Dual Kinase Targeting in Leukemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer
diagnostics Review Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer Shunsuke Kato Department of Clinical Oncology, Juntendo University Graduate School of Medicine, 2-1-1, Hongo, Bunkyo-ku, Tokyo 113-8421, Japan; [email protected]; Tel.: +81-3-5802-1543 Abstract: The prognosis of patients with solid tumours has remarkably improved with the develop- ment of molecular-targeted drugs and immune checkpoint inhibitors. However, the improvements in the prognosis of pancreatic cancer and biliary tract cancer is delayed compared to other carcinomas, and the 5-year survival rates of distal-stage disease are approximately 10 and 20%, respectively. How- ever, a comprehensive analysis of tumour cells using The Cancer Genome Atlas (TCGA) project has led to the identification of various driver mutations. Evidently, few mutations exist across organs, and basket trials targeting driver mutations regardless of the primary organ are being actively conducted. Such basket trials not only focus on the gate keeper-type oncogene mutations, such as HER2 and BRAF, but also focus on the caretaker-type tumour suppressor genes, such as BRCA1/2, mismatch repair-related genes, which cause hereditary cancer syndrome. As oncogene panel testing is a vital approach in routine practice, clinicians should devise a strategy for improved understanding of the cancer genome. Here, the gene mutation profiles of pancreatic cancer and biliary tract cancer have been outlined and the current status of tumour-agnostic therapy in these cancers has been reported. Keywords: pancreatic cancer; biliary tract cancer; targeted therapy; solid tumours; driver mutations; agonist therapy Citation: Kato, S. Tumour-Agnostic Therapy for Pancreatic Cancer and 1. -
![[1,2,5]Thiadiazolo[3,4-D]Pyridazine As an Internal Acceptor in the DA-Π-A](https://docslib.b-cdn.net/cover/3156/1-2-5-thiadiazolo-3-4-d-pyridazine-as-an-internal-acceptor-in-the-da-a-93156.webp)
[1,2,5]Thiadiazolo[3,4-D]Pyridazine As an Internal Acceptor in the DA-Π-A
Article [1,2,5]Thiadiazolo[3,4-d]Pyridazine as an Internal Acceptor in the D-A-π-A Organic Sensitizers for Dye- Sensitized Solar Cells Timofey N. Chmovzh 1, Ekaterina A. Knyazeva 1,2, Ellie Tanaka 3, Vadim V. Popov 2, Ludmila V. Mikhalchenko 1, Neil Robertson 3,* and Oleg A. Rakitin 1,2,* 1 N. D. Zelinsky Institute of Organic Chemistry, Russian Academy of Sciences, 119991 Moscow, Russia; [email protected] (O.A.R.); [email protected] (T.N.C.); [email protected] (E.A.K.); [email protected] (L.V.M.) 2 Nanotechnology Education and Research Center, South Ural State University, 454080 Chelyabinsk, Russia; [email protected] 3 EaStCHEM School of Chemistry, University of Edinburgh, Edinburgh EH9 3FJ, UK; [email protected] * Correspondence: Correspondence: [email protected] (N.R.); [email protected] (O.A.R.); Tel.: +44-131-650-4755 (N.R.); +7-499-135-5327(O.A.R.) Academic Editor: Panayiotis A. Koutentis Received: 4 April 2019; Accepted: 19 April 2019; Published: 22 April 2019 Abstract: Four new D-A-π-A metal-free organic sensitizers for dye-sensitized solar cells (DSSCs), with [1,2,5]thiadiazolo[3 ,4-d]pyridazine as internal acceptor, thiophene unit as π-spacer and cyanoacrylate as anchoring electron acceptor, have been synthesized. The donor moiety was introduced into [1,2,5]thiadiazolo[3,4-d]pyridazine by nucleophilic aromatic substitution and Suzuki cross-coupling reactions, allowing design of D-A-π-A sensitizers with the donor attached to the internal heterocyclic acceptor not only by the carbon atom, as it is in a majority of DSSCs, but by the nitrogen atom also. -

WHO Drug Information Vol
WHO Drug Information Vol. 31, No. 3, 2017 WHO Drug Information Contents Medicines regulation 420 Post-market monitoring EMA platform gains trade mark; Automated 387 Regulatory systems in India FDA field alert reports 421 GMP compliance Indian manufacturers to submit self- WHO prequalification certification 421 Collaboration 402 Prequalification process quality China Food and Drug Administration improvement initiatives: 2010–2016 joins ICH; U.S.-EU cooperation in inspections; IGDRP, IPRF initiatives to join 422 Medicines labels Safety news Improved labelling in Australia 423 Under discussion 409 Safety warnings 425 Approved Brimonidine gel ; Lactose-containing L-glutamine ; Betrixaban ; C1 esterase injectable methylprednisolone inhibitor (human) ; Meropenem and ; Amoxicillin; Azithromycin ; Fluconazole, vaborbactam ; Delafloxacin ; Glecaprevir fosfluconazole ; DAAs and warfarin and pibrentasvir ; Sofosbuvir, velpatasvir ; Bendamustine ; Nivolumab ; Nivolumab, and voxilaprevir ; Cladribine ; Daunorubicin pembrolizumab ; Atezolizumab ; Ibrutinib and cytarabine ; Gemtuzumab ozogamicin ; Daclizumab ; Loxoprofen topical ; Enasidenib ; Neratinib ; Tivozanib ; preparations ; Denosumab ; Gabapentin Guselkumab ; Benznidazole ; Ciclosporin ; Hydroxocobalamine antidote kit paediatric eye drops ; Lutetium oxodotreotide 414 Diagnostics Gene cell therapy Hightop HIV home testing kits Tisagenlecleucel 414 Known risks Biosimilars Warfarin ; Local corticosteroids Bevacizumab; Adalimumab ; Hydroquinone skin lighteners Early access 415 Review outcomes Idebenone -
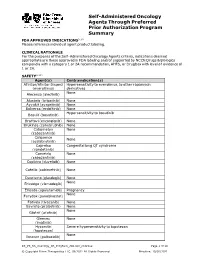
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

Clinical Response of the Novel Activating ALK-I1171T
http://www.diva-portal.org This is the published version of a paper published in Cold Spring Harbor Molecular Case Studies. Citation for the original published paper (version of record): Guan, J., Fransson, S., Siaw, J T., Treis, D., Van den Eynden, J. et al. (2018) Clinical response of the novel activating ALK-I1171T mutation in neuroblastoma o the ALK inhibitor ceritinib Cold Spring Harbor Molecular Case Studies, 4(4): a002550 https://doi.org/10.1101/mcs.a002550 Access to the published version may require subscription. N.B. When citing this work, cite the original published paper. Permanent link to this version: http://urn.kb.se/resolve?urn=urn:nbn:se:umu:diva-154087 Downloaded from molecularcasestudies.cshlp.org on December 12, 2018 - Published by Cold Spring Harbor Laboratory Press COLD SPRING HARBOR Molecular Case Studies | RESEARCH ARTICLE Clinical response of the novel activating ALK-I1171T mutation in neuroblastoma to the ALK inhibitor ceritinib Jikui Guan,1,2,12 Susanne Fransson,3,12 Joachim Tetteh Siaw,1,12 Diana Treis,4,12 Jimmy Van den Eynden,1 Damini Chand,1 Ganesh Umapathy,1 Kristina Ruuth,5 Petter Svenberg,4 Sandra Wessman,6,7 Alia Shamikh,6,7 Hans Jacobsson,8 Lena Gordon,9 Jakob Stenman,10 Pär-Johan Svensson,10 Magnus Hansson,11 Erik Larsson,1 Tommy Martinsson,3 Ruth H. Palmer,1 Per Kogner,6,7 and Bengt Hallberg1 1Department of Medical Biochemistry and Cell Biology, Institute of Biomedicine, The Sahlgrenska Academy, University of Gothenburg, Gothenburg 40530, Sweden; 2Children’s Hospital Affiliated to Zhengzhou University, -

The Drug Sensitivity and Resistance Testing (DSRT) Approach
A phenotypic screening and machine learning platform eciently identifies triple negative breast cancer-selective and readily druggable targets Prson Gautam 1 Alok Jaiswal 1 Tero Aittokallio 1, 2 Hassan Al Ali 3 Krister Wennerberg 1,4 Identifying eective oncogenic targets is challenged by the complexity of genetic alterations in 1Institute for Molecular Medicine Finland (FIMM), HiLIFE, University of Helsinki, Finland cancer and their poorly understood relation to cell function and survival. There is a need for meth- Current kinome coverage of kinase inhibitors in TNBC exhibit diverse kinase dependencies MFM-223 is selectively addicted to FGFR2 2Department of Mathematics and Statistics, University of Turku, Finland 3The Miami Project to Cure Paralysis, Peggy and Harold Katz Family Drug Discovery Center, A A Sylvester Comprehensive Cancer Center, and Department of Neurological Surgery and Medicine ods that rapidly and accurately identify “pharmacologically eective” targets without the require- clinical evaluation TN Kinases MFM-223 CAL-120 MDA-MB-231 TNBC TNBC TNBC TNBC TNBC TNBC HER2+ 100 University of Miami Miller School of Medicine, Miami, FL 33136, USA. non- HER2+ FGFR1 0.97 0.00 0.00 MFM-223 BL1 BL2 M MSL IM LAR ER+, PR+ 50 ment for priori knowledge of complex signaling networks. We developed an approach that uses ma- cancerous FGFR2 56.46 0.00 0.00 CAL-120 25 4 MDA-MB-231 Biotech Research & Innovation Centre (BRIC) and Novo Nordisk Foundation Center HCC1937 CAL-85-1 CAL-120 MDA-MB-231 DU4475 CAL-148 MCF-10A SK-BR-3 BT-474 FGFR3 25.10 0.00 0.00 0 chine learning to relate results from unbiased phenotypic screening of kinase inhibitors to their bio- for Stem Cell Biology (DanStem), University of Copenhagen, Denmark HCC1599 HDQ-P1 BT-549 MDA-MB-436 MFM-223 FGFR4 0.00 0.00 0.00 MAXIS*Bk Clinical status MDA-MB-468 CAL-51 Hs578T MDA-MB-453 score chemical activity data. -

Pharmacy Pre-Authorization Criteria
PHARMACY PRE-AUTHORIZATION CRITERIA DRUG (S) Oncology Medications: Sprycel (dasatinib) Afinitor (everolimus) Stivarga (regorafenib) Caprelsa (vandetanib) Sutent (sunitinib) Gilotrif (afatinib dimaleate) Tarceva (erlotinob) Gleevec (imatinib mesylate) Temodar (temozolomide) Ibrance (palbociclib) Tepadina (thiotepa) Idhifa (enasidenib) Thalomid (thalidomide) Iressa (gefitinib) Vantas (histrelin acetate) Kisqali (ribociclib) Venclexta (venetoclax) Lenvima (lenvatinib) Verzenio (abemaciclib) Nerlynx (neratinib) Vidaza (azacitidine) Nexavar (sorafenib) Votrient (pazopanib) Ninlaro (ixazomib) Xalkori (crizotinib) Odomzo (sonidegib) Xeloda (capecitabine) Zydelig (idelalisib) Zykadia (certinib) Zytiga (abiraterone acetate) PHARMACY PRE-AUTHORIZATION CRITERIA POLICY # 21107 CRITERIA The above medications are covered when the following criteria are met: 1. Ordered by an oncologist or hematologist AND 2. All FDA Approved Indications OR 3. Chemo agent is listed in an accepted Compendia for treatment of cancer type, OR - National Comprehensive Cancer Network (NCCN) Drugs and Biologics Compendium, level of evidence 1, 2A, or 2B - Thomson Micromedex DrugDex - Chemo agent is recommended for cancer type in formal clinical studies published in at least 2 peer reviewed professional medical journals, published in the United States or Great Britain Coverage Duration: Initial: 3 months Continuation: 6 months. Afinitor, Gilotrif, Gleevec, Ibrance, Idhifa, Iressa, Kisqali, Lenvima, Nexavar, Ninlaro, Odomzo, Sprycel, Stivarga, Sutent, Tarceva, Temodar, Thalomid, -

ZYKADIA (Ceritinib) RATIONALE for INCLUSION in PA PROGRAM
ZYKADIA (ceritinib) RATIONALE FOR INCLUSION IN PA PROGRAM Background Zykadia is used in patients with a certain type of late-stage (metastatic) non-small cell lung cancer (NSCLC), which is caused by a defect in a gene called anaplastic lymphoma kinase (ALK). Zykadia is a tyrosine kinase inhibitor that blocks proteins that promote the development of cancerous cells. It is intended for patients with metastatic ALK-positive NSCLC (1). Regulatory Status FDA- approved indication: Zykadia is a kinase inhibitor indicated for the treatment of patients with anaplastic lymphoma kinase (ALK)-positive metastatic non-small cell lung cancer (NSCLC) as detected by an FDA-approved test (1). Off-Label Uses: (2-3) 1. Inflammatory Myofibroblastic Tumor (IMT) with ALK translocation Zykadia can cause hepatotoxicity therefore liver function tests including AST, ALT and total bilirubin should be monitored at least monthly. Zykadia can cause interstitial lung disease (ILD) or pneumonitis. Zykadia should be permanently discontinued in patients diagnosed with treatment- related ILD/pneumonitis. Zykadia can cause QTc interval prolongation, which requires monitoring of electrocardiograms and electrolytes in patients with congestive heart failure (1). Zykadia is pregnancy category D and may cause fetal harm when administered to a pregnant woman (1). Safety and effectiveness of Zykadia in pediatric patients have not been established (1). Summary Zykadia is an anaplastic lymphoma kinase (ALK) tyrosine kinase inhibitor that blocks proteins that promote the development of cancerous cells. It is intended for patients with metastatic ALK-positive NSCLC. Safety and effectiveness of Zykadia in patients under 18 years of age have not been established (1). Zykadia FEP Clinical Rationale ZYKADIA (ceritinib) Prior approval is required to ensure the safe, clinically appropriate and cost effective use of Zykadia while maintaining optimal therapeutic outcomes. -

New Contributions in Undergraduate Research
PSU McNair Scholars Online Journal Volume 11 Issue 1 Without Borders: Original Contributions Article 6 in Undergraduate Research 2017 Wings Outstretched: New Contributions in Undergraduate Research Follow this and additional works at: https://pdxscholar.library.pdx.edu/mcnair Let us know how access to this document benefits ou.y Recommended Citation (2017) "Wings Outstretched: New Contributions in Undergraduate Research," PSU McNair Scholars Online Journal: Vol. 11: Iss. 1, Article 6. https://doi.org/10.15760/mcnair.2017.01 This open access Full Issue is distributed under the terms of the Creative Commons Attribution-NonCommercial- ShareAlike 4.0 International License (CC BY-NC-SA 4.0). All documents in PDXScholar should meet accessibility standards. If we can make this document more accessible to you, contact our team. Portland State University McNair Research Journal 2017 Without Borders: Original Contributions in Undergraduate Research 2017 Ronald E. McNair Scholars Journal Portland State University 1 About the Program The Portland State University (PSU) Ronald E. McNair Scholars Program at Portland State University works with motivated and talented undergraduates who want to pursue PhDs. It introduces juniors and seniors who are first-generation and low income, and/or members of under-represented groups to academic research and to effective strategies for getting into and graduating from PhD programs. The McNair Scholars Program has academic-year activities and a full-time summer research internship. Scholars take academic and skills-building seminars and workshops during the year, and each scholar works closely with a faculty mentor on original research in the summer. Scholars present their research findings at the McNair Summer Symposium and at other conferences, and are encouraged to publish their papers in the McNair Journal and other scholarly publications. -

Weak Interaction of the Antimetabolite Drug Methotrexate with a Cavitand Derivative
International Journal of Molecular Sciences Article Weak Interaction of the Antimetabolite Drug Methotrexate with a Cavitand Derivative Zsolt Preisz 1,2, Zoltán Nagymihály 3,4, Beáta Lemli 1,4 ,László Kollár 3,4 and Sándor Kunsági-Máté 1,2,4,* 1 Institute of Organic and Medicinal Chemistry, Medical School, University of Pécs, Szigeti 12, H-7624 Pécs, Hungary; [email protected] (Z.P.); [email protected] (B.L.) 2 Department of General and Physical Chemistry, Faculty of Sciences, University of Pécs, Ifjúság 6, H 7624 Pécs, Hungary 3 Department of Inorganic Chemistry, Faculty of Sciences, University of Pécs, Ifjúság 6, H 7624 Pécs, Hungary; [email protected] (Z.N.); [email protected] (L.K.) 4 János Szentágothai Research Center, University of Pécs, Ifjúság 20, H-7624 Pécs, Hungary * Correspondence: [email protected]; Tel.: +36-72-503600 (ext. 35449) Received: 2 June 2020; Accepted: 16 June 2020; Published: 18 June 2020 Abstract: Formation of inclusion complexes involving a cavitand derivative (as host) and an antimetabolite drug, methotrexate (as guest) was investigated by photoluminescence measurements in dimethyl sulfoxide solvent. Molecular modeling performed in gas phase reflects that, due to the structural reasons, the cavitand can include the methotrexate in two forms: either by its opened structure with free androsta-4-en-3-one-17α-ethinyl arms or by the closed form when all the androsta-4-en-3-one-17α-ethinyl arms play role in the complex formation. Experiments reflect enthalpy driven complex formation in higher temperature range while at lower temperature the complexes are stabilized by the entropy gain. -

Antibody–Drug Conjugates
Published OnlineFirst April 12, 2019; DOI: 10.1158/1078-0432.CCR-19-0272 Review Clinical Cancer Research Antibody–Drug Conjugates: Future Directions in Clinical and Translational Strategies to Improve the Therapeutic Index Steven Coats1, Marna Williams1, Benjamin Kebble1, Rakesh Dixit1, Leo Tseng1, Nai-Shun Yao1, David A. Tice1, and Jean-Charles Soria1,2 Abstract Since the first approval of gemtuzumab ozogamicin nism of activity of the cytotoxic warhead. However, the (Mylotarg; Pfizer; CD33 targeted), two additional antibody– enthusiasm to develop ADCs has not been dampened; drug conjugates (ADC), brentuximab vedotin (Adcetris; Seat- approximately 80 ADCs are in clinical development in tle Genetics, Inc.; CD30 targeted) and inotuzumab ozogami- nearly 600 clinical trials, and 2 to 3 novel ADCs are likely cin (Besponsa; Pfizer; CD22 targeted), have been approved for to be approved within the next few years. While the hematologic cancers and 1 ADC, trastuzumab emtansine promise of a more targeted chemotherapy with less tox- (Kadcyla; Genentech; HER2 targeted), has been approved to icity has not yet been realized with ADCs, improvements treat breast cancer. Despite a clear clinical benefit being dem- in technology combined with a wealth of clinical data are onstrated for all 4 approved ADCs, the toxicity profiles are helping to shape the future development of ADCs. In this comparable with those of standard-of-care chemotherapeu- review, we discuss the clinical and translational strategies tics, with dose-limiting toxicities associated with the mecha- associated with improving the therapeutic index for ADCs. Introduction in antibody, linker, and warhead technologies in significant depth (2, 3, 8, 9). Antibody–drug conjugates (ADC) were initially designed to leverage the exquisite specificity of antibodies to deliver targeted potent chemotherapeutic agents with the intention of improving Overview of ADCs in Clinical Development the therapeutic index (the ratio between the toxic dose and the Four ADCs have been approved over the last 20 years (Fig. -
Public Assessment Report
Public Assessment Report Tifix 150mg and 500mg film-coated tablets Capecitabine BE/H/195/01-02/DC BE licence no: BE423552-BE423561 Applicant: Alfred E. Tiefenbacher, Germany Date: 27-04-2012 Toepassingsdatum : 15-09-10 Page 1 of 17 Blz. 1 van 17 This assessment report is published by the Federal Agency for Medicines and Health Products following Article 21 (3) and (4) of Directive 2001/83/EC, amended by Directive 2004/27/EC and Article 25 paragraph 4 of Directive 2001/82/EC as amended by 2004/28/EC. The report comments on the registration dossier that was submitted to the Federal Agency for Medicines and Health Products and its fellow organisations in all concerned EU member states. It reflects the scientific conclusion reached by the Federal Agency for Medicines and Health Products and all concerned member states at the end of the evaluation process and provides a summary of the grounds for approval of a marketing authorisation. This report is intended for all those involved with the safe and proper use of the medicinal product, i.e. healthcare professionals, patients and their family and carers. Some knowledge of medicines and diseases is expected of the latter category as the language in this report may be difficult for laymen to understand. This assessment report shall be updated by a following addendum whenever new information becomes available. To the best of the Federal Agency for Medicines and Health Products’ knowledge, this report does not contain any information that should not have been made available to the public. The Marketing Autorisation Holder has checked this report for the absence of any confidential information.