. G. Marin1,2, Maria Giuseppina Prete3,4, Angela Lamarca5,6, Simona Tavolari7, Ana Landa-Magdalena8, Giovanni Brandi9, Oreste Segatto10, Arndt Vogel11, Rocío I. R. Macias1,2, Pedro M. Rodrigues8, Adelaida La Casta8, Joachim Mertens12, Cecilia M. P. Rodrigues13, Maite G. Fernandez-Barrena14, Ana Da Silva Ruivo15, Marco Marzioni16, Giulia Mentrasti16, Pilar Acedo17, Patricia Munoz-Garrido18, Vincenzo Cardinale19, Jesus M. Banales2,8,20, Juan W. Valle 5,6, John Bridgewater 21, Chiara Braconi 3, on behalf of the working group 6 of the COST-action 18122 (Euro-Cholangio-NET) as part of the European Network for the study of Cholangiocarcinoma (ENSCCA) Biliary tract cancers (BTCs) are a group of rare and aggressive malignancies that arise in the biliary tree within and outside the liver. Beyond surgical resection, which is beneficial for only a small proportion of patients, current strategies for treating patients with BTCs include chemotherapy, as a single agent or combination regimens, in the adjuvant and palliative setting. Increased characterisation of the molecular landscape of these tumours has facilitated the identification of molecular vulnerabilities, such as IDH mutations and FGFR fusions, that can be exploited for the treatment of BTC patients. Beyond targeted therapies, active research avenues explore the development of novel therapeutics that target the crosstalk between cancer and stroma, the cellular pathways involved in the regulation of cell death, the chemoresistance phenotype and the dysregulation of RNA. In this review, we discuss the therapeutic opportunities currently available in the management of BTC patients, and explore the strategies that can support the implementation of precision oncology in BTCs, including novel molecular targets, liquid biopsies and patient-derived predictive tools. -

Biliary Tract Cancers
Biliary Tract Cancers Miguel Navarro Salamanca BTCs are quite challenging to treat BTCs Background • Uncommon. • Increasing incidence and mortality globally. • Most patient are diagnosed with no resecable disease. • Associated with poor outcomes. • Need of new drugs. Khan SA, et al. J Hepatol. 2012;56:848-854. Biliary tract cancers are a diverse set of neoplasms arising from the biliary tract epithelium …. Why doesn´t one size fits all? Valle et al. Cancer Discovery.2017 Why doesn´t one size fits all? Valle et al. Cancer Discovery.2017 Why doesn´t one size fits all? Such differences are worth taking into account at time of treatment planning, research, and clinical trial design. Surgery • Biliary tract cancers usually present at an advanced stage, and only approximately 20% of tumors are considered resectable. • Surgery is the primary curative treatment option for early-stage biliary tract cancer. Adjuvant therapy • Need for effective adjuvant therapy. • Older randomised studies were not sufficiently statistically powered to define a standard of care. • Meta-analysis (of mostly retrospective data) has suggested improved overall survival with adjuvant treatment. Takada T, et al. Cancer 2002; 95: 1685–95. Neoptolemos JP,et al.JAMA 2012; 308: 147–56 Horgan AM, et al. J Clin Oncol 2012; 30: 1934–40. Adjuvant therapy Two recent randomised studies did NOT show a significant benefit of: • gemcitabine • gemcitabine plus oxaliplatin (GEMOX regimen) Adjuvant therapy BILCAP: Study Design Open-label, randomized, controlled phase III trial 753 patients -

Targeting the Src Pathway Enhances the Efficacy of Selective FGFR Inhibitors
bioRxiv preprint doi: https://doi.org/10.1101/2020.04.04.025544; this version posted April 5, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Targeting the Src pathway enhances the efficacy of selective FGFR inhibitors in cancers with FGFR3 alterations Nadia Carvalho Lima1, Eliza Atkinson1, Tom D Bunney2, Matilda Katan2, Paul H. Huang1 1) Division of Molecular Pathology, The Institute of Cancer Research, London, UK 2) Institute of Structural and Molecular Biology, Division of Biosciences, University College London, London, UK Correspondence to: Paul H Huang Division of Molecular Pathology Institute of Cancer Research 237 Fulham Road London SW3 6JB United Kingdom Email: [email protected] Keywords FGFR3, Src, urothelial cancer, bladder cancer, cell signalling, cancer therapeutics 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.04.04.025544; this version posted April 5, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Abstract Selective FGFR inhibitors such as infigratinib (BGJ398) and erdafitinib (JNJ-42756493) have been evaluated in clinical trials for cancers with FGFR3 molecular alterations, particularly in urothelial carcinoma patients. However, a substantial proportion of these patients (up to 50%) display intrinsic resistance to these drugs and receive minimal clinical benefit. -

1 Bridgebio Pharma's Affiliate QED Therapeutics and Helsinn Group
BridgeBio Pharma’s Affiliate QED Therapeutics and Helsinn Group Announce Strategic Collaboration to Co-Develop and Commercialize Infigratinib in Oncology ■ BridgeBio, through its Affiliate QED (“BridgeBio”), and Helsinn to co- commercialize infigratinib for oncology and all other indications other than skeletal dysplasia indications in the U.S. and equally share profits ■ Helsinn Group will have an exclusive license to co-develop, manufacture and commercialize infigratinib in such indications outside of the U.S., excluding China, Hong Kong and Macau ■ BridgeBio will be eligible to receive more than $2 billion USD in upfront, regulatory and commercial milestone payments ■ BridgeBio retains full rights to infigratinib for use in skeletal dysplasias, including for achondroplasia PALO ALTO, Calif. and LUGANO, Switzerland – March 31, 2021 – BridgeBio Pharma, Inc. (Nasdaq: BBIO), through its affiliate QED Therapeutics, Inc., and Helsinn Group today announced a global collaboration and licensing agreement (the “Agreement”) to further develop and commercialize QED Therapeutics’ FGFR1-3 inhibitor, infigratinib, in oncology and all other indications except for skeletal dysplasias (including achondroplasia). Completion of the Agreement is subject to regulatory review and customary closing conditions, which are expected to occur in the second quarter of 2021. Infigratinib is an orally administered, ATP-competitive, tyrosine kinase inhibitor that is designed to inhibit FGFR, and being investigated for treatment of individuals with FGFR-driven conditions, including cholangiocarcinoma (bile duct cancer), urothelial carcinoma (urinary tract and bladder cancer), and other FGFR-driven cancers. Under the terms of the Agreement, BridgeBio will retain all rights to infigratinib in skeletal dysplasia, including achondroplasia. Subject to U.S. Food and Drug Administration (“FDA”) approval, QED and Helsinn will co-commercialize infigratinib in oncology indications in the U.S. -

Sorafenib/MEK Inhibitor Combination Inhibits Tumor Growth and the Wnt/Β‑Catenin Pathway in Xenograft Models of Hepatocellular Carcinoma
INTERNATIONAL JOURNAL OF ONCOLOGY 54: 1123-1133, 2019 Sorafenib/MEK inhibitor combination inhibits tumor growth and the Wnt/β‑catenin pathway in xenograft models of hepatocellular carcinoma HUNG HUYNH1, RICHARD ONG1, KAH YONG GOH1, LIEK YEOW LEE1, FLORIAN PUEHLER2, ARNE SCHOLZ2, OLIVER POLITZ2, DOMINIK MUMBERG2 and KARL ZIEGELBAUER2 1Laboratory of Molecular Endocrinology, Division of Molecular and Cellular Research, National Cancer Centre, Singapore 169610, Republic of Singapore; 2R&D Pharmaceuticals, Bayer AG, D‑13353 Berlin, Germany Received September 14, 2018; Accepted January 8, 2019 DOI: 10.3892/ijo.2019.4693 Abstract. Mutations affecting the Wnt/β-catenin pathway and refametinib inhibits the growth of naïve and sorafenib have been identified in 26‑40% of hepatocellular carcinoma resistant HCC tumors in association with active suppression of (HCC) cases. Aberrant activation of this pathway leads to β‑catenin signaling regardless of β‑catenin mutational status. uncontrolled cell proliferation and survival. Thus, identifying Thus, the sorafenib/MEK inhibitor combination may represent Wnt/β‑catenin pathway inhibitors may benefit a subset of an alternative treatment for patients with HCC whose tumors patients with HCC. In the present study, the effects of sorafenib develop resistance to sorafenib therapy. and a MEK inhibitor on tumor growth and Wnt/β-catenin signaling in HCC models were evaluated. A β‑catenin mutant Introduction and β‑catenin wild‑type HCC models were treated once daily with i) 10 mg/kg sorafenib, ii) 15 mg/kg refametinib Hepatocellular carcinoma (HCC) is the second most common (or 25 mg/kg selumetinib), or iii) sorafenib/refametinib. cause of cancer mortality worldwide, and accounts for Western blotting was employed to determine changes in 500,000 to 1 million deaths annually worldwide (1). -

Facts and New Hopes on Selective FGFR Inhibitors in Solid Tumors Francesco Facchinetti1, Antoine Hollebecque2, Rastislav Bahleda2, Yohann Loriot3, Ken A
Published OnlineFirst October 4, 2019; DOI: 10.1158/1078-0432.CCR-19-2035 CLINICAL CANCER RESEARCH | REVIEW Facts and New Hopes on Selective FGFR Inhibitors in Solid Tumors Francesco Facchinetti1, Antoine Hollebecque2, Rastislav Bahleda2, Yohann Loriot3, Ken A. Olaussen1, Christophe Massard2, and Luc Friboulet1 ABSTRACT ◥ Precision oncology relies on the identification of molecular altera- molecularly guided treatments. Matching molecularly selected tions, responsible for tumor initiation and growth, which are suitable tumors with selective FGFR inhibitors has indeed led to promising targets of specific inhibitors. The development of FGFR inhibitors results in phase I and II trials, justifying their registration to be represents an edifying example of the rapid evolution in the field of expected in a near future, such as the recent accelerated approval of targeted oncology, with 10 different FGFR tyrosine kinase inhibitors erdafitinib granted by the FDA for urothelial cancer. Widening our actually under clinical investigation. In parallel, the discovery of knowledge of the activity, efficacy, and toxicities relative to the FGFR activating molecular alterations (mainly FGFR3 mutations selective FGFR tyrosine kinase inhibitors under clinical investi- and FGFR2 fusions) across many tumor types, especially urothelial gation, according to the exact FGFR molecular alteration, will be carcinomas and intrahepatic cholangiocarcinomas, widens the selec- crucial to determine the optimal therapeutic strategy for patients tion of patients that might benefit from selective FGFR inhibitors. suffering from FGFR-driven tumors. Similarly, identifying with The ongoing concomitant clinical evaluation of selective FGFR appropriate molecular diagnostic, every single tumor harboring inhibitors in molecularly selected solid tumors brings new hopes targetable FGFR alterations will be of utmost importance to attain for patients with metastatic cancer, for tumors so far excluded from the best outcomes for patients with FGFR-driven cancer. -

A Perspective from Clinical Trials
biomolecules Review Development of Possible Next Line of Systemic Therapies for Gemcitabine-Resistant Biliary Tract Cancers: A Perspective from Clinical Trials Nai-Jung Chiang 1,2, Li-Tzong Chen 1,2,3, Yan-Shen Shan 4,5, Chun-Nan Yeh 6,* and Ming-Huang Chen 7,8,* 1 National Institute of Cancer Research, National Health Research Institutes, Tainan 704, Taiwan; [email protected] (N.-J.C.); [email protected] (L.-T.C.) 2 Department of Oncology, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan 704, Taiwan 3 Department of Internal Medicine, Kaohsiung Medical University Hospital and Kaohsiung Medical University, Kaohsiung 807, Taiwan 4 Institute of Clinical Medicine, College of Medicine, National Cheng Kung University, Tainan 704, Taiwan; [email protected] 5 Department of Surgery, National Cheng Kung University Hospital, Tainan 704, Taiwan 6 Department of General Surgery and Liver Research Center, Chang Gung Memorial Hospital, Linkou Branch, Chang Gung University, Taoyuan 333, Taiwan 7 Center for Immuno-Oncology, Department of Oncology, Taipei Veterans General Hospital, Taipei 112, Taiwan 8 School of Medicine, National Yang Ming University, Taipei 112, Taiwan * Correspondence: [email protected] (C.-N.Y.); [email protected] (M.-H.C.); Tel.: +886-33281200 (C.-N.Y.); +886-28712121 (ext. 2508) (M.-H.C.); Fax: +886-33285818 (C.-N.Y.); +886-28732131 (M.-H.C.) Abstract: Biliary tract cancer (BTC) compromises a heterogenous group of tumors with poor prog- noses. Curative surgery remains the first choice for localized disease; however, most BTC pa- tients have had unresectable or metastatic disease. -
Tyrosine Kinase Inhibitors for Solid Tumors in the Past 20 Years (2001–2020) Liling Huang†, Shiyu Jiang† and Yuankai Shi*
Huang et al. J Hematol Oncol (2020) 13:143 https://doi.org/10.1186/s13045-020-00977-0 REVIEW Open Access Tyrosine kinase inhibitors for solid tumors in the past 20 years (2001–2020) Liling Huang†, Shiyu Jiang† and Yuankai Shi* Abstract Tyrosine kinases are implicated in tumorigenesis and progression, and have emerged as major targets for drug discovery. Tyrosine kinase inhibitors (TKIs) inhibit corresponding kinases from phosphorylating tyrosine residues of their substrates and then block the activation of downstream signaling pathways. Over the past 20 years, multiple robust and well-tolerated TKIs with single or multiple targets including EGFR, ALK, ROS1, HER2, NTRK, VEGFR, RET, MET, MEK, FGFR, PDGFR, and KIT have been developed, contributing to the realization of precision cancer medicine based on individual patient’s genetic alteration features. TKIs have dramatically improved patients’ survival and quality of life, and shifted treatment paradigm of various solid tumors. In this article, we summarized the developing history of TKIs for treatment of solid tumors, aiming to provide up-to-date evidence for clinical decision-making and insight for future studies. Keywords: Tyrosine kinase inhibitors, Solid tumors, Targeted therapy Introduction activation of tyrosine kinases due to mutations, translo- According to GLOBOCAN 2018, an estimated 18.1 cations, or amplifcations is implicated in tumorigenesis, million new cancer cases and 9.6 million cancer deaths progression, invasion, and metastasis of malignancies. occurred in 2018 worldwide [1]. Targeted agents are In addition, wild-type tyrosine kinases can also func- superior to traditional chemotherapeutic ones in selec- tion as critical nodes for pathway activation in cancer. -
Highlights from the First Annual Cholangiocarcinoma Summit
DECEMBER 2019 Highlights from the First Annual Cholangiocarcinoma Summit From the publishers of © 2019 The Lynx Group, LLC NOW ENROLLING NCT03656536 Cholangiocarcinoma Phase 3 Randomized, Open-Label, Phase 3 Study to Assess the Ef cacy and Safety of Pemigatinib (FGFR1/2/3 Inhibitor) Versus Gemcitabine Plus Cisplatin Chemotherapy in First-Line Treatment of Patients with Unresectable or Metastatic CCA with FGFR2 Rearrangement Primary endpoint: Patients with Pemigatinib PFS unresectable or metastatic cholangiocarcinoma with Secondary endpoints: FGFR2 rearrangement ORR, OS, DOR, DCR, (N = 432) Gemcitabine + Cisplatin Randomization safety, QOL Select inclusion criteria: Select exclusion criteria: • Age ≥18 years • Received prior anticancer systemic therapy for • Histologically or cytologically con rmed unresectable and/or metastatic disease (not including cholangiocarcinoma that is previously untreated and adjuvant/neo-adjuvant treatment completed at considered unresectable and/or metastatic least 6 months prior to enrollment, and treatment for locally advanced disease with clear evidence of • Radiographically measurable/evaluable disease by CT radiological progression) or MRI per RECIST v1.1 criteria • Child-Pugh B and C • ECOG PS 0 to 1 • Current evidence of clinically signi cant corneal • Documented FGFR2 rearrangement or retinal disorder con rmed by ophthalmologic examination • History of calcium and phosphate hemostasis disorder or systemic mineral imbalance with ectopic calci cation of soft tissue The ef cacy and safety of the investigational -

Precision Medicine Approaches to Lung Adenocarcinoma With
Oh et al. BMC Cancer (2017) 17:535 DOI 10.1186/s12885-017-3525-9 RESEARCH ARTICLE Open Access Precision medicine approaches to lung adenocarcinoma with concomitant MET and HER2 amplification Doo-Yi Oh1,3, Kyungsoo Jung3, Ji-Young Song1,3, Seokhwi Kim1, Sang Shin2,3, Yong-Jun Kwon2,3, Ensel Oh1,3, Woong-Yang Park3,4, Sang Yong Song1,2 and Yoon-La Choi1,3* Abstract Background: Patient-derived xenograft (PDX) models are important tools in precision medicine and for the development of targeted therapies to treat cancer patients. This study aimed to evaluate our precision medicine strategy that integrates genomic profiling and preclinical drug-screening platforms, in order to personalize cancer treatments using PDX models. Methods: We performed array-comparative genomic hybridization, microarray, and targeted next-generation sequencing analyses, in order to determine the oncogenic driver mutations. PDX cells were obtained from PDXs and subsequently screened in vitro with 17 targeted agents. Results: PDX tumors recapitulated the histopathologic and genetic features of the patient tumors. Among the samples from lung cancer patients that were molecularly-profiled, copy number analysis identified unique focal MET amplification in one sample, 033 T, without RTK/RAS/RAF oncogene mutations. Although HER2 amplification in 033 T was not detected in the cancer panel, the selection of HER2-amplified clones was found in PDXs and PDX cells. Additionally, MET and HER2 overexpression were found in patient tumors, PDXs, and PDX cells. Crizotinib or EGFR tyrosine kinase inhibitor treatments significantly inhibited cell growth and impaired tumor sphere formation in 033 T PDX cells. Conclusions: We established PDX cell models using surgical samples from lung cancer patients, and investigated their preclinical and clinical implications for personalized targeted therapy.