First-Line Treatment Options for Patients with Stage IV Non-Small Cell Lung Cancer with Driver Alterations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cstone's Partner Blueprint Medicines Presented Updated Part 1 Data from PIONEER Trial of Avapritinib
Hong Kong Exchanges and Clearing Limited and The Stock Exchange of Hong Kong Limited take no responsibility for the contents of this announcement, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this announcement. The forward-looking statements made in this announcement relate only to the events or information as of the date on which the statements are made in this announcement. Except as required by law, we undertake no obligation to update or revise publicly any forward-looking statements, whether as a result of new information, future events or otherwise, after the date on which the statements are made or to reflect the occurrence of unanticipated events. You should read this announcement completely and with the understanding that our actual future results or performance may be materially different from what we expect. In this announcement, statements of, or references to, our intentions or those of any of our directors and/or our Company are made as of the date of this announcement. Any of these intentions may alter in light of future development. CStone Pharmaceuticals 基 石 藥 業 (Incorporated in the Cayman Islands with limited liability) (Stock Code: 2616) VOLUNTARY ANNOUNCEMENT CSTONE’S PARTNER BLUEPRINT MEDICINES PRESENTED UPDATED PART 1 DATA FROM PIONEER TRIAL OF AVAPRITINIB SHOWING ROBUST REDUCTIONS IN CUTANEOUS DISEASE SYMPTOMS IN PATIENTS WITH INDOLENT SYSTEMIC MASTOCYTOSIS The partner of CStone Pharmaceuticals (the “Company” or “CStone”), Blueprint Medicines Corporation (NASDAQ: BPMC) (“Blueprint Medicines”), announced on June 6 updated clinical data from part 1 of the PIONEER trial showing robust and consistent clinical activity for avapritinib across multiple qualitative and quantitative measures of cutaneous disease in patients with indolent systemic mastocytosis (“ISM”). -

Mekinist, INN-Trametinib
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 for how to report adverse reactions. 1. NAME OF THE MEDICINAL PRODUCT Mekinist 0.5 mg film-coated tablets Mekinist 2 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Mekinist 0.5 mg film-coated tablets Each film-coated tablet contains trametinib dimethyl sulfoxide equivalent to 0.5 mg of trametinib. Mekinist 2 mg film-coated tablets Each film-coated tablet contains trametinib dimethyl sulfoxide equivalent to 2 mg of trametinib. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet Mekinist 0.5 mg film-coated tablets Yellow, modified oval, biconvex, film-coated tablets, approximately 4.8 x 8.9 mm, with “GS” debossed on one face and “TFC” on the opposing face. Mekinist 2 mg film-coated tablets Pink, round, biconvex, film-coated tablets, approximately 7.5 mm, with “GS” debossed on one face and “HMJ” on the opposing face. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Trametinib as monotherapy or in combination with dabrafenib is indicated for the treatment of adult patients with unresectable or metastatic melanoma with a BRAF V600 mutation (see sections 4.4 and 5.1). Trametinib monotherapy has not demonstrated clinical activity in patients who have progressed on a prior BRAF inhibitor therapy (see section 5.1). 4.2 Posology and method of administration Treatment with trametinib should only be initiated and supervised by a physician experienced in the administration of anti-cancer medicinal products. -

Clinical Response of the Novel Activating ALK-I1171T
http://www.diva-portal.org This is the published version of a paper published in Cold Spring Harbor Molecular Case Studies. Citation for the original published paper (version of record): Guan, J., Fransson, S., Siaw, J T., Treis, D., Van den Eynden, J. et al. (2018) Clinical response of the novel activating ALK-I1171T mutation in neuroblastoma o the ALK inhibitor ceritinib Cold Spring Harbor Molecular Case Studies, 4(4): a002550 https://doi.org/10.1101/mcs.a002550 Access to the published version may require subscription. N.B. When citing this work, cite the original published paper. Permanent link to this version: http://urn.kb.se/resolve?urn=urn:nbn:se:umu:diva-154087 Downloaded from molecularcasestudies.cshlp.org on December 12, 2018 - Published by Cold Spring Harbor Laboratory Press COLD SPRING HARBOR Molecular Case Studies | RESEARCH ARTICLE Clinical response of the novel activating ALK-I1171T mutation in neuroblastoma to the ALK inhibitor ceritinib Jikui Guan,1,2,12 Susanne Fransson,3,12 Joachim Tetteh Siaw,1,12 Diana Treis,4,12 Jimmy Van den Eynden,1 Damini Chand,1 Ganesh Umapathy,1 Kristina Ruuth,5 Petter Svenberg,4 Sandra Wessman,6,7 Alia Shamikh,6,7 Hans Jacobsson,8 Lena Gordon,9 Jakob Stenman,10 Pär-Johan Svensson,10 Magnus Hansson,11 Erik Larsson,1 Tommy Martinsson,3 Ruth H. Palmer,1 Per Kogner,6,7 and Bengt Hallberg1 1Department of Medical Biochemistry and Cell Biology, Institute of Biomedicine, The Sahlgrenska Academy, University of Gothenburg, Gothenburg 40530, Sweden; 2Children’s Hospital Affiliated to Zhengzhou University, -

Alectinib Provides a New Option for ALK-Positive NSCLC Patients After Progression on Crizotinib See Commentary on Page 239
Community Translations Edited by Jame Abraham, MD, FACP Alectinib provides a new option for ALK-positive NSCLC patients after progression on crizotinib See Commentary on page 239 n December 2015, alectinib became the third ALK inhibitor approved by the United States Food and What’s new, what’s important IDrug Administration for the treatment of non-small- The US Food and Drug Administration approved alectinib to cell lung cancer (NSCLC) that displays rearrangements of treat patients with metastatic ALK-positive non-small-cell lung the anaplastic lymphoma kinase (ALK) gene. Alectinib is cancer whose disease had progressed or who could not toler- a second-generation small molecule inhibitor of the ALK ate treatment with crizotinib. In clinical trials, alectinib showed a protein that joins ceritinib in providing a useful treatment partial response of 38%-44% and an average progression-free option for patients who have progressed on crizotinib, as survival of 11.2 months. In all, 61% of patients experienced a a result of its ability to target crizotinib-resistant mutant complete or partial reduction in their brain metastatic lesions, forms of the ALK protein. Alectinib also displays enhanced with a progression-free survival of of 9.1 months. The recom- penetrance of the blood-brain barrier, which improves ef- mended dose is 600 mg orally twice daily. cacy against central nervous system (CNS) metastases. The most common side effects are fatigue, constipation, swell- Te FDA awarded alectinib accelerated approval on the ing (edema), and muscle pain (myalgia). Treatment with alec- basis of 2 phase 2, single-arm clinical trials in patients tinib may cause sunburn when patients are exposed to sunlight, with ALK-positive NSCLC who had progressed on and pregnant women should be notifed of the possible risk to crizotinib therapy, a group of patients who have few avail- the fetus, and to use contraception throughout treatment and for able treatment options. -

Pharmaceutics of Oral Anticancer Agents and Stimulants
Pharmaceutics of oral anticancer agents and stimulants Maikel Herbrink The research in this thesis was performed at the Departments of Pharmacy & Pharma- cology and Medical Oncology & Clinical Pharmacology of the Netherlands Cancer Insti- tute – Antoni van Leeuwenhoek hospital, Amsterdam, the Netherlands. Printing of this thesis was financially supported by: Netherlands Cancer Institute Chipsoft BV Pfizer BV ISBN: 978-90-393-6997-5 Design, lay-out and print Gildeprint, Enschede © Maikel Herbrink, 2018 Pharmaceutics of oral anticancer agents and stimulants Farmaceutisch onderzoek naar oraal toegediende antikankermiddelen en stimulantia (met een samenvatting in het Nederlands) Proefschrift ter verkrijging van de graad van doctor aan de Universiteit Utrecht op gezag van de rector magnificus, prof. dr. H.R.B.M. Kummeling, ingevolge het besluit van het college voor promoties in het openbaar te verdedigen op woensdag 27 juni 2018 des middags te 4.15 uur door Maikel Herbrink geboren op 2 februari 1990 te Groningen Promotoren: Prof. dr. J.H. Beijnen Prof. dr. J.H.M. Schellens Copromotor: Dr. B. Nuijen Contents Preface 9 Chapter 1: Introduction 15 1.1 Variability in bioavailability of small molecular tyrosine 17 kinase inhibitors Cancer Treat Rev. 2015 May;41(5):412-422 1.2 Inherent formulation issues of kinase inhibitors 51 J Control Release. 2016 Oct;239:118-127 1.3 High-tech drugs in creaky formulations 81 Pharm Res. 2017 Sep;34(9):1751-1753 Chapter 2: Pharmaceutical analysis of oral anticancer drug substances 89 2.1. Thermal study of pazopanib hydrochloride 91 J Therm Anal Calorim. 2017 Dec;130(3):1491-1499 2.2. -

ZYKADIA (Ceritinib) RATIONALE for INCLUSION in PA PROGRAM
ZYKADIA (ceritinib) RATIONALE FOR INCLUSION IN PA PROGRAM Background Zykadia is used in patients with a certain type of late-stage (metastatic) non-small cell lung cancer (NSCLC), which is caused by a defect in a gene called anaplastic lymphoma kinase (ALK). Zykadia is a tyrosine kinase inhibitor that blocks proteins that promote the development of cancerous cells. It is intended for patients with metastatic ALK-positive NSCLC (1). Regulatory Status FDA- approved indication: Zykadia is a kinase inhibitor indicated for the treatment of patients with anaplastic lymphoma kinase (ALK)-positive metastatic non-small cell lung cancer (NSCLC) as detected by an FDA-approved test (1). Off-Label Uses: (2-3) 1. Inflammatory Myofibroblastic Tumor (IMT) with ALK translocation Zykadia can cause hepatotoxicity therefore liver function tests including AST, ALT and total bilirubin should be monitored at least monthly. Zykadia can cause interstitial lung disease (ILD) or pneumonitis. Zykadia should be permanently discontinued in patients diagnosed with treatment- related ILD/pneumonitis. Zykadia can cause QTc interval prolongation, which requires monitoring of electrocardiograms and electrolytes in patients with congestive heart failure (1). Zykadia is pregnancy category D and may cause fetal harm when administered to a pregnant woman (1). Safety and effectiveness of Zykadia in pediatric patients have not been established (1). Summary Zykadia is an anaplastic lymphoma kinase (ALK) tyrosine kinase inhibitor that blocks proteins that promote the development of cancerous cells. It is intended for patients with metastatic ALK-positive NSCLC. Safety and effectiveness of Zykadia in patients under 18 years of age have not been established (1). Zykadia FEP Clinical Rationale ZYKADIA (ceritinib) Prior approval is required to ensure the safe, clinically appropriate and cost effective use of Zykadia while maintaining optimal therapeutic outcomes. -

Successful Chemotherapy Is Possible for Seemingly Inoperable Anaplastic Thyroid Cancer
® Clinical Thyroidology for the Public VOLUME 12 | ISSUE 12 | DECEMBER 2019 THYROID CANCER Successful chemotherapy is possible for seemingly inoperable anaplastic thyroid cancer BACKGROUND form of standard chemotherapy and 2 received another While the vast majority of thyroid cancers are slow tyrosine kinase inhibitor called pembrolizumab. Of the 6 growing and have an excellent prognosis, anaplastic patients that had surgery after this treatment, 4 patients thyroid cancer, which makes up <1% of all thyroid cancer, had the entire primary cancer removed and the other 2 is one of the most aggressive of all cancers, with a survival patients only had microscopic pieces of cancer left after averaging ~6 months after diagnosis. Surgery, radiation the surgery. After the surgery, 5 of 6 patients received and single drug chemotherapy is all ineffective in most standard chemotherapy and radiation to the surgical area. cases. The aim of this study is to study if combination Of the 6 patients, 4 patients had no evidence of cancer at chemotherapy will make previously inoperable anaplastic the last check, some over 2 years after surgery. The 2 other thyroid cancers safe to remove with surgery. patients did pass away from anaplastic cancer; however, there was no re-growth of cancer in the area where surgery THE FULL ARTICLE TITLE occurred. Wang JR et al 2019 Complete surgical resection following neoadjuvant dabrafenib plus trametinib in BRAFV600E- WHAT ARE THE IMPLICATIONS mutated anaplastic thyroid carcinoma. Thyroid 29:1036– OF THIS STUDY? 1043. PMID: 31319771. In selected patients with anaplastic thyroid cancer with the BRAF V600E mutation, treatment with dabrafenib SUMMARY OF THE STUDY and trametinib may increase the chance of having a In this study from the MD Anderson Cancer Center successful surgery of the primary tumor. -

07052020 MR ASCO20 Curtain Raiser
Media Release New data at the ASCO20 Virtual Scientific Program reflects Roche’s commitment to accelerating progress in cancer care First clinical data from tiragolumab, Roche’s novel anti-TIGIT cancer immunotherapy, in combination with Tecentriq® (atezolizumab) in patients with PD-L1-positive metastatic non- small cell lung cancer (NSCLC) Updated overall survival data for Alecensa® (alectinib), in people living with anaplastic lymphoma kinase (ALK)-positive metastatic NSCLC Key highlights to be shared on Roche’s ASCO virtual newsroom, 29 May 2020, 08:00 CEST Basel, 7 May 2020 - Roche (SIX: RO, ROG; OTCQX: RHHBY) today announced that new data from clinical trials of 19 approved and investigational medicines across 21 cancer types, will be presented at the ASCO20 Virtual Scientific Program organised by the American Society of Clinical Oncology (ASCO), which will be held 29-31 May, 2020. A total of 120 abstracts that include a Roche medicine will be presented at this year's meeting. "At ASCO, we will present new data from many investigational and approved medicines across our broad oncology portfolio," said Levi Garraway, M.D., Ph.D., Roche's Chief Medical Officer and Head of Global Product Development. “These efforts exemplify our long-standing commitment to improving outcomes for people with cancer, even during these unprecedented times. By integrating our medicines and diagnostics together with advanced insights and novel platforms, Roche is uniquely positioned to deliver the healthcare solutions of the future." Together with its partners, Roche is pioneering a comprehensive approach to cancer care, combining new diagnostics and treatments with innovative, integrated data and access solutions for approved medicines that will both personalise and transform the outcomes of people affected by this deadly disease. -

Center for Drug Evaluation and Research
CENTER FOR DRUG EVALUATION AND RESEARCH Approval Package for: APPLICATION NUMBER: 125554Origs051 Trade Name: OPDIVO Generic or Proper nivolumab Name: Sponsor: Bristol-Myers Squibb Company Approval Date: March 05, 2018 Indication: Opdivo is a programmed death receptor-1 (PD-1) blocking antibody indicated for the treatment of: • patients with BRAF V600 wild-type unresectable or metastatic melanoma, as a single agent. (1.1) • patients with BRAF V600 mutation-positive unresectable or metastatic melanoma, as a single agent.a (1.1) • patients with unresectable or metastatic melanoma, in combination with ipilimumab.a (1.1) • patients with melanoma with lymph node involvement or metastatic disease who have undergone complete resection, in the adjuvant setting. (1.2) • patients with metastatic non-small cell lung cancer and progression on or after platinum-based chemotherapy. Patients with EGFT or ALK genomic tumor aberrations should have disease progression on FDA-approved therapy for these aberrations prior to receiving OPDIVO. (1.3) • patients with advanced renal cell carcinoma who have received prior anti-angiogenic therapy. (1.4) • adult patients with classical Hodgkin lymphoma that has relapsed or progressed afterb: (1.5) o autologous hematopoietic stem cell transplantation (HSCT) and brentuximab vedotin, or o 3 or more lines of systemic therapy that includes autologous HSCT. • patients with recurrent or metastatic squamous cell carcinoma of the head and neck with disease progression on or after a platinum-based therapy (1.6) • patients with locally advanced or metastatic urothelial carcinoma whob: o have disease progression during or following platinum-containing chemotherapy o have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum- containing chemotherapy. -
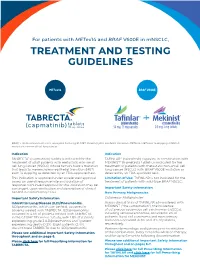
Treatment and Testing Guidelines
For patients with METex14 and BRAF V600E in mNSCLC, TREATMENT AND TESTING GUIDELINES METex14 BRAF V600E BRAF, v-raf murine sarcoma viral oncogene homolog B1; MET, mesenchymal-epithelial transition; METex14, MET exon 14 skipping; mNSCLC, metastatic non-small cell lung cancer. Indication Indication TABRECTA® (capmatinib) tablets is indicated for the TAFINLAR® (dabrafenib) capsules, in combination with treatment of adult patients with metastatic non-small MEKINIST® (trametinib) tablets, is indicated for the cell lung cancer (NSCLC) whose tumors have a mutation treatment of patients with metastatic non-small cell that leads to mesenchymal-epithelial transition (MET) lung cancer (NSCLC) with BRAF V600E mutation as exon 14 skipping as detected by an FDA-approved test. detected by an FDA-approved test. This indication is approved under accelerated approval Limitation of Use: TAFINLAR is not indicated for the based on overall response rate and duration of treatment of patients with wild-type BRAF NSCLC. response. Continued approval for this indication may be contingent upon verification and description of clinical Important Safety Information benefit in confirmatory trials. New Primary Malignancies. Important Safety Information Cutaneous Malignancies Interstitial Lung Disease (ILD)/Pneumonitis. Across clinical trials of TAFINLAR administered with ILD/pneumonitis, which can be fatal, occurred in MEKINIST (“the combination”), the incidence patients treated with TABRECTA. ILD/pneumonitis of cutaneous squamous cell carcinomas (cuSCCs), occurred in 4.5% of patients treated with TABRECTA including keratoacanthomas, occurred in 2% of in the GEOMETRY mono-1 study, with 1.8% of patients patients. Basal cell carcinoma and new primary experiencing grade 3 ILD/pneumonitis and 1 patient melanoma occurred in 3% and <1% of patients, experiencing death (0.3%). -

Combined BRAF and MEK Inhibition with Vemurafenib and Cobimetinib for Patients with Advanced Melanoma
Review Melanoma Combined BRAF and MEK Inhibition with Vemurafenib and Cobimetinib for Patients with Advanced Melanoma Antonio M Grimaldi, Ester Simeone, Lucia Festino, Vito Vanella and Paolo A Ascierto Melanoma, Cancer Immunotherapy and Innovative Therapy Unit, Istituto Nazionale Tumori Fondazione “G. Pascale”, Napoli, Italy cquired resistance is the most common cause of BRAF inhibitor monotherapy treatment failure, with the majority of patients experiencing disease progression with a median progression-free survival of 6-8 months. As such, there has been considerable A focus on combined therapy with dual BRAF and MEK inhibition as a means to improve outcomes compared with monotherapy. In the COMBI-d and COMBI-v trials, combined dabrafenib and trametinib was associated with significant improvements in outcomes compared with dabrafenib or vemurafenib monotherapy, in patients with BRAF-mutant metastatic melanoma. The combination of vemurafenib and cobimetinib has also been investigated. In the phase III CoBRIM study in patients with unresectable stage III-IV BRAF-mutant melanoma, treatment with vemurafenib and cobimetinib resulted in significantly longer progression-free survival and overall survival (OS) compared with vemurafenib alone. One-year OS was 74.5% in the vemurafenib and cobimetinib group and 63.8% in the vemurafenib group, while 2-year OS rates were 48.3% and 38.0%, respectively. The combination was also well tolerated, with a lower incidence of cutaneous squamous-cell carcinoma and keratoacanthoma compared with monotherapy. Dual inhibition of both MEK and BRAF appears to provide a more potent and durable anti-tumour effect than BRAF monotherapy, helping to prevent acquired resistance as well as decreasing adverse events related to BRAF inhibitor-induced activation of the MAPK-pathway. -

Tabrecta (Capmatinib)
Tabrecta (capmatinib) NEW PRODUCT SLIDESHOW Introduction . Brand name: Tabrecta . Generic name: Capmatinib . Pharmacologic class: Kinase inhibitor . Strength and Formulation: 150mg, 200mg; tablets . Manufacturer: Novartis . How supplied: Tabs—56 . Legal Classification: Rx Tabrecta Indication Treatment of adult patients with metastatic non-small cell lung cancer (NSCLC) whose tumors have a mutation that leads to mesenchymal-epithelial transition (MET) exon 14 skipping as detected by an FDA- approved test . Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trial(s) Dosage and Administration Confirm presence of a mutation that leads to MET exon 14 skipping in tumor specimens Swallow whole 400mg twice daily Recommended dose reductions for adverse reactions: . First: 300mg twice daily . Second: 200mg twice daily . Permanently discontinue in patients unable to tolerate 200mg twice daily Dosage Modifications for Adverse Reactions Interstitial lung disease/pneumonitis . Any grade: permanently discontinue Increased ALT and/or AST without increased total bilirubin . Grade 3: withhold until recovery to baseline ALT/AST; if recovery to baseline within 7 days, then resume at same dose, otherwise resume at a reduced dose . Grade 4: permanently discontinue Increased ALT and/or AST with increased total bilirubin in the absence of cholestasis or hemolysis . ALT and/or AST >3xULN with total bilirubin >2xULN: permanently discontinue Dosage Modifications for Adverse Reactions Increased total bilirubin without concurrent increased ALT and/or AST . Grade 2: withhold until recovery to baseline bilirubin; if recovered to baseline within 7 days, then resume at same dose, otherwise resume at reduced dose . Grade 3: withhold until recovery to baseline bilirubin; if recovered to baseline within 7 days, then resume at reduced dose, otherwise permanently discontinue .