Estimation of the Percentage of US Patients with Cancer Who Benefit from Genome‐Driven Oncology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Oncofocus® Precision Oncology
Medical Laboratory Accredited to ISO15189:2012 Oncofocus® Precision Oncology ONCOFOCUS® TEST REPORT Oncologica UK Ltd Suite 15-16, The Science Village Chesterford Research Park Cambridge, CB10 1XL, UK Tel: +44(0)1223 785327 Email: [email protected] Lead Clinical Scientist: - Pre-Reg Clinical Scientist: - Date: 1 of 30 ONC19 - Surname - Requester - Forename - Contact details - DOB - Date requested - Gender - Histology # - Tumour % - Primary site Breast Tumour % - Tumour subtype - (macrodissected) Tissue Type - Comment: The DNA and RNA extracted from this sample were of optimal quality. The Oncofocus assay on which the sample was run met all assay specific quality metrics. Oncofocus currently targets 505 genes covering oncogenes, fusion genes, genes susceptible to copy number variation and tumour suppressors. Actionable genetic variants detected by Oncofocus are currently linked to 687 anti-cancer targeted therapies/therapy combinations. The following actionable variants were detected: Within the 'Current Clinical Trials Information' section of this report, starting on page 8, the NCT numbers are hyperlinks to the clinicaltrials.gov webpages which should be accessed to gain further trial specific information Sample Cancer Type: Breast Cancer Clinically Significant Biomarkers Indicated Contraindicated Relevant Therapies Relevant Therapies Genomic Alteration Alt allele freq (In this cancer type) (In other cancer type) Clinical Trials ERBB2 p.(G727A) c.2180G>C 39% Clinical trials and/or off-label ado-trastuzumab emtansine 19 BRAF p.(V600E) c.1799T>A 5% Clinical trials and/or off-label dabrafenib 13 vemurafenib PIK3CA p.(G1049R) c.3145G>C 58% Clinical trials and/or off-label Clinical trials and/or off-label 15 Sources included in relevant therapies: EMA1, FDA2, ESMO, NCCN Hotspot variants with >10% alternate allele reads are classified as ‘detected’ with an assay sensitivity and positive predictive value(PPV) of 99%. -

Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer
diagnostics Review Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer Shunsuke Kato Department of Clinical Oncology, Juntendo University Graduate School of Medicine, 2-1-1, Hongo, Bunkyo-ku, Tokyo 113-8421, Japan; [email protected]; Tel.: +81-3-5802-1543 Abstract: The prognosis of patients with solid tumours has remarkably improved with the develop- ment of molecular-targeted drugs and immune checkpoint inhibitors. However, the improvements in the prognosis of pancreatic cancer and biliary tract cancer is delayed compared to other carcinomas, and the 5-year survival rates of distal-stage disease are approximately 10 and 20%, respectively. How- ever, a comprehensive analysis of tumour cells using The Cancer Genome Atlas (TCGA) project has led to the identification of various driver mutations. Evidently, few mutations exist across organs, and basket trials targeting driver mutations regardless of the primary organ are being actively conducted. Such basket trials not only focus on the gate keeper-type oncogene mutations, such as HER2 and BRAF, but also focus on the caretaker-type tumour suppressor genes, such as BRCA1/2, mismatch repair-related genes, which cause hereditary cancer syndrome. As oncogene panel testing is a vital approach in routine practice, clinicians should devise a strategy for improved understanding of the cancer genome. Here, the gene mutation profiles of pancreatic cancer and biliary tract cancer have been outlined and the current status of tumour-agnostic therapy in these cancers has been reported. Keywords: pancreatic cancer; biliary tract cancer; targeted therapy; solid tumours; driver mutations; agonist therapy Citation: Kato, S. Tumour-Agnostic Therapy for Pancreatic Cancer and 1. -

Product Monograph Including Patient Medication Information
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION Pr ® COTELLIC cobimetinib tablets 20 mg cobimetinib (as cobimetinib fumarate) Protein Kinase Inhibitor Date of Revision: Hoffmann-La Roche Limited January 5, 2018 7070 Mississauga Road Mississauga, Ontario, Canada L5N 5M8 www.rochecanada.com Submission Control No: 209926 COTELLIC®, ZELBORAF® are registered trade-marks of F. Hoffmann-La Roche AG, used under license ©Copyright 2016-2017, Hoffmann-La Roche Limited Page 1 of 38 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .........................................................3 SUMMARY PRODUCT INFORMATION ........................................................................3 INDICATIONS AND CLINICAL USE ..............................................................................3 CONTRAINDICATIONS ...................................................................................................3 WARNINGS AND PRECAUTIONS ..................................................................................4 ADVERSE REACTIONS ..................................................................................................11 DRUG INTERACTIONS ..................................................................................................15 DOSAGE AND ADMINISTRATION ..............................................................................17 OVERDOSAGE ................................................................................................................20 ACTION AND CLINICAL PHARMACOLOGY ............................................................20 -

Quantification of Cobimetinib, Cabozantinib, Dabrafenib, Niraparib
University of Groningen Quantification of cobimetinib, cabozantinib, dabrafenib, niraparib, olaparib, vemurafenib, regorafenib and its metabolite regorafenib M2 in human plasma by UPLC-MS/MS Krens, Stefanie D; van der Meulen, Eric; Jansman, Frank G A; Burger, David M; van Erp, Nielka P Published in: Biomedical chromatography DOI: 10.1002/bmc.4758 IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2020 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Krens, S. D., van der Meulen, E., Jansman, F. G. A., Burger, D. M., & van Erp, N. P. (2020). Quantification of cobimetinib, cabozantinib, dabrafenib, niraparib, olaparib, vemurafenib, regorafenib and its metabolite regorafenib M2 in human plasma by UPLC-MS/MS. Biomedical chromatography, 34(3), [4758]. https://doi.org/10.1002/bmc.4758 Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). The publication may also be distributed here under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license. More information can be found on the University of Groningen website: https://www.rug.nl/library/open-access/self-archiving-pure/taverne- amendment. Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. -
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
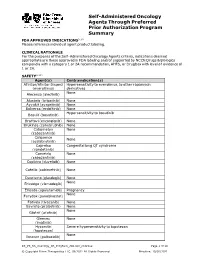
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

Pharmacy Pre-Authorization Criteria
PHARMACY PRE-AUTHORIZATION CRITERIA DRUG (S) Oncology Medications: Sprycel (dasatinib) Afinitor (everolimus) Stivarga (regorafenib) Caprelsa (vandetanib) Sutent (sunitinib) Gilotrif (afatinib dimaleate) Tarceva (erlotinob) Gleevec (imatinib mesylate) Temodar (temozolomide) Ibrance (palbociclib) Tepadina (thiotepa) Idhifa (enasidenib) Thalomid (thalidomide) Iressa (gefitinib) Vantas (histrelin acetate) Kisqali (ribociclib) Venclexta (venetoclax) Lenvima (lenvatinib) Verzenio (abemaciclib) Nerlynx (neratinib) Vidaza (azacitidine) Nexavar (sorafenib) Votrient (pazopanib) Ninlaro (ixazomib) Xalkori (crizotinib) Odomzo (sonidegib) Xeloda (capecitabine) Zydelig (idelalisib) Zykadia (certinib) Zytiga (abiraterone acetate) PHARMACY PRE-AUTHORIZATION CRITERIA POLICY # 21107 CRITERIA The above medications are covered when the following criteria are met: 1. Ordered by an oncologist or hematologist AND 2. All FDA Approved Indications OR 3. Chemo agent is listed in an accepted Compendia for treatment of cancer type, OR - National Comprehensive Cancer Network (NCCN) Drugs and Biologics Compendium, level of evidence 1, 2A, or 2B - Thomson Micromedex DrugDex - Chemo agent is recommended for cancer type in formal clinical studies published in at least 2 peer reviewed professional medical journals, published in the United States or Great Britain Coverage Duration: Initial: 3 months Continuation: 6 months. Afinitor, Gilotrif, Gleevec, Ibrance, Idhifa, Iressa, Kisqali, Lenvima, Nexavar, Ninlaro, Odomzo, Sprycel, Stivarga, Sutent, Tarceva, Temodar, Thalomid, -

211192Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 211192Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 211192 PDUFA Goal Date August 21, 2018 OSE RCM # 2017-2612; 2017-2614 Reviewer Name(s) Till Olickal, Ph.D., Pharm.D. Team Leader Elizabeth Everhart, MSN, RN, ACNP Division Director Cynthia LaCivita, Pharm.D. Review Completion Date June 6, 2018 Subject Review to determine if a REMS is necessary Established Name Ivosidenib Trade Name Tibsovo Name of Applicant Agios Pharmaceuticals, Inc. Therapeutic Class Isocitrate dehydrogenase-1 inhibitor Formulation(s) 250 mg tablet Dosing Regimen 500 mg orally once daily until disease progression or unacceptable toxicity. 1 Reference ID: 4273770 Table of Contents EXECUTIVE SUMMARY ......................................................................................................................................................... 3 1 Introduction ..................................................................................................................................................................... 3 2 Background ...................................................................................................................................................................... 3 2.1 Product Information .......................................................................................................................................... -

New Oncology Reimbursements in Belgium
33 New oncology reimbursements in Belgium P. Specenier, MD, PhD OVERVIEW OF BELGIAN REIMBURSEMENT NEWS (BELG J MED ONCOL 2018;12(1):33-34) TEMOZOLOMIDE® (TEMODAR/TEMODAL) was 7.4 months (95% confidence interval [CI] 5.6-9.1) with Some companies have transferred temozolomide from chap- cabozantinib versus 3.8 months (95% CI 3.7-5.4) with ever- ter IV to chapter I. These can now be prescribed without re- olimus with a hazard ratio (HR) of 0.58 (95% CI 0.45-0.74; strictions. In the near future, other temozolomide brands are p<0.0001). Similar data were observed in the intent-to-treat also expected to be transferred. population. A planned interim analysis of overall survival (OS) was conducted at the time of the PFS analysis and did LOMUSTINE (CCNU) not reach the interim boundary for statistical significance The reimbursement criteria for lomustine have been modi- (HR=0.68 [0.51, 0.90], p=0.006). However, in a subsequent fied and are entirely concordant with the recently modified unplanned interim analysis of OS, a statistically significant criteria for procarbazine, except for the indication Hodgkin’s improvement was demonstrated (median 21.4 months ver- disease, which only applies for procarbazine. sus 16.5 months; HR=0.66; 95% CI 0.53-0.83; p=0.0003). The overall response rate (ORR) was 17% (95% CI 13-22) for CABOMETYX® (CABOZANTINIB) cabozantinib and 3% (95% CI 2-6) for everolimus (p<0.0001). Cabometyx® (cabozantinib) can be reimbursed for patients with advanced renal cell carcinoma (RCC) after at least one COTELLIC® (COBIMETINIB) prior anti-VEGF directed agent. -

Horizon Scanning Status Report June 2019
Statement of Funding and Purpose This report incorporates data collected during implementation of the Patient-Centered Outcomes Research Institute (PCORI) Health Care Horizon Scanning System, operated by ECRI Institute under contract to PCORI, Washington, DC (Contract No. MSA-HORIZSCAN-ECRI-ENG- 2018.7.12). The findings and conclusions in this document are those of the authors, who are responsible for its content. No statement in this report should be construed as an official position of PCORI. An intervention that potentially meets inclusion criteria might not appear in this report simply because the horizon scanning system has not yet detected it or it does not yet meet inclusion criteria outlined in the PCORI Health Care Horizon Scanning System: Horizon Scanning Protocol and Operations Manual. Inclusion or absence of interventions in the horizon scanning reports will change over time as new information is collected; therefore, inclusion or absence should not be construed as either an endorsement or rejection of specific interventions. A representative from PCORI served as a contracting officer’s technical representative and provided input during the implementation of the horizon scanning system. PCORI does not directly participate in horizon scanning or assessing leads or topics and did not provide opinions regarding potential impact of interventions. Financial Disclosure Statement None of the individuals compiling this information have any affiliations or financial involvement that conflicts with the material presented in this report. Public Domain Notice This document is in the public domain and may be used and reprinted without special permission. Citation of the source is appreciated. All statements, findings, and conclusions in this publication are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI) or its Board of Governors. -

Combined BRAF and MEK Inhibition with Vemurafenib and Cobimetinib for Patients with Advanced Melanoma
Review Melanoma Combined BRAF and MEK Inhibition with Vemurafenib and Cobimetinib for Patients with Advanced Melanoma Antonio M Grimaldi, Ester Simeone, Lucia Festino, Vito Vanella and Paolo A Ascierto Melanoma, Cancer Immunotherapy and Innovative Therapy Unit, Istituto Nazionale Tumori Fondazione “G. Pascale”, Napoli, Italy cquired resistance is the most common cause of BRAF inhibitor monotherapy treatment failure, with the majority of patients experiencing disease progression with a median progression-free survival of 6-8 months. As such, there has been considerable A focus on combined therapy with dual BRAF and MEK inhibition as a means to improve outcomes compared with monotherapy. In the COMBI-d and COMBI-v trials, combined dabrafenib and trametinib was associated with significant improvements in outcomes compared with dabrafenib or vemurafenib monotherapy, in patients with BRAF-mutant metastatic melanoma. The combination of vemurafenib and cobimetinib has also been investigated. In the phase III CoBRIM study in patients with unresectable stage III-IV BRAF-mutant melanoma, treatment with vemurafenib and cobimetinib resulted in significantly longer progression-free survival and overall survival (OS) compared with vemurafenib alone. One-year OS was 74.5% in the vemurafenib and cobimetinib group and 63.8% in the vemurafenib group, while 2-year OS rates were 48.3% and 38.0%, respectively. The combination was also well tolerated, with a lower incidence of cutaneous squamous-cell carcinoma and keratoacanthoma compared with monotherapy. Dual inhibition of both MEK and BRAF appears to provide a more potent and durable anti-tumour effect than BRAF monotherapy, helping to prevent acquired resistance as well as decreasing adverse events related to BRAF inhibitor-induced activation of the MAPK-pathway. -

Preferential Response of Basal-Like Head and Neck Squamous Cell Carcinoma Cell Lines to EGFR-Targeted Therapy Depending on EREG-Driven Oncogenic Addiction
Article Preferential Response of Basal-Like Head and Neck Squamous Cell Carcinoma Cell Lines to EGFR-Targeted Therapy Depending on EREG-Driven Oncogenic Addiction Sylvie Job 1, Aurélien de Reyniès 1, Betty Heller 2, Amélie Weiss 2, Eric Guérin 3,4, Christine Macabre 4,5, Sonia Ledrappier 4,5, Cyril Bour 4,5, Christine Wasylyk 2, Nelly Etienne-Selloum 5,6, Laurent Brino 2, Christian Gaiddon 4, Bohdan Wasylyk 2,† and Alain C. Jung 4,5,†,* 1 Programme Cartes d’Identité des Tumeurs (CIT), Ligue Nationale Contre le Cancer, 75013 Paris, France; [email protected] (S.J.); [email protected] (A.d.R.) 2 Institut de Génétique et de Biologie Moléculaire et Cellulaire IGBMC, UMR 7104 CNRS-UdS, U.1258 INSERM, 1 rue Laurent Fries, BP 10142, 67404 Illkirch cedex, France.; [email protected] (B.H.); [email protected] (A.W.); [email protected] (C.W.); [email protected] (L.B.); [email protected] (B.W.) 3 Laboratoire de Biochimie et Biologie Moléculaire, Hôpitaux Universitaires de Strasbourg, 67098 Strasbourg, France; [email protected] 4 Université de Strasbourg, Inserm, UMR_S1113, 67200 Strasbourg, France; [email protected] (C.M.); [email protected] (S.L.); [email protected] (C.B.); [email protected] (C.G.) 5 Centre de Lutte Contre le Cancer Paul Strauss, 67000 Strasbourg, France; [email protected] 6 UMR 7021 CNRS/Unistra, Laboratoire de Bioimagerie et Pathologies (LBP), Faculté de Pharmacie, 67401 Illkirch, France * Correspondence: [email protected]; Tel.: +33-0388275367 † These authors contributed equally to this work. -

209606Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209606Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA Multidisciplinary Review and Evaluation Application Number(s) NDA 209606 Application Type Original 505(b)(1) Priority or Standard Priority Submit Date(s) December 30, 2016 Received Date(s) December 30, 2016 PDUFA Goal Date August 30, 2017 Division/Office DHP/OHOP Review Completion Date July 28, 2017 Applicant Celgene Corporation Established Name Enasidenib (Proposed) Trade Name IDHIFA® Pharmacologic Class Isocitrate dehydrogenase 2 inhibitor Formulation(s) Tablets, 50mg and 100mg Dosing Regimen 100 mg once daily Applicant Proposed IDHIFA is indicated for the treatment of patients with relapsed or Indication(s)/Population(s) refractory acute myeloid leukemia with an IDH2 mutation Recommendation on Regular approval Regulatory Action Recommended IDHIFA is an isocitrate dehydrogenase-2 inhibitor indicated for the Indication(s)/Population(s) treatment of adult patients with relapsed or refractory acute myeloid leukemia with an isocitrate dehydrogenase-2 mutation as detected by an FDA-approved test. Reference ID: 4131433 Multidisciplinary Review and Evaluation NDA 209606 IDHIFA® (enasidenib) Table of Contents Table of Contents ........................................................................................................................... 2 Table of Tables ..............................................................................................................................