New Directions for Emerging Therapies in Acute Myeloid Leukemia: the Next Chapter Naval Daver 1,Andrewh.Wei2, Daniel A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The TP53 Apoptotic Network Is a Primary Mediator of Resistance to BCL2 Inhibition in AML Cells
Published OnlineFirst May 2, 2019; DOI: 10.1158/2159-8290.CD-19-0125 RESEARCH ARTICLE The TP53 Apoptotic Network Is a Primary Mediator of Resistance to BCL2 Inhibition in AML Cells Tamilla Nechiporuk1,2, Stephen E. Kurtz1,2, Olga Nikolova2,3, Tingting Liu1,2, Courtney L. Jones4, Angelo D’Alessandro5, Rachel Culp-Hill5, Amanda d’Almeida1,2, Sunil K. Joshi1,2, Mara Rosenberg1,2, Cristina E. Tognon1,2,6, Alexey V. Danilov1,2, Brian J. Druker1,2,6, Bill H. Chang2,7, Shannon K. McWeeney2,8, and Jeffrey W. Tyner1,2,9 ABSTRACT To study mechanisms underlying resistance to the BCL2 inhibitor venetoclax in acute myeloid leukemia (AML), we used a genome-wide CRISPR/Cas9 screen to identify gene knockouts resulting in drug resistance. We validated TP53, BAX, and PMAIP1 as genes whose inactivation results in venetoclax resistance in AML cell lines. Resistance to venetoclax resulted from an inability to execute apoptosis driven by BAX loss, decreased expression of BCL2, and/or reliance on alternative BCL2 family members such as BCL2L1. The resistance was accompanied by changes in mitochondrial homeostasis and cellular metabolism. Evaluation of TP53 knockout cells for sensitivities to a panel of small-molecule inhibitors revealed a gain of sensitivity to TRK inhibitors. We relate these observations to patient drug responses and gene expression in the Beat AML dataset. Our results implicate TP53, the apoptotic network, and mitochondrial functionality as drivers of venetoclax response in AML and suggest strategies to overcome resistance. SIGNIFICANCE: AML is challenging to treat due to its heterogeneity, and single-agent therapies have universally failed, prompting a need for innovative drug combinations. -

Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer
diagnostics Review Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer Shunsuke Kato Department of Clinical Oncology, Juntendo University Graduate School of Medicine, 2-1-1, Hongo, Bunkyo-ku, Tokyo 113-8421, Japan; [email protected]; Tel.: +81-3-5802-1543 Abstract: The prognosis of patients with solid tumours has remarkably improved with the develop- ment of molecular-targeted drugs and immune checkpoint inhibitors. However, the improvements in the prognosis of pancreatic cancer and biliary tract cancer is delayed compared to other carcinomas, and the 5-year survival rates of distal-stage disease are approximately 10 and 20%, respectively. How- ever, a comprehensive analysis of tumour cells using The Cancer Genome Atlas (TCGA) project has led to the identification of various driver mutations. Evidently, few mutations exist across organs, and basket trials targeting driver mutations regardless of the primary organ are being actively conducted. Such basket trials not only focus on the gate keeper-type oncogene mutations, such as HER2 and BRAF, but also focus on the caretaker-type tumour suppressor genes, such as BRCA1/2, mismatch repair-related genes, which cause hereditary cancer syndrome. As oncogene panel testing is a vital approach in routine practice, clinicians should devise a strategy for improved understanding of the cancer genome. Here, the gene mutation profiles of pancreatic cancer and biliary tract cancer have been outlined and the current status of tumour-agnostic therapy in these cancers has been reported. Keywords: pancreatic cancer; biliary tract cancer; targeted therapy; solid tumours; driver mutations; agonist therapy Citation: Kato, S. Tumour-Agnostic Therapy for Pancreatic Cancer and 1. -
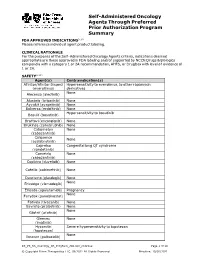
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

Pharmacy Pre-Authorization Criteria
PHARMACY PRE-AUTHORIZATION CRITERIA DRUG (S) Oncology Medications: Sprycel (dasatinib) Afinitor (everolimus) Stivarga (regorafenib) Caprelsa (vandetanib) Sutent (sunitinib) Gilotrif (afatinib dimaleate) Tarceva (erlotinob) Gleevec (imatinib mesylate) Temodar (temozolomide) Ibrance (palbociclib) Tepadina (thiotepa) Idhifa (enasidenib) Thalomid (thalidomide) Iressa (gefitinib) Vantas (histrelin acetate) Kisqali (ribociclib) Venclexta (venetoclax) Lenvima (lenvatinib) Verzenio (abemaciclib) Nerlynx (neratinib) Vidaza (azacitidine) Nexavar (sorafenib) Votrient (pazopanib) Ninlaro (ixazomib) Xalkori (crizotinib) Odomzo (sonidegib) Xeloda (capecitabine) Zydelig (idelalisib) Zykadia (certinib) Zytiga (abiraterone acetate) PHARMACY PRE-AUTHORIZATION CRITERIA POLICY # 21107 CRITERIA The above medications are covered when the following criteria are met: 1. Ordered by an oncologist or hematologist AND 2. All FDA Approved Indications OR 3. Chemo agent is listed in an accepted Compendia for treatment of cancer type, OR - National Comprehensive Cancer Network (NCCN) Drugs and Biologics Compendium, level of evidence 1, 2A, or 2B - Thomson Micromedex DrugDex - Chemo agent is recommended for cancer type in formal clinical studies published in at least 2 peer reviewed professional medical journals, published in the United States or Great Britain Coverage Duration: Initial: 3 months Continuation: 6 months. Afinitor, Gilotrif, Gleevec, Ibrance, Idhifa, Iressa, Kisqali, Lenvima, Nexavar, Ninlaro, Odomzo, Sprycel, Stivarga, Sutent, Tarceva, Temodar, Thalomid, -

211192Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 211192Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRISK) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 211192 PDUFA Goal Date August 21, 2018 OSE RCM # 2017-2612; 2017-2614 Reviewer Name(s) Till Olickal, Ph.D., Pharm.D. Team Leader Elizabeth Everhart, MSN, RN, ACNP Division Director Cynthia LaCivita, Pharm.D. Review Completion Date June 6, 2018 Subject Review to determine if a REMS is necessary Established Name Ivosidenib Trade Name Tibsovo Name of Applicant Agios Pharmaceuticals, Inc. Therapeutic Class Isocitrate dehydrogenase-1 inhibitor Formulation(s) 250 mg tablet Dosing Regimen 500 mg orally once daily until disease progression or unacceptable toxicity. 1 Reference ID: 4273770 Table of Contents EXECUTIVE SUMMARY ......................................................................................................................................................... 3 1 Introduction ..................................................................................................................................................................... 3 2 Background ...................................................................................................................................................................... 3 2.1 Product Information .......................................................................................................................................... -

Signal Transduction Guide
Signal Transduction Product Guide | 2007 NEW! Selective T-type Ca2+ channel blockers, NNC 55-0396 and Mibefradil ZM 447439 – Novel Aurora Kinase Inhibitor NEW! Antibodies for Cancer Research EGFR-Kinase Selective Inhibitors – BIBX 1382 and BIBU 1361 DRIVING RESEARCH FURTHER Calcium Signaling Agents ...................................2 G Protein Reagents ...........................................12 Cell Cycle and Apoptosis Reagents .....................3 Ion Channel Modulators ...................................13 Cyclic Nucleotide Related Tools ...........................7 Lipid Signaling Agents ......................................17 Cytokine Signaling Agents ..................................9 Nitric Oxide Tools .............................................19 Enzyme Inhibitors/Substrates/Activators ..............9 Protein Kinase Reagents....................................22 Glycobiology Agents .........................................12 Protein Phosphatase Reagents ..........................33 Neurochemicals | Signal Transduction Agents | Peptides | Biochemicals Signal Transduction Product Guide Calcium Signaling Agents ......................................................................................................................2 Calcium Binding Protein Modulators ...................................................................................................2 Calcium ATPase Modulators .................................................................................................................2 Calcium Sensitive Protease -

New Contributions in Undergraduate Research
PSU McNair Scholars Online Journal Volume 11 Issue 1 Without Borders: Original Contributions Article 6 in Undergraduate Research 2017 Wings Outstretched: New Contributions in Undergraduate Research Follow this and additional works at: https://pdxscholar.library.pdx.edu/mcnair Let us know how access to this document benefits ou.y Recommended Citation (2017) "Wings Outstretched: New Contributions in Undergraduate Research," PSU McNair Scholars Online Journal: Vol. 11: Iss. 1, Article 6. https://doi.org/10.15760/mcnair.2017.01 This open access Full Issue is distributed under the terms of the Creative Commons Attribution-NonCommercial- ShareAlike 4.0 International License (CC BY-NC-SA 4.0). All documents in PDXScholar should meet accessibility standards. If we can make this document more accessible to you, contact our team. Portland State University McNair Research Journal 2017 Without Borders: Original Contributions in Undergraduate Research 2017 Ronald E. McNair Scholars Journal Portland State University 1 About the Program The Portland State University (PSU) Ronald E. McNair Scholars Program at Portland State University works with motivated and talented undergraduates who want to pursue PhDs. It introduces juniors and seniors who are first-generation and low income, and/or members of under-represented groups to academic research and to effective strategies for getting into and graduating from PhD programs. The McNair Scholars Program has academic-year activities and a full-time summer research internship. Scholars take academic and skills-building seminars and workshops during the year, and each scholar works closely with a faculty mentor on original research in the summer. Scholars present their research findings at the McNair Summer Symposium and at other conferences, and are encouraged to publish their papers in the McNair Journal and other scholarly publications. -

Identification of Candidate Repurposable Drugs to Combat COVID-19 Using a Signature-Based Approach
www.nature.com/scientificreports OPEN Identifcation of candidate repurposable drugs to combat COVID‑19 using a signature‑based approach Sinead M. O’Donovan1,10, Ali Imami1,10, Hunter Eby1, Nicholas D. Henkel1, Justin Fortune Creeden1, Sophie Asah1, Xiaolu Zhang1, Xiaojun Wu1, Rawan Alnafsah1, R. Travis Taylor2, James Reigle3,4, Alexander Thorman6, Behrouz Shamsaei4, Jarek Meller4,5,6,7,8 & Robert E. McCullumsmith1,9* The COVID‑19 pandemic caused by the novel SARS‑CoV‑2 is more contagious than other coronaviruses and has higher rates of mortality than infuenza. Identifcation of efective therapeutics is a crucial tool to treat those infected with SARS‑CoV‑2 and limit the spread of this novel disease globally. We deployed a bioinformatics workfow to identify candidate drugs for the treatment of COVID‑19. Using an “omics” repository, the Library of Integrated Network‑Based Cellular Signatures (LINCS), we simultaneously probed transcriptomic signatures of putative COVID‑19 drugs and publicly available SARS‑CoV‑2 infected cell lines to identify novel therapeutics. We identifed a shortlist of 20 candidate drugs: 8 are already under trial for the treatment of COVID‑19, the remaining 12 have antiviral properties and 6 have antiviral efcacy against coronaviruses specifcally, in vitro. All candidate drugs are either FDA approved or are under investigation. Our candidate drug fndings are discordant with (i.e., reverse) SARS‑CoV‑2 transcriptome signatures generated in vitro, and a subset are also identifed in transcriptome signatures generated from COVID‑19 patient samples, like the MEK inhibitor selumetinib. Overall, our fndings provide additional support for drugs that are already being explored as therapeutic agents for the treatment of COVID‑19 and identify promising novel targets that are worthy of further investigation. -

FLT3 Inhibitors in Acute Myeloid Leukemia Mei Wu1, Chuntuan Li2 and Xiongpeng Zhu2*
Wu et al. Journal of Hematology & Oncology (2018) 11:133 https://doi.org/10.1186/s13045-018-0675-4 REVIEW Open Access FLT3 inhibitors in acute myeloid leukemia Mei Wu1, Chuntuan Li2 and Xiongpeng Zhu2* Abstract FLT3 mutations are one of the most common findings in acute myeloid leukemia (AML). FLT3 inhibitors have been in active clinical development. Midostaurin as the first-in-class FLT3 inhibitor has been approved for treatment of patients with FLT3-mutated AML. In this review, we summarized the preclinical and clinical studies on new FLT3 inhibitors, including sorafenib, lestaurtinib, sunitinib, tandutinib, quizartinib, midostaurin, gilteritinib, crenolanib, cabozantinib, Sel24-B489, G-749, AMG 925, TTT-3002, and FF-10101. New generation FLT3 inhibitors and combination therapies may overcome resistance to first-generation agents. Keywords: FMS-like tyrosine kinase 3 inhibitors, Acute myeloid leukemia, Midostaurin, FLT3 Introduction RAS, MEK, and PI3K/AKT pathways [10], and ultim- Acute myeloid leukemia (AML) remains a highly resist- ately causes suppression of apoptosis and differentiation ant disease to conventional chemotherapy, with a me- of leukemic cells, including dysregulation of leukemic dian survival of only 4 months for relapsed and/or cell proliferation [11]. refractory disease [1]. Molecular profiling by PCR and Multiple FLT3 inhibitors are in clinical trials for treat- next-generation sequencing has revealed a variety of re- ing patients with FLT3/ITD-mutated AML. In this re- current gene mutations [2–4]. New agents are rapidly view, we summarized the preclinical and clinical studies emerging as targeted therapy for high-risk AML [5, 6]. on new FLT3 inhibitors, including sorafenib, lestaurtinib, In 1996, FMS-like tyrosine kinase 3/internal tandem du- sunitinib, tandutinib, quizartinib, midostaurin, gilteriti- plication (FLT3/ITD) was first recognized as a frequently nib, crenolanib, cabozantinib, Sel24-B489, G-749, AMG mutated gene in AML [7]. -

Cstone Pharmaceuticals 基石藥業
Hong Kong Exchanges and Clearing Limited and The Stock Exchange of Hong Kong Limited take no responsibility for the contents of this announcement, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this announcement. The forward-looking statements made in this announcement relate only to the events or information as of the date on which the statements are made in this announcement. Except as required by law, we undertake no obligation to update or revise publicly any forward-looking statements, whether as a result of new information, future events or otherwise, after the date on which the statements are made or to reflect the occurrence of unanticipated events. You should read this announcement completely and with the understanding that our actual future results or performance may be materially different from what we expect. In this announcement, statements of, or references to, our intentions or those of any of our directors and/or our Company are made as of the date of this announcement. Any of these intentions may alter in light of future development. CStone Pharmaceuticals 基 石 藥 業 (Incorporated in the Cayman Islands with limited liability) (Stock Code: 2616) VOLUNTARY ANNOUNCEMENT CSTONE SUCCESSFULLY HOSTED THE FIRST U.S. R&D DAY IN NEW YORK CStone Pharmaceuticals (the “Company” or “CStone”) announces that it successfully hosted its 2020 U.S. R&D Day in New York City, the United States on January 21, 2020. -

ESMO 2019 Update
ESMO 2019 Update Axel Grothey Director, GI Oncology Research West Cancer Center Research Institute Encorafenib plus Cetuximab With or Without Binimetinib for BRAF V600E–Mutant Metastatic Colorectal Cancer: Expanded Results from a Randomized, 3-Arm, Phase 3 Study vs. the Choice of Either Irinotecan or FOLFIRI plus Cetuximab (BEACON CRC) Josep Tabernero, Axel Grothey, Eric Van Cutsem, Rona Yaeger, Harpreet Wasan, Takayuki Yoshino, Jayesh Desai, Fortunato Ciardiello, Fotios Loupakis, Yong Sang Hong, Neeltje Steeghs, Tormod Kyrre Guren, Hendrik-Tobias Arkenau, Pilar Garcia-Alfonso, Ashwin Gollerkeri, Michael Pickard, Kati Maharry, Janna Christy-Bittel, Lisa Anderson, and Scott Kopetz BEACON CRC: Binimetinib, Encorafenib, And Cetuximab COmbiNed to Treat BRAF-mutant ColoRectal Cancer 2 Study Design Patients with BRAFV600E mCRC with disease progression after 1 or 2 prior regimens; ECOG PS of 0 or 1; and no prior treatment with any RAF inhibitor, MEK inhibitor, or EGFR inhibitor Phase 3 Primary Endpoints: Safety Lead-in ENCORAFENIB + Triplet therapy BINIMETINIB + ENCORAFENIB + BINIMETINIB + CETUXIMAB Triplet vs Control n = 205 CETUXIMAB N = 30 OS R Doublet therapy (All randomized Pts) Encorafenib 300 mg PO daily 1:1:1 ENCORAFENIB + CETUXIMAB Binimetinib 45 mg PO bid n = 205 Cetuximab standard weekly ORR – dosing Blinded Central Control arm Review FOLFIRI + CETUXIMAB, or (1st 331 randomized Pts) irinotecan + CETUXIMAB n = 205 Randomization was stratified by ECOG PS (0 vs. 1), prior use of irinotecan (yes vs. no), and cetuximab source (US-licensed vs. EU-approved) Secondary Endpoints: Doublet vs Control and Triplet vs Doublet - OS & ORR, PFS, Safety QOL Assessments: EORTC QOL Questionnaire (QLQ C30), Functional Assessment of Cancer Therapy Colon Cancer, EuroQol 5D5L, and Patient Global Impression of Change). -

Chronic Lymphocytic Leukemia
Amsterdam, the Netherlands, June 14 – 17, 2012 Chronic lymphocytic leukemia - Clinical 1 assumed efficacy especially in high-risk situations (early relapse, unfavourable prognostic markers), was used in 202 patients. The overall survival in the CHOP-collective was significantly shorter than in the comparative group (p<0.0001) although median observation time was not significantly differ - 0144 ent. However, this observation might reflect a bias in the selection of high risk patients for this relapse treatment. No influence on survival was INFLUENCE OF DIFFERENT TREATMENT REGIMENS ON SURVIVAL IN observed in patients receiving a mitoxantrone-containing regimen at any PATIENTS WITH CHRONIC LYMPHOCYTIC LEUKEMIA - A META-ANALY - time during the treatment course. Summary and Conclusions. This meta- SIS OF THE GERMAN CLL STUDY GROUP (GCLLSG) analysis shows that the advances in the development of strategies for first- S Isfort 1, P Cramer 2, J Bahlo 2, R Busch 3, K Fischer 2, AM Fink 2, V Goede 2, T line therapies result in prolongation of treatment-free and overall survival Elter 2, M Bergmann 4, M Stauch 5, S Stilgenbauer 4, CM Wendtner 6, M Hallek 2, for patients with CLL and need of treatment. Chemoimmunotherapies pro - B Eichhorst 2 long the survival independently of the time point of chemoimmunotherapy 1Department of Medicine IV, University Hospital Aachen, Aachen, Germany administration (for first-line therapy or relapse). 2Department I of Internal Medicine, University Hospital of Cologne, Cologne, Germany 3 Institute for Medical Statistic and Epidemiology, Technical University Munich, 0145 Munich, Germany 4 Department III of Internal Medicine, University Hospital Ulm, Ulm, Germany A SINGLE-ARM MULTI-CENTER TRIAL OF BENDAMUSTINE GIVEN 5 Private practice and day time clinic for Hematology and Oncology, Kronach, WITH OFATUMUMAB (BENDOFA) IN PATIENTS WITH REFRACTORY OR Kronach, Germany RELAPSED CHRONIC LYMPHOCYTIC LEUKEMIA.