National Cancer Institute Cancer National
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Company Coverage Report
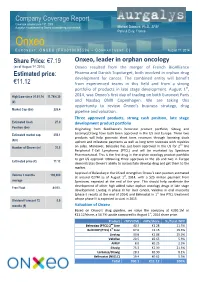
Company Coverage Report th Coverage initiated June 19 , 2009 Aurgalys is contracted by Onxeo to provide equity research Mickael Dubourd, Ph.D., SFAF Paris & Evry, France Onxeo E URONEXT : ONXEO [FR0010095596 – C OMPARTMENT C] August 1st, 2014 Share Price: €7.19 Onxeo, leader in orphan oncology (as of August 1st, 2014) Onxeo resulted from the merger of French BioAlliance Estimated price: Pharma and Danish Topotarget, both involved in orphan drug development for cancer. The combined entity will benefit €11.12 from experienced teams in this field and from a strong portfolio of products in late stage development. August 1st, High/Low since 01.01.14 11.74/4.30 2014, was Onxeo’s first day of trading on both Euronext Paris (€) and Nasdaq OMX Copenhagen. We are taking this opportunity to review Onxeo’s business strategy, drug Market Cap (€m) 226.4 pipeline and valuation. Three approved products, strong cash position, late stage Estimated Cash 27.0 development product portfolio Position (€m) Originating from BioAlliance's historical product portfolio, Sitavig and Estimated market cap. 350.1 Loramyc/Oravig have both been approved in the US and Europe. These two products will help generate short term revenues through licensing deals (€m) upfront and milestone payments as well as long term revenues with royalties nd Number of Shares (m) 31.5 on sales. Moreover, Beleodaq has just been approved in the US for 2 line Peripheral T-Cell Lymphoma (PTCL) and will be marketed by Spectrum Pharmaceutical. This is the first drug in the orphan oncology product portfolio to get US approval. -

New Contributions in Undergraduate Research
PSU McNair Scholars Online Journal Volume 11 Issue 1 Without Borders: Original Contributions Article 6 in Undergraduate Research 2017 Wings Outstretched: New Contributions in Undergraduate Research Follow this and additional works at: https://pdxscholar.library.pdx.edu/mcnair Let us know how access to this document benefits ou.y Recommended Citation (2017) "Wings Outstretched: New Contributions in Undergraduate Research," PSU McNair Scholars Online Journal: Vol. 11: Iss. 1, Article 6. https://doi.org/10.15760/mcnair.2017.01 This open access Full Issue is distributed under the terms of the Creative Commons Attribution-NonCommercial- ShareAlike 4.0 International License (CC BY-NC-SA 4.0). All documents in PDXScholar should meet accessibility standards. If we can make this document more accessible to you, contact our team. Portland State University McNair Research Journal 2017 Without Borders: Original Contributions in Undergraduate Research 2017 Ronald E. McNair Scholars Journal Portland State University 1 About the Program The Portland State University (PSU) Ronald E. McNair Scholars Program at Portland State University works with motivated and talented undergraduates who want to pursue PhDs. It introduces juniors and seniors who are first-generation and low income, and/or members of under-represented groups to academic research and to effective strategies for getting into and graduating from PhD programs. The McNair Scholars Program has academic-year activities and a full-time summer research internship. Scholars take academic and skills-building seminars and workshops during the year, and each scholar works closely with a faculty mentor on original research in the summer. Scholars present their research findings at the McNair Summer Symposium and at other conferences, and are encouraged to publish their papers in the McNair Journal and other scholarly publications. -

Chronic Lymphocytic Leukemia
Amsterdam, the Netherlands, June 14 – 17, 2012 Chronic lymphocytic leukemia - Clinical 1 assumed efficacy especially in high-risk situations (early relapse, unfavourable prognostic markers), was used in 202 patients. The overall survival in the CHOP-collective was significantly shorter than in the comparative group (p<0.0001) although median observation time was not significantly differ - 0144 ent. However, this observation might reflect a bias in the selection of high risk patients for this relapse treatment. No influence on survival was INFLUENCE OF DIFFERENT TREATMENT REGIMENS ON SURVIVAL IN observed in patients receiving a mitoxantrone-containing regimen at any PATIENTS WITH CHRONIC LYMPHOCYTIC LEUKEMIA - A META-ANALY - time during the treatment course. Summary and Conclusions. This meta- SIS OF THE GERMAN CLL STUDY GROUP (GCLLSG) analysis shows that the advances in the development of strategies for first- S Isfort 1, P Cramer 2, J Bahlo 2, R Busch 3, K Fischer 2, AM Fink 2, V Goede 2, T line therapies result in prolongation of treatment-free and overall survival Elter 2, M Bergmann 4, M Stauch 5, S Stilgenbauer 4, CM Wendtner 6, M Hallek 2, for patients with CLL and need of treatment. Chemoimmunotherapies pro - B Eichhorst 2 long the survival independently of the time point of chemoimmunotherapy 1Department of Medicine IV, University Hospital Aachen, Aachen, Germany administration (for first-line therapy or relapse). 2Department I of Internal Medicine, University Hospital of Cologne, Cologne, Germany 3 Institute for Medical Statistic and Epidemiology, Technical University Munich, 0145 Munich, Germany 4 Department III of Internal Medicine, University Hospital Ulm, Ulm, Germany A SINGLE-ARM MULTI-CENTER TRIAL OF BENDAMUSTINE GIVEN 5 Private practice and day time clinic for Hematology and Oncology, Kronach, WITH OFATUMUMAB (BENDOFA) IN PATIENTS WITH REFRACTORY OR Kronach, Germany RELAPSED CHRONIC LYMPHOCYTIC LEUKEMIA. -

Supporting Information
Supporting Information Pouryahya et al. SI Text Table S1 presents genes with the highest absolute value of Ricci curvature. We expect these genes to have significant contribution to the network’s robustness. Notably, the top two genes are TP53 (tumor protein 53) and YWHAG gene. TP53, also known as p53, it is a well known tumor suppressor gene known as the "guardian of the genome“ given the essential role it plays in genetic stability and prevention of cancer formation (1, 2). Mutations in this gene play a role in all stages of malignant transformation including tumor initiation, promotion, aggressiveness, and metastasis (3). Mutations of this gene are present in more than 50% of human cancers, making it the most common genetic event in human cancer (4, 5). Namely, p53 mutations play roles in leukemia, breast cancer, CNS cancers, and lung cancers, among many others (6–9). The YWHAG gene encodes the 14-3-3 protein gamma, a member of the 14-3-3 family proteins which are involved in many biological processes including signal transduction regulation, cell cycle pro- gression, apoptosis, cell adhesion and migration (10, 11). Notably, increased expression of 14-3-3 family proteins, including protein gamma, have been observed in a number of human cancers including lung and colorectal cancers, among others, suggesting a potential role as tumor oncogenes (12, 13). Furthermore, there is evidence that loss Fig. S1. The histogram of scalar Ricci curvature of 8240 genes. Most of the genes have negative scalar Ricci curvature (75%). TP53 and YWHAG have notably low of p53 function may result in upregulation of 14-3-3γ in lung cancer Ricci curvatures. -

Draft COMP Agenda 16-18 January 2018
12 January 2018 EMA/COMP/818236/2017 Inspections, Human Medicines Pharmacovigilance and Committees Committee for Orphan Medicinal Products (COMP) Draft agenda for the meeting on 16-18 January 2018 Chair: Bruno Sepodes – Vice-Chair: Lesley Greene 16 January 2018, 09:00-19:30, room 2F 17 January 2018, 08:30-19:30, room 2F 18 January 2018, 08:30-18:30, room 2F Health and safety information In accordance with the Agency’s health and safety policy, delegates are to be briefed on health, safety and emergency information and procedures prior to the start of the meeting. Disclaimers Some of the information contained in this agenda is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the COMP meeting reports once the procedures are finalised. Of note, this agenda is a working document primarily designed for COMP members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the agenda cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on- going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). -

Belinostat Phase II Trial Initiated in Platinum-Resistant Ovarian Cancer by the Gynecologic Oncology Group (GOG) Supported by the National Cancer Institute (US)
To NASDAQ OMX Copenhagen A/S TopoTarget A/S Announcement No. 01-10 / Copenhagen, January 6 2010 Symbion Fruebjergvej 3 DK 2100 Copenhagen Denmark Tel: +45 39 17 83 92 Fax: +45 39 17 94 92 CVR-nr: 25695771 www.topotarget.com Belinostat phase II trial initiated in platinum-resistant ovarian cancer by the Gynecologic Oncology Group (GOG) supported by the National Cancer Institute (US) Copenhagen, Denmark – January 6, 2010 – TopoTarget A/S (OMX: TOPO) announced today that GOG (The Gynecologic Oncology Group, US) has initiated a phase II trial evaluating efficacy and safety of belinostat and carboplatin in the treatment of recurrent or persistent platinum-resistant ovarian, fallopian tube or peritoneal cancer. GOG receives support for this trial from the National Cancer Institute (NCI) of the National Institutes of Health (NIH). “Positive efficacy and safety data with belinostat and carboplatin and paclitaxel (BelCaP) in patients with platinum resistant ovarian cancer have previously been announced by TopoTarget. We are very pleased that GOG now initiates this phase II study with belinostat and carboplatin (BelCar) in this difficult to treat patient population. Platin-resistance is a huge unsolved clinical problem in relapsing ovarian cancer and hopefully GOG will be able to show that BelCar, without additional paclitaxel is active in the platinum resistant setting.” said MD., Professor Peter Buhl Jensen, CEO of TopoTarget “ if GOG is able to repeat our initial positive results in platinum resistant patients we hope to advance into pivotal trials.” The study A Phase II evaluation of belinostat and carboplatin in the treatment of recurrent or persistent platinum-resistant ovarian, fallopian tube, or primary peritoneal cancer. -

Clinical Study Report Belinostat Study Report No: PXD101-CLN-8/PXD101-040-EU
Topotarget A/S - Spectrum Pharmaceuticals, Inc. Module 5 Clinical Study Report Belinostat Study Report No: PXD101-CLN-8/PXD101-040-EU 2 SYNOPSIS NAME OF COMPANY: Individual Study Table (FOR NATIONAL AUTHORITY Topotarget A/S, CuraGen, and Spectrum Referring to Part of the USE ONLY) Pharmaceuticals, Inc. Dossier: NAME OF FINISHED PRODUCT: Belinostat Injection 50 mg/mL Volume: NAME OF ACTIVE INGREDIENT: Belinostat (PXD101) Page: TITLE OF STUDY: A Phase 1/2 Safety, Pharmacodynamic, and Pharmacokinetic Study of Intravenously Administered PXD101 Plus Carboplatin or Paclitaxel or Both in Patients with Advanced Solid Tumors INVESTIGATORS: Coordinating Investigator (Site 001): Dr. Ulrik Lassen, Department of Oncology, The Finsen Center, Copenhagen University Hospital, Copenhagen, DK. Principal Investigators: Site 002: Dr, Johann de Bono. Site 003: Dr. Robert John Jones. Site 004: Dr. Lisa Sengeløv. Site 101: Dr. Richard Penson. Site 102: Dr Don Dizon. Site 105: Dr. James Hoffman. Site 106: Dr. John Micha. Site 108: Dr. Neil Finkler. Site 109 Dr. Patricia Braly. Site 111: Dr. Paul Celano. STUDY CENTERS: Part A: The Phase 1 part (advanced tumor) was conducted at: • Site 001: The Finsen Center, Copenhagen University Hospital, DK • Site 002: The Royal Marsden NHS Trust, Cancer Research, UK • Site 101: Massachusetts General Hospital Cancer center, Boston, US Part B: The Phase 2 part, MTD expansion phase (ovarian cancer) was conducted at: • Site 001: The Finsen Center, Copenhagen University Hospital, DK • Site 002: The Royal Marsden NHS Trust, Cancer -

Pricing of Cancer Medicines and Its Impacts
ACCESS TO MEDICINES, VACCINES AND PHARMACEUTICALS TECHNICAL REPORT Pricing of cancer medicines and its impacts A comprehensive technical report for the World Health Assembly Resolution 70.12 Operative paragraph 2.9 on pricing approaches and their impacts on availability and affordability of medicines for the prevention and treatment of cancer TECHNICAL REPORT Pricing of cancer medicines and its impacts Pricing of cancer medicines and its impacts ISBN 978-92-4-151511-5 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. -

140703EN NDA Belinostat
FDA approval of Beleodaq™ (belinostat) Accelerated Approval of Topotarget’s Beleodaq™ for the treatment of patients with relapsed or refractory peripheral T-cell lymphoma Early Action follows Priority Review 5 weeks before PDUFA Date Trigger milestone payment of USD 25 million to Topotarget Beleodaq™ is expected to be available to patients in July 2014 and will be launched through Spectrum Pharmaceutical's existing oncology sales force The Orphan Oncology Innovator BioAlliance Pharma and Topotarget are merging to create Onxeo, following approval of both companies shareholders end of June 2014 Paris, July 3, 2014 – BioAlliance Pharma SA (Euronext Paris - BIO), an innovative Company specialized in the development of drugs in orphan oncology diseases, today announced that the U.S. Food and Drug Administration (FDA) has granted Topotarget Accelerated Approval of Beleodaq™ for the treatment of patients with relapsed or refractory peripheral T-cell lymphoma (R/R PTCL). This follows a Priority Review of the Beleodaq™ New Drug Application (NDA) and was an Early Approval action prior to the August 9, 2014 PDUFA (Prescription Drug User Fee Act) date. Beleodaq™ was granted marketing authorization under the FDA’s accelerated approval program, which allows conditional approval of a medicine for a life-threatening disease based on early evidence suggesting clinical benefit. The approval is based on results from the BELIEF study, which enrolled 129 PTCL patients refractory to or who had failed at least one prior systemic therapy. A milestone cash payment of USD 25 million from Spectrum Pharmaceuticals is triggered by the NDA approval. A double-digit royalties as well as sales milestones of the aggregated net sales will be received by the company. -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -

Topotarget A/S Rodman & Renshaw Annual Global Investment Conference 2013 Safe Harbor Statement
Topotarget A/S Rodman & Renshaw Annual Global Investment Conference 2013 Safe harbor statement This announcement may contain forward-looking statements, including statements about Topotarget A/S’ expectations to the progression of Topotarget A/S’ clinical pipeline and with respect to cash burn guidance. Such statements are subject to risks and uncertainties of which many are outside the control of Topotarget A/S, and which could cause actual results to differ materially from those described. Topotarget A/S disclaims any intention or obligation to update or revise any forward-looking statements, whether as a result of new information, future events, or otherwise, unless required by Danish law. 2 Topotarget at a glance A Scandinavian-based biopharmaceutical company dedicated to develop and market cancer therapies • Situated in Copenhagen, Denmark with ~14 employees and a lean cost structure • Focused on the development and commercialization of belinostat, a molecular targeted cancer therapy NASDAQ OMX Listing Copenhagen 22% Symbol TOPO Denmark Switzerland 45% Market UK capitalization EUR 48 million Sweden (as of Aug 28, 2013) 20% ROW No. of shares 143,317,114 8% 4% 3 Building a strong commercial profile for belinostat Large sales potential in solid First registration filing tumors (CRC, bladder, expected Q4 2013 ovarian, NSCLC) Partnership with Spectrum Outstanding safety profile. Pharmaceuticals, Inc. Belinostat tested in more Pursuing partnerships in EU than 1,100 patients and Asia-Pac Belinostat – a pan-HDACi - Orphan indications (PTCL, -

Phenotype-Based Drug Screening Reveals Association Between Venetoclax Response and Differentiation Stage in Acute Myeloid Leukemia
Acute Myeloid Leukemia SUPPLEMENTARY APPENDIX Phenotype-based drug screening reveals association between venetoclax response and differentiation stage in acute myeloid leukemia Heikki Kuusanmäki, 1,2 Aino-Maija Leppä, 1 Petri Pölönen, 3 Mika Kontro, 2 Olli Dufva, 2 Debashish Deb, 1 Bhagwan Yadav, 2 Oscar Brück, 2 Ashwini Kumar, 1 Hele Everaus, 4 Bjørn T. Gjertsen, 5 Merja Heinäniemi, 3 Kimmo Porkka, 2 Satu Mustjoki 2,6 and Caroline A. Heckman 1 1Institute for Molecular Medicine Finland, Helsinki Institute of Life Science, University of Helsinki, Helsinki; 2Hematology Research Unit, Helsinki University Hospital Comprehensive Cancer Center, Helsinki; 3Institute of Biomedicine, School of Medicine, University of Eastern Finland, Kuopio, Finland; 4Department of Hematology and Oncology, University of Tartu, Tartu, Estonia; 5Centre for Cancer Biomarkers, De - partment of Clinical Science, University of Bergen, Bergen, Norway and 6Translational Immunology Research Program and Department of Clinical Chemistry and Hematology, University of Helsinki, Helsinki, Finland ©2020 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2018.214882 Received: December 17, 2018. Accepted: July 8, 2019. Pre-published: July 11, 2019. Correspondence: CAROLINE A. HECKMAN - [email protected] HEIKKI KUUSANMÄKI - [email protected] Supplemental Material Phenotype-based drug screening reveals an association between venetoclax response and differentiation stage in acute myeloid leukemia Authors: Heikki Kuusanmäki1, 2, Aino-Maija